Reconstruction of tendon losses
Abstract
This review discusses the latest literature-based evidence on reconstructive strategies following tendon losses, with a final focus on the innovative regenerative approach. Significant improvements in primary tendon repair techniques have radically reduced the failure rate and therefore decreased the use of reconstructive procedures. However, in specific conditions, such as crush injuries with loss of substance, avulsion injuries and inveterate injuries, the tendon gap cannot be repaired with a primary suture, making the procedure much more challenging for the surgeon. This article aims to guide the treatment of tendon losses, which is still a complex topic in hand surgery.
Keywords
INTRODUCTION
Tendon injuries are a frequently encountered and commonly treated condition in our hospitals.
Despite that, tendon losses may occur concurrently with other peculiar circumstances, such as accidental events, timing and previous failures. In this article, three topics will be discussed: flexor tendon losses, extensor tendon losses, and the regenerative surgery approach. This analysis will be principally supported by the evidence of the latest literature.
RECONSTRUSTRUCTION OF FLEXOR TENDON DEFECTS
Significant improvements in primary flexor tendon repair and postoperative rehabilitation have radically reduced the need for tendon reconstruction in the last few decades[1-3].
In the past, flexor tendon injuries in zone II, also known as “no man’s land” because of its complex and uncertain treatment, were repaired with a tendon graft as the primary reconstruction method. Currently, tendon reconstruction is reserved for inveterate injuries, primary repair failures and exceptional cases characterized by considerable loss of substance, as it may happen in crush injuries or following exposed fractures[2,4,5].
The purpose of this section is to describe current concepts on flexor tendon reconstruction, which remains one of the most challenging topics in hand surgery despite significant surgical and rehabilitative improvements.
Diagnosis and preoperative evaluation
The diagnosis of flexor tendon injury is based on the patient’s medical history and a thorough clinical evaluation; then, a standard radiographic investigation allows the exclusion of any associated bone lesions. Second-level imaging is usually not necessary.
Through clinical evaluation, potential signs of tendon injury such as loss of the digital flexor cascade, loss of tone, or loss of active flexion of the joint to which the tendon under examination is deputed should be investigated. Careful preoperative evaluation of the site of injury, any neurovascular injury, flexor digitorum superficialis (FDS) integrity or adhesion formation, pulley rupture, and joint contracture will permit the establishment of the most appropriate surgical strategy. The Boyes preoperative classification, whose increasing grade is associated with worse prognostic significance[6] [Table 1], is helpful in this context.
Boyes Preoperative Classification of Tendon Injury
| Grade | Conditions | Description |
| Grade I | Good | Minimal scar, mobile joints |
| Grade II | Cicatrix | Significant scar damage due to previous surgery or infections |
| Grade III | Joint damage | Joint damage, decreased range of motion |
| Grade IV | Nerve damage | Digital nerve injury |
| Grade V | Multiple system injury | Combination of II, III, IV |
Indications
The guidelines for defining the surgical technique to be used in cases of flexor tendon reconstruction are not standardized, and a gold standard has not yet been established[7].
As mentioned before, a careful clinical evaluation should be assessed preoperatively: surgical reconstruction should be avoided in patients with fixed contractures, joint disruption, hypovascularized fingers, or severe sensory disturbances[7,8].
A single-stage tendon grafting reconstruction may be indicated in patients with delayed presentation and significant tendon retraction or in patients with loss of tendon substance, who nevertheless still present poor scar adhesions, good preoperative Range of Motion (ROM), favorable neurovascular condition and intact tendon sheath.
In case of delayed primary repair, up to 30 days after injury, if tendon shortening causes flexion contracture and excessive tension force at the suture, 2-3 cm of additional length can be obtained by performing lengthening at the myotendinous junction, as described by Le Viet[9].
A two-stage tendon grafting reconstruction is recommended in conditions with a high risk of graft adhesion in a compromised tendon sheath and/or an insufficient pulley system. Using a silicone rod in the first surgical stage will create a new pseudosheath to allow free gliding of the tendon graft.
A vascularized flexor tendon transfer is a highly complex procedure that requires the sacrifice of the ulnar artery. This technique should only be performed by experienced surgeons in extremely selected cases involving injuries classified between Boyes’ Grades 3 and 5.
Injuries with a worse prognosis include crush trauma, significant soft tissue loss, joint fractures, or associated neurovascular damage. Young age is often associated with a better prognosis; however, it is important to remember that if rehabilitation is too intense, it may compromise a patient's compliance.
An additional therapeutic alternative described in literature is the tendon prosthesis, which can also be used as a permanent implant in patients with a poor prognosis[10].
Regardless of the surgical choice, it is crucial for the patient to be compliant to undertake intensive rehabilitation therapy to reduce soft tissue contractures and maintain flexible joints before and after surgery[11].
Single-stage reconstruction
This reconstruction involves replacing the missed or damaged tendon segment with a free tendon graft. Until the 1970s, single-stage reconstruction was commonly performed for acute tendon classes in zone II because of the high failure rate of direct repair. Today, due to improvements in primary repair, this surgical approach is almost dismissed[12,13].
In cases of tendon gaps, different types of tendon grafts can be used. The availability and desired length of the graft should always be evaluated before harvesting. The palmaris longus is the most commonly used tendon graft due to its easy accessibility, good quality, and low morbidity at the harvest site. Several clinical studies have shown its effectiveness in reconstructive use[1,2,4,5,14]. If long palmar is not present in the involved arm, the plantaris tendon may serve as an alternative. This graft is of considerable length, allowing it to extend from the digital apex to the forearm. However, it is often insubstantial, and preoperative ultrasonography can prevent unnecessary donor site mobility. Extensor tendons of II-III-IV toes can also be utilized, especially if a multi-toe graft is needed. In case of small gaps instead, the proper extensor tendons of the II and V fingers can also be used[4,15]. It has been observed that intrasynovial grafts, such as FDS and toe flexors, have better morphological and functional characteristics than extrasynovial grafts, creating fewer adhesions during tendon healing. However, the intrasynovial component of the toe flexors is generally too short to bridge the entire tendon gap[2,16,17].
Another potential graft is the long toe extensor tendon, the harvesting of which, however, may be difficult due to the presence of the extensor retinacula and may result in donor site weakness[18].
Traditionally, the graft is first fixed distally, either at the level of the residual flexor digitorum profundus (FDP) stump or at the distal phalanx. Proper tensioning must be established and connected to the proximal stump with a Pulvertaft suture. There are different fixation methods to the distal phalanx; after performing the core suture with Prolene or FiberWire (diameter 3-0) in the graft, this is either stabilized by pull-out technique, or fixed by suture anchor, which can be bioabsorbable or metallic; this reduces the risk of autolysis associated with the former. Pull-out fixation techniques are preferred in elderly patients or in those with poor bone quality[19,20].
Two-stage reconstruction
When the flexor tendon sheath is highly compromised and the pulley system is no longer valid, a two-stage flexor tendon reconstruction is recommended. Introducing a tendon graft into an injured flexor tendon sheath carries a significant risk of adhesions and postoperative stiffness[4,21].
The original technique introduced by Hunter and Salisbury involves the insertion of a silicone rod into the tendon sheath that induces the formation of a lubricated pseudomembrane coated with mesothelial cells that later allows tendon gliding within it[22,23]. The implant can have different lengths and can extend from the distal phalanx to the palm or the forearm. The diameter of the silicone rod should also be chosen considering the expected size of the intended tendon graft; generally, a diameter of 3 mm is indicated for a palmaris longus. The implant should not be too tight to ensure gliding[8]. The rod should be attached distally to the residual FDP or secured to the distal phalanx (i.e., with a pull-out technique)[16,24,25]. After a waiting period of 2-3 months, the second surgical time involves filling the new pseudosheath with the tendon graft[24,26]. According to some authors, however, this technique included two critical points: the simultaneous healing of the proximal and distal tenorrhaphy of the graft and the inability to predict the graft size during the first surgical time[24].
Subsequently, the Paneva-Holevich technique was developed, adding tenorrhaphy at the palm level between the distal stumps of FDP and FDS during the first surgical time. The tendon suture can be performed according to Kessler or with a fish mouth suture. After 2 to 3 months, the FDS will be released at its tendon muscle junction, creating a new elongated FDP following the now-healed tenorrhaphy. The new FDP will cross the carpal tunnel, palm, and flexor sheath until it is anchored distally[25,27,28].
Kessler later provided further development of these techniques, which is the result of the combination of the two previously described [Figure 1]. In the first stage, the anastomosis between the FDP and FDS is performed concurrently with the insertion of the silicone rod. Subsequently, the second stage will be similar to the technique described by Paneva-Holevich, even though it includes the removal of the implant and the passage of the graft into the pseudosheath[21,29]. In order to avoid excessive adhesion formation, effective tenolysis of the FDP extended to the carpal tunnel is strongly recommended to achieve complete intra-operatively mobility and a better postoperative outcome. The graft is commonly anchored to the silicone rod distal extremity, which is pulled out by dragging the tendon graft into the new pseudosheath. The pedicle graft will be stabilized distally by pull-out technique or suture anchors[21,30]. Proper suture tensioning and tightness will be assessed by the harmonic aspect of the digital cascade, the “squeeze test,” or by active flexion-extension of the patient in case of surgery under Wide-Awake Local Anesthesia (WALANT)[30]. The modified Paneva-Holevich technique has two advantages: first, the anastomosis between the FDS and FDP at the second stage is almost healed; second, during the first stage, it is possible to choose the appropriate size of the silicon rod. Therefore, this technique significantly improves on the previous ones[24].
Figure 1. Representation of a two-stage reconstruction according to the modified Paneva-Holevich technique. The figure on the left illustrates the anastomotic loop between the FDS (blue) and FDP (red) at the palm level. The figure on the right shows the new elongated FDP formed by the union with the FDS. FDS: flexor digitorum superficialis.
Vascularized flexor tendon transfer
Guimberteau et al. proposed a one-staged reconstructive technique for Boyes’ Grades 3-4-5[31]. They consider the peritendinous connective tissue and the paratenon as a single operative unit with the flexor tendons. These structures would provide an adequate blood supply and a gliding sheath that ensures the optimal function of the tendon itself. This technique is based on retrograde flow through the ulnar artery and involves the use of the FDS of the fourth finger to fill defects between 18-20 cm. Preoperatively, it is necessary to ensure the effectiveness of the radial artery with Allen's test and a Doppler test. The technique involves careful dissection of the ulnar artery proximal to Guyon's canal; at that level, the anterolateral branches of the artery are identified and will vascularize the flap. Although Guimberteau et al. obtained better results with this technique if compared to more traditional ones, they acknowledged that, considering its high complexity, it should be limited to a small number of patients and performed by experienced surgeons. Cavadas et al. reviewed 40 flexor tendon reconstructions (four flexor pollicis longus and 36 finger flexors) with vascularized FDS tendon grafts, including 37 pedicled flaps and three free flaps. The authors reported a postoperative total active range of motion of 178.05° (SD 50)[32].
Currently, the available studies concerning this technique are limited, and the indications are not fully clarified.
Pulleys Reconstruction
The pulley system optimizes the action of the flexor tendons, keeping the tendon close to the phalanges; furthermore, it converts tendon gliding into joint excursion[33]. Damage to the pulleys results in tendon bowstringing, which reduces the effectiveness of active flexion and requires more muscle effort[34,35]. Preservation of the original pulleys is always more advisable than reconstruction and it may allow a single-stage procedure. In particular, even though preservation or reconstruction of A2 and A4 pulleys is recommended[36,37], it has currently been shown that the A4 pulley can be sacrificed during acute tendon repair if A2 pulley is safe. However, it has not yet been clarified whether the same concept is applicable in the reconstructive setting[38]. Several reconstructive techniques involve the use of the damaged tendon, a tendon graft, or the extensor retinaculum. These techniques involve creating a loop around the phalanx or pulling the graft through remnants of the pulleys. The technique, according to Klinert/Weilby, creates a weave of the tendon graft over the edges of the native pulley[39]. The tendon graft can also be intrasynovial, thus involving the use of a slip of FDS or extensors retinaculum; according to some authors, this would improve tendon glide[40,41]. Another procedure is the "belt-loop" technique described by Karev, according to which the graft constituting the pulley passes through a tunnel in the volar plate[42]. In addition, several techniques for pulley reconstruction are based on creating a loop around the phalanx: while Lister envisions a single loop using the extensor retinaculum, Okutsu describes the triple-loop technique (preferred by the author) and Widstrom the loop-and-a-half technique[43-45]. Reconstruction, according to Lister, seems to lead to better tendon gliding, perhaps because of the intrasynovial graft[36]. On the other hand, the techniques involving loops around the bone appear to be the strongest, particularly the one outlined by Okutsu, which is recommended in A2 pulley reconstruction[46] [Figures 2 and 3].
Figure 2. Two pulley reconstructive techniques are shown. On the left, there is Okutsu’s triple-loop reconstruction; on the right, you can observe Klinert and Weilby’s bone encircling. The tendon graft used for pulley reconstruction is shown in green.
Outcomes and complications
The goal of flexor tendon reconstruction is to restore function with good recovery of flexion-extension; however, the results are often poor compared to primary repair. There is no standardized evaluation system, but several have been described: total active motion (TAM), strength assessment, Stickland's or Schneider's modified grading system[1,2,7,47]. Heterogeneous results have been reported in the literature; using intrasynovial grafts and early active mobilization, Leversedge describes 64% and 55% active ROM recovery for single-stage and double-stage reconstructions, respectively. Better results with 73% active ROM recovery have been described for single-finger reconstructions[2]. In contrast, Coyle et al. achieved 91% active motion recovery with a double-stage technique; however, they confronted a 9% rupture rate and the need for secondary tenolysis at 6%[3]. Karakaplan et al., after a two-staged reconstruction of flexor tendon injuries in Zone II in 10 patients, reported good to excellent results in 60% of the cases. They also recorded one case of tenolysis. The most frequent complication following tendon reconstruction is adhesion formation: in particular, the relevant literature reports a rate of adhesions from 12% to 47%[1,48,49]. For this reason, an appropriate postoperative protocol is essential. Rehabilitation should promote graft gliding, thus preventing adhesion formation and loss of function. There is no standardized rehabilitation protocol; reportedly, the splint may be removed after a period of 5 days to 5 weeks[24]. Early active mobilization has been shown to promote healing by inducing collagen type III production and reducing adhesion formation[50-52]. Adhesion formation may result in the need for subsequent tenolysis; however, at least six months of intensive rehabilitation are recommended before secondary surgery[30]. A poor surgical technique or excessive mobilization can result in tendon repair rupture; this occurs in 3% to 9% of patients, and the greatest risk is recorded 10-12 days after surgery[53]. Rupture can occur on the proximal or distal side of the suture, and sometimes it can occur intra-substance. A primary repair can be performed if this adverse event occurs in the first few weeks after the repair; otherwise, if the soft tissue condition does not allow it, the procedure can be converted to a two-staged procedure. If the rupture involves only the FDP and the FDS is intact, an arthrodesis of the distal interphalangeal joint or a tenodesis of the FDP on the FDS can be performed[30,54]. Joint contractures in flexion, particularly at the PIP, are a frequent complication that can occur in up to 40% of reconstructions. In these cases, a surgical release of the joint may be indicated when physical therapy fails[30,55]. Excessive tensioning or extreme shortness of the graft can result in a quadriga effect with reduced proper motility of adjacent fingers. The most affected by this complication are III-IV and V fingers, which can tolerate an advancement of up to 1 cm. Instead, an extremely loose graft tension or its excessive length can result in lumbrical plus deformities. The latter consists of the paradoxical extension of the finger when the attempt is to flex it; this is caused by premature contracture of the lumbrical muscles before the FDP can flex the DIP[56].
An uncommon complication is silicone rod synovitis, which leads to a poor outcome because it impairs the proper gliding canal formation[1,21]. Implant infection is also described: it requires implant removal and antibiotic therapy, and results in delayed reconstruction[55].
The use of WALANT is increasing in hand surgery and tendon repair. Local anesthesia offers significant advantages in this setting: the possibility of intraoperative mobilization allows simultaneous assessment of tendon gliding, graft tension, and suture strength[57,58].
RECONSTRUCTION OF EXTENSOR TENDON DEFECTS
The extensor tendons run close to the skin on the dorsal aspect of the hand, lying in a very superficial position, which makes them particularly prone to injury. Laceration, avulsion and crush are common trauma dynamics[59,60].
Whereas simple lacerations could be repaired with direct tendon suture, avulsion and crush injuries may result in tendon gaps and defects, becoming more challenging to repair[61,62].
Due to the different degrees of possible excursion of the extensor and flexor tendon systems in hand, the tendon defects in the extensors must be managed carefully[63]. Compared to flexor tendons, whose mobilization, thanks to a moderate excursion degree, can bridge gaps up to 1 centimeter, extensor tendons have less excursion, especially in Verdan’s zones from 1 to 5[64]. Indeed, even a 1-millimeter extensor tendon elongation in zone 1-5 might lead to a 20° extension lag; on the other hand, even a 1-millimeter extensor tendon shortening in zone 1-5 may cause decreased finger flexion[62].
Primary tendon suture is the optimal surgical technique, but when it is not possible, different surgical procedures could be employed, namely tendon lengthening, tendon grafts, and tendon transfers[65].
The appropriate reconstructive procedure varies according to the injury location, due to the unique properties of the extensor tendons in each different Verdan’s zone[61,66]. For example, in the wrist and forearm, extensor tendons are tubular rope-like structures with a morphology comparable to that of flexor tendons, but going distally, they transform into paper-thin, almost translucent, flat structures[63]. Accordingly, the classification of the zones of injury (Verdan’s classification) is of high clinical relevance, as it permits delineating the subsequent different treatment approaches[59].
The purpose of this section is to describe current concepts on extensor tendon reconstruction techniques.
Diagnosis and preoperative evaluation
The assessment of extensor tendon injury is based on the patient's medical history and clinical evaluation[66,67]. Radiographs are routinely performed in order to detect potential concomitant bone or joint injury, such as fractures or bony avulsion of the tendon. Second-level imaging is usually not necessary. Moreover, it is necessary to rule out any concurrent neurovascular damage.
On the physical examination, attention should be paid to any abnormal cascade of fingers and wrist. Elson’s test helps in the evaluation of the integrity of the central slip[68]. This test is based on the assumption that full distal interphalangeal (DIP) extension is not physiologically achievable with the finger flexed at the proximal interphalangeal (PIP) joint, because of loose lateral bands. Lacerations of the central slip cause the lateral bands to tighten and migrate towards the pivot axis of the PIP joint while the central slip slightly retracts. During the examination, the patient’s PIP joint is flexed to 90 degrees. A central slip injury is evidenced by the patient’s ability to extend or even hyperextend the corresponding DIP joint[68-70].
If a tendon graft is required during the surgical procedure, the existence of the palmaris longus (PL) should be checked preoperatively. Patients should oppose their thumb and small finger to test for the presence of the PL; this structure is absent in 15% to 25% of people[71].
Surgical techniques
If the extensor tendon primary repair is not possible due to tendon loss, a number of procedures have been developed to repair the extensor system. Particularly, the main surgical techniques employed are tendon lengthening, tendon graft, and tendon transfer[61,66,67,72].
Lengthening of the tendon may be done to achieve additional length in a small to moderate extensor tendon gap, especially in more proximal lacerations where the extensor tendons have more thickness[58,66]. The modified Baker technique (U-T plasty) and Z-plasties are recommended because of their simple technique, favorable biomechanical characteristics, and early rehabilitation[73].
There are also reconstructive techniques for chronic lesions of the extensor pollicis longus (EPL). One example is the L-lengthening local tendon flap described by Lobo-Escolar et al., which avoids the use of tendon graft or tendon transfer[74].
Another extensor tendon reconstructive option is the use of local or distant tendon flaps. Both these techniques are anatomically feasible and technically quick to perform, but local tendon flap harvesting avoids distant donor site morbidity and provides morphologically similar donor tendon that is readily accessible[72,75].
When local procedures cannot adequately resolve significant tendon gaps, tendon grafting offers a relevant surgical solution[76,77]. The palmaris longus (PL) or strip of the flexor carpi radialis (FCR) are useful as donors for small defects, whereas the plantaris tendon is suitable for large gaps or when multiple grafts are required[71]. Other examples include extensor digitorum longus of the middle and small toe, extensor proprius indicis, extensor digiti minimi, abductor pollicis longus and accessory abductor pollicis longus tendons[59].
In cases of multiple finger injury, if one finger requires amputation or joint fusion, tendon grafts could be harvested from this finger and employed to reconstruct tendon gaps in another finger[78].
Adequate tendon length is crucial for a functional outcome. When placing the tendon graft, care must be given to determine the graft length to reconstruct the extension mechanism and ensure complete flexion in wrist and hand joints[72].
The suture technique introduced by Pulvertaft in 1956 is one of the most reliable suturing methods for joining the tendon ends[77].
The maintenance of the anatomic axis of tendon function and the minimal donor site morbidity are two of the main benefits of tendon grafts with respect to tendon transfers[79].
In cases of extensive trauma of the dorsum of the hand with severe soft tissue damage, previous surgical approaches may not be sufficient to guarantee a functional clinical outcome. Usually, these large defect treatments require both stable skin replacement and tendon repair, using microsurgical reconstruction, in a single-stage procedure or, more frequently, in a multiple-stage procedure[59,66]. Fasciocutaneous flaps and free-functioning muscle transfer, with or without the application of silicon rods and followed by delayed tendons transfers graft, as well as free composite tissue flap (tendons and soft tissue flap, especially from the lower extremity, e.g., dorsalis pedis flap with extensor tendons of the toes) can help to re-establish hand function[62,80-82].
The single-stage reconstruction is the result of all the attempts made to reduce the number of surgical procedures and the time of recovery[81]. Furthermore, some authors stated that the use of vascularized tendon grafts leads to faster recovery and reduces adhesion formation, because the tendons are transferred with their vascularity and their surrounding tissue containing the tendon sheath[66,81].
However, due to the considerable donor site morbidity and the debatable actual advantages of a vascularized tendon graft, less-invasive techniques are recommended. Therefore, it is preferable to opt for a thin free flap allowing for sufficient gliding in combination with an avascularized tendon graft[59].
Another reconstructive option to overcome extensor tendon defects is tendon allograft. Some authors found that allograft is a safe procedure and its outcomes are very similar to those related to tendon autograft[59,83].
Tendon transfer is an option to substitute the function of injured tendon when reconstruction is not possible (e.g., large extensor gaps, such as those resulting from severe forearm trauma, or extensor muscle paralysis from a radial nerve injury)[79,84-86]. This technique plays a key role even in the reconstruction of extensor pollicis longus (EPL) tendon, both after subcutaneous injuries and large loss of tendon substance[72]. In order to achieve satisfactory outcomes, a tendon transfer must respect several principles:
● the donor muscle must be able to sufficiently move the recipient tendon;
● the recipient and donor muscles’ tendon degree of excursions must be comparable;
● the donor muscles must work in phase with the recipient one[72].
Any of these various surgical techniques could be employed in restoring the extensor tendon system, with different indications according to Verdan’s zone of injury[59,72,87].
Zone 1
An extensor tendon gap in zone 1 can develop both after a traumatic injury and after a chronic mallet finger repair with the removal of scar tissue[59,86]. Based on the size of the tendon defect, different reconstruction techniques might be chosen[59,88].
Regarding local tendon flaps, the terminal tendon hemilateral band technique might be useful to address tendon gaps of about 1 centimeter. This procedure uses the lateral bands of the injured finger to bridge the extensor tendon gap and reconstruct a new terminal slip. Particularly, after wound exploration and tendon gap measurement, L-shaped cuts are performed in the lateral bands in accordance with the size of the defect. The cut bands are then flipped over to the distal portion of the gap and both the distal and proximal portions of the bands are sutured[89]. This procedure may require temporary arthrodesis of distal interphalangeal (DIP) joints for 4-6 weeks[59,89]. Attention must be paid to leaving an adequate amount of lateral band to prevent loss of intrinsic activity[89].
Interposition tendon grafting necessitates tendon harvesting to reconstruct the extensor defect and provides the repair of tendon gaps over 1 centimeter. Palmaris longus (PL) tendon is the most commonly employed in zone 1 reconstruction[59,63]. Various techniques have been described to provide the attachment of the harvested tendon to the distal phalanx, including the possibility of creating a drill hole in the distal phalanx, in which the surgeon can insert the PL tendon and secure it with a knot[90]. The interposition of a tendon graft requires postoperatively immobilization (usually 4 weeks)[91].
Composite venous flap and palmaris longus (PL) tendon might be useful to reconstruct soft tissue defects along with tendon loss. This technique requires microsurgical reconstruction, arterializing one vein of the flap with an anastomosis with the digital artery and connecting another vein with the finger venous system[92,93].
Zone 2
The management of zone 2 extensor tendon defects employs the same technique described in relation to zone 1, considering particularly local tendon flap and interposition tendon graft (palmaris longus tendon)[1].
Regarding local tendon flap, the defect is bridged with a tendon graft harvested from the proximal portions of the extensor tendon and flipped distally to fill the gap [Figure 4][64].
Zone 3
Due to the unique anatomy of the extensor tendon in zone 3 and the different structures that could be involved, various reconstructive procedures could be performed[66,70].
If the lateral bands are intact, they may be divided longitudinally, centered over the proximal interphalangeal (PIP) joint and sutured to each other[59]. If the proximal portion of the extensor tendon is intact, a distally based tendon flap may be harvested from this tendon portion and flipped over distally to overcome the gap [Figures 5 and 6][94].
If the lateral bands and the proximal portion of the extensor tendon are damaged, interposition tendon grafting or, in case of associated soft tissue injuries, composite tissue grafting should be considered[59,61].
Zone 3 extensor tendon defects should be managed carefully, proposing a reconstruction that manages to overcome the gap as well as to prevent the development of boutonnière deformity[59].
Zone 4
Since in zone 4, extensor tendons gradually show more girth than in the previous zones, tendon gap restoration may be more simple[59,61,72]. Again, two main reconstructive methods should be taken into consideration: local tendon flaps and interpositional tendon reconstructions[72].
Zone 5
Compared to zone 4, the treatment of defects in zone 5 also includes the use of tendon lengthening techniques[75].
Zone 6, 7 and 8
The extensor tendons in zone 6-8 are characterized by a parallel course and a greater degree of excursion. In cases of single extensor tendon defect, with adjacent tendons in continuity, a straightforward method to overcome the gap is to suture the injured tendon to a close tendon using a side-to-side suture. However, this new pattern is biomechanically inefficient, altering the alignment of tendons and creating overloading on the donor tendon; this might lead to early tendon ruptures[95,96]. Accordingly, even in zone 6-8, tendon lengthening procedures and interposition tendon grafts should be considered when planning the reconstruction[73]. Among tendon lengthening procedures, Cerovac and Miranda described the tendon turnover technique, where the tendon ends are L-shaped cut and flipped over to reconstruct the gap[75]. Another surgical option suitable for significant tissue and tendon loss is the two-stage extensor tendon reconstruction employing a silicone rod[65,83,97].
For zone 1-5 reconstructions, the finger is typically immobilized in extension for 4 to 6 weeks, sometimes performing a K-wire temporary arthrodesis of the interphalangeal joint. On the other hand, for zone 6-8 reconstructions, early passive and active motion could be permitted[59,98].
Sagittal bands reconstruction
The sagittal bands (SBs) at the metacarpophalangeal (MC) joints act as the primary lateral stabilizers of the extensor tendons. Although trauma is the most frequent cause, congenital, inflammatory, or degenerative processes can also lead to extensor tendon subluxation[99].
In order to center the extensor digitorum communis (EDC) tendon over the MC joint and regain strength with range of motion, several techniques have been described and advocated in the literature. In the case of acute injuries, conservative treatment with Yoke splint and immediate controlled active motion (ICAM) can be effective. The surgical treatment options depend on the local tissue quality: if the sufficient quality of the injured tissue remains, direct repair with realignment is possible, but if there is a sagittal band loss of substance, various forms of reconstruction should be considered[99-101]. The main reconstructive options include flaps from extensor tendon (e.g., rotational tendon flap inserted to the adjacent finger volar plate as an anchor site), the use of juncturae tendinum to lengthen the EDC tendon graft[46], and palmaris longus tendon graft[99].
Complications
Peritendinous adhesions that form after extensor tendon repair and reconstruction remain a difficult issue. Numerous materials have been used in order to limit adhesions, but without reproducible results and real success. Tenolysis may ultimately be required if the functional range of motion is not obtained, even though it should not occur before 6 months postoperatively. The patient candidate for tenolysis should be willing to access therapy and should show these features: failed nonsurgical management for at least 6 months, full passive range of motion, pliable and well-healed skin without strong scar tissue, and uninvolved joint surfaces[63].
Arthrodesis is a feasible option for patients suffering from pain and dysfunction after failed extensor tendon repair and/or revision in zones 1 and 3. Fusion of the joint at this level can be a reliable method to eliminate pain while maintaining some level of function[63,102].
Outcomes
To measure clinical outcome and patient satisfaction, Nakamura and Katsuki suggested the use of the pulp-to-palm distance, patient satisfaction (based on the visual analog scale, VAS) and the metacarpophalangeal (MP) joint extension lag. They found that patient satisfaction is related to the pulp-to-palm distance, but not to the MP joint extension lag[76].
In early 1980, Shannon and Barton suggested that the outcome of tendon transfer for finger extensor tendon ruptures was often poor[103]. Indeed, further studies reported satisfactory results for tendon graft; Bora and Minami described optimal functional outcomes for tendon graft, particularly using palmaris longus to reconstruct extensor tendon defects[104,105]. Moore reported that the clinical outcome is minimal when there are multiple extensor tendon deficiencies, but good results could be achieved with tendon transfers if only one extensor tendon is injured[106].
Chung compared clinical outcomes after tendon grafts and tendon transfers, finding no difference in functional results between the procedures[84] [Table 2].
Comparison of patient characteristics between the tendon transfer and tendon graft groups
| Variable | Tendon transfer | Tendon graft | P-value | ||
| Median | SD | Median | SD | ||
| Age (years) | 46.3 | 8.3 | 46.2 | 8.2 | 0.40 |
| RA duration (years) | 11.2 | 2.8 | 11.4 | 2.4 | 0.36 |
| Time from rupture to surgery(weeks) | 12.8 | 9.4 | 13.7 | 9.2 | 0.11 |
| Follow-up (years) | 16.0 | 5.1 | 13.9 | 3.3 | 0.10 |
| Extension lag (°) | 8.9 | 9.0 | 8.2 | 12.0 | 0.84 |
| Range of motion (°) | 71.1 | 17.9 | 77.3 | 17.0 | 0.12 |
| Pulp-to-palm distance (cm) | 0.3 | 0.4 | 0.4 | 0.7 | 0.51 |
| Geldmacher score | 20.9 | 3.9 | 20.7 | 3.7 | 0.48 |
| Overall satisfaction rate | 84.5 | 8.2 | 87.2 | 8.3 | 0.19 |
Minami et al. reported good functional results using tendon graft after 1987, before which they had poor results caused by flexion deficit after end-to-side repair with an adjacent tendon[107]. In contrast, Nakamura and Katsuki[76] suggested that tendon grafting is unsatisfactory because finger flexion may be restricted as a consequence of irreversible muscle contracture.
Tendon transfer is the most common surgical treatment for extensor tendon rupture. Shannon and Barton[103] suggested that the outcome of tendon transfer for finger extensor tendon ruptures is often poor. Moore et al. reported that patients with a single extensor tendon rupture have good results after tendon transfer, but that tendon transfer for three or more ruptured tendons associated with MP arthritis often requires salvage procedures[106].
The duration of the untreated rupture is often long because rheumatoid patients are accustomed to performing daily activities with a deformed hand (Nalebuff, 1987)[108]. If joint destruction is apparent in the MP joint or if multiple fingers are involved, the clinical result is poor and inversely proportional to the duration of an untreated tendon rupture (Moore et al., 1987; Shannon and Barton, 1976)[103,106]. The patient had a better outcome when one or two fingers were involved than when three fingers were involved, and the duration of untreated rupture was related to the MP joint extension lag. Nakamura and Katsuki[76] suggested that the pulp-to-palm distance (a clinical outcome) and patient satisfaction (measured on the visual analog scale) are related but that the MP joint extension lag and the patient satisfaction are not related.
REGENERATIVE SURGERY APPROACH TO TENDON DEFECTS
Regenerative medicine is a branch of translational research based on the clinical application of cell therapy, promoting and stimulating the body's own repair mechanisms to achieve healing with complete morphological and functional recovery in the absence of scar tissue. Regenerative Surgery (RS) defines all the Regenerative Medicine treatments that can be clinically applied through minimally invasive surgical procedures.
The three pillars on which Regenerative Medicine is based and acts are the interaction and integration of 'stem' cells, growth factors and scaffolds. When tissues get damaged, the most common body repairing response is represented by scarring activity, which produces nonfunctional tissue. To be more precise, the scar tissue possesses inferior mechanical and biochemical properties compared to native tissue[109], and this is particularly true for tendon healing. In fact, the tendon, due to its low cellularity and poor blood supply, has limited healing capacity; therefore, it is difficult to regain the original structure and function of the tendon after damage. This is also due to the fact that tendon healing, which is composed of the three classical phases of healing, namely the inflammatory phase, the proliferative phase and the remodeling phase, is extruded through two distinct processes, which are intrinsic and extrinsic healing[110,111]. The inflammatory phase is characterized by increased vascular permeability and the arrival of inflammatory cells such as neutrophils, macrophages, T-cells, and mast cells. It is well known how abnormal macrophage activity can cause fibrosis, and it has been shown that in macrophage-deprived tendons, there is decreased scar production attributed to lower levels of cytokine transforming growth factor (TGF)-β. In contrast, the proliferative phase is characterized by different fibroblast populations with mainly type III collagen production. In animal models, the healing process starts at the epitenon, and the cells move from the epitenon/paratenon into the injury area. The remodeling phase involves the transformation of granulation tissue into scar tissue with a reduction in vascularity and cellularity. Unlike other tissues, however, tendons cannot regenerate completely, and the scar is never wholly replaced. This reason could be due to the inability of the tendon tissue to transform the temporary scar rich in type III collagen into the original reticulated scar consisting of type I collagen[112]. Current surgical treatments, such as autografts, allografts, and tendon prostheses, are often required for tendon repair. However, these methods are limited owing to the high incidence of failure rate, donor site morbidity, inferior graft integration, and limited long term functional recovery[113,114]. For the patient, this results in functional deficits, which, due to the peculiar capabilities of the “hand organ”, lead to serious personal, social and economic problems associated with high welfare costs for society. Meanwhile, a real and effective regenerative process should ensure complete functional and morphologic restoration. Therefore, faced with the problem of reconstructing tendon defects, the approach of regenerative medicine will be, on the one hand, to promote tendon regeneration and, on the other hand, to provide a neo-tendon with similar characteristics to the native tendon that can bridge the gap. This goal can be achieved only through functional cell division and concomitant self-renewal and differentiation of mesenchymal stem cells[110,115]. From the review carried out, it emerges that, to date, there are no regenerative surgery techniques validated for clinical use in humans that are suitable for the treatment of tendon defects. However, the numerous pre-clinical studies show promising scientific advances that are likely to provide us with tools that can improve the biological and functional outcomes of tendon surgery in general, and of the treatment of tendon defects in particular, in just a few years.
The following are the most promising discoveries for each of the three fundamental pillars of regenerative medicine.
Cells
Cells that are widely used in tendon tissue engineering include tendon fibroblasts (tenocytes), dermal fibroblasts, and mesenchymal stem cells (MSC). Mesenchymal stem cells (MSCs), first described by A. Caplan in 1989, currently seem to be the best regenerative option in terms of cell population. This is primarily due to their unique potential in repairing damaged tissues and organs and their active regeneration, facilitated by their self-renewal and multi-lineage differentiation potential. Among different sources of MSCs, adipose tissue (AT) remains one of the most promising, valuable, and reliable sources of regenerative elements as adipose-derived stem cells (ADSCs), even if the tenogenic potential of bone marrow-derived stem cells (BMSCs) has been firstly and extensively studied[110,116-118]. Human ADSCs seeded onto a mesh derived from hyaluronan (Hyalonect) and placed under mechanical stress formed a vascularized tendon-like structure[119]. In vivo, from the pathophysiological point of view, there are different elements interfering with transplanted cell survival and local homeostasis. Factors that induce transplanted cell death are: host inflammatory response, shear and mechanical stress, the local activity of reactive oxygen species (ROS), hypoxia, and low nutrient supply. Conversely, pro-survival factors are mediated by extracellular membranous vesicles, better known as exosomes, containing mRNAs and signal molecules, able to mediate intercellular communication, generically called bioactive molecules[120].
Bioactive molecules and markers
Numerous growth factors have been shown to be active in both tendon development and healing. Little is known about the synergistic and antagonistic interactions of these growth factors, and likewise, there is a poor understanding of the optimal spatial and temporal distribution of growth factors that would produce the best effects. Because of that, the application of growth factors to clinical tendon repair remains challenging.
IGF-1 in a rat Achilles tendon model was able to mitigate inflammation-induced functional deficits[121].
TGF-β is involved in matrix synthesis in tendon healing, as demonstrated by a significant increase in collagen types I and III production in rabbit tendon cells with the addition of these TGF-β isoforms[122].
bFGF increases, in a dose-dependent way, proliferation and the expression of collagen type in a rat patellar tendon treated with bFGF[123].
Scleraxis (Scx) is expressed in both tendon progenitor cells and mature tenocytes. Scx binds tendon-specific element 2 (TSE2) to form the Scx/E47 heterodimer, which in turn activates the collagen type I promoter[124,125].
Growth differentiation factor 5 (GDF-5) has been reported to efficiently promote tenogenic differentiation in vitro. Haimi et al. achieved a rapid tenogenic extracellular matrix production of ASCs in vitro by the use of GDF-5. However, GDF-5-induced tenogenic differentiation has not yet been evaluated in animal models[126-129].
Connective tissue growth factor (CTGF) has been demonstrated to induce the differentiation of human MSCs cells into fibroblasts. This is demonstrated by the marked increase in type I collage and tenascin-C synthesis. Hence, CTGF may contribute to the preservation of the structural integrity of tendon tissue, and because of that, it could play a crucial role as a therapeutic agent in tendon regeneration[130,131].
Transforming growth factor beta (TGF-b) in a developing mouse limb model proved to be the most significant signaling pathway in differentiating tendon stem/progenitor cells (TSPCs) into tendon cells. In addition, Scx-GFP signaling, which gradually disappeared when TSPCs were cultured in vitro, was reported to reappear upon TGF-b treatment. These results demonstrated the central role of TGF-b in tendon induction[132,133].
Mechanical Stimulation
Among the bioactive molecules, Mechanical Stimulation (MS) holds a prominent position due to its well-known role in stimulating collagen production and cell differentiation in the tenocyte sense. After tendon injury and repair, it is well recognized that early and controlled mobilization during the recovery process is crucial to improving outcomes and mechanical properties of the healed tendon, although the optimal timing and loading are largely debated[52]. In animal models, the complete removal of load during the tendon’s healing results in inferior mechanical properties of the repaired tendon[134,135]. Conversely, increased loading and movement are also detrimental to tendon properties if implemented too quickly[135]. Increased cellular proliferation, collagen production, and tenogenic gene expression, as well as Scx upregulation, is found in both fibroblasts and mesenchymal stem cells when exposed to static or cyclic uniaxial tension[136].
Scaffolds
Scaffolds are another critical factor for tendon tissue regeneration. They provide biomechanical support and improve tendon healing by facilitating cell proliferation and differentiation, promoting matrix production through cellular hybridization, surface modification, growth factor attachment, and mechanical stimulation[137]. Because of that, the topographical cues provided by scaffolds must be carefully considered: for example, the micro-/nano-structure of material surfaces has been widely reported to modulate cellular behavior. Furthermore, tendon tissue is composed of parallel collagen fibers and the alignment is an important topographical characteristic to mimic in tendon tissue engineering. This was widely demonstrated by the experiments showing that tendon-specific markers, such as scleraxis and tenomodulin, were significantly increased on electrochemically aligned collagen (ELAC) threads compared to randomly oriented collagen fibers[138].
Three major categories of scaffolds are used:
(A) native tendon matrices; (B) synthetic polymers; (C) derivatives of naturally occurring proteins.
(A) Scaffolds derived from tendon matrices could retain both the normal biomechanical and biochemical properties, turning out to be the ideal biomaterial to support tendon healing. However, before it can be utilized, the native cells must be removed to prevent disease transmission and immune response[137].
(B) A great number of biodegradable and biocompatible polymers have been used for tendon tissue engineering as well. In particular, for their biodegradability and material characteristics, the α-hydroxy-polyesters including polyglycolic acid (PGA), poly-L-lactic acid (PLLA) and their copolymer polylactic-co-glycolic acid (PLGA) have been studied. Numerous experimental studies on animal models demonstrated the formation of mature collagen fibrils and cellular tenogenic differentiation using PGA or PLLA scaffolds seeded with MSCs derived cells[140]. Despite these advantages, polyester’s scaffolds suffer from several limitations, such as the absence of biochemical motifs for cellular attachment, or the inability to fully regulate cell activity[141].
(C) Scaffolds made from natural proteins.
Tendon ECMs are mainly composed of collagen type I and therefore scaffolds based on collagen derivatives are highly biocompatible. Collagen derivatives scaffolds, in contrast with polyester ones, demonstrate better bio-functionality by supporting cell adhesion and cell proliferation. The major disadvantage of collagen scaffolds relates to their poor mechanical properties and their relatively short in vivo life, due to progressive and natural enzymatic degradation, which further compromises their mechanical properties. Partial solutions to these problems have been achieved through their modification by cross-linking or co-fabricating with other materials to enhance mechanical strength and resistance[142]. Beyond collagen, scaffolds made from silk have been used in tendon tissue engineering. Tenogenesis of MSCs is enhanced when seeded on aligned silk fibroin electrospun fibers, as evidenced by the upregulation of expression of tendon/ligament-related proteins[143].
DISCUSSION
The new and more in-depth knowledge of biology and molecular biology linked to the development and healing of tendon tissue, coupled with the increasing scientific knowledge of the regenerative potential of mature cells and tissues, are bringing us ever closer to the goal of achieving tendon healing by regeneration after simple tendon trauma or loss of substance. However, unfortunately, to date the comparison between regeneration and scarring after a tendon injury is very unbalanced in favor of the latter, with its consequent negative consequences in terms of functional recovery, pain and return to a normal working and social life for the patient who has suffered the injury.
As analyzed above, there are already several studies in the literature documenting the regenerative success of cellular and molecular therapies with growth and differentiation factors in an animal model. To these experiences, we must then add the numerically inferior studies demonstrating the effectiveness of using bioengineered tendons in the treatment of loss of substance. These studies, which give us great hope for the near future, unfortunately, must be rightly confronted, in the transition to clinical trials, with the strict regulations present in highly industrially and economically developed nations and with the ethical rules imposed by scientific societies throughout the world[144].
Trying to condense the different legislative codes on regeneration, cell therapies and bioinduction present in the various nations, it can be asserted that they all more or less descend from the FDA's guidelines and regulatory framework.
In the majority of developed countries, the only therapies that are allowed in the clinical practice are cells or non- structural tissues-based therapies that do not cause relevant alteration of the biological characteristics of cells or tissues and preserve their original properties and functions, such as decantation, filtration, centrifugation, and mechanical disruption without relevant alteration. These methods are included in the definition of minimal-grade manipulation (MGM), by which tissues are harvested, treated, and reimplanted during the same surgical session and inside the same operating room. In this sense, for clinical application, the basket of regenerative options should be evaluated according to the principle of low or high cellular manipulation. Bearing this in mind, and mainly led by the need to fall within the legal parameters of the low manipulation rules, which in Europe stipulate that cells must be extracted at the patient's bedside in the operating theater without the use of enzymatic products, numerous medical devices have appeared on the market. Their intrinsic feature is the promise to obtain MSCs in compliance with these regulations in order to be able to perform primitive regenerative cell therapy.
At the same time, numerous clinical and pre-clinical scientific studies have appeared in the literature to independently validate the ability of these medical devices to provide adequate quantities of viable MSCs at the patient's bedside to be useful for clinical purposes. To date, these clinical purposes only aim to tip the scales of the healing process a little more in favor of regeneration and a little less in favor of healing, yet without providing the possibility of regenerating the injured tendon or using a histocompatible neo-tendon that is bioengineered with the recipient patient and has several mechanical characteristics similar to the native tendon[145-150]. Currently, one of the few viable therapeutic options, which is able to unbalance in favor of regeneration the scarring outcome present in tendon injuries with digital canal defect is the exogenous implementation of hyaluronic acid[151,152].
CONCLUSION
In the past decades, various surgical techniques have been described and employed to reconstruct tendon loss of substances. Despite significant progress in surgical and rehabilitation techniques, tendon reconstruction remains a very complex topic for both surgeons and patients.
New approaches such as WALANT and tissue engineering will perhaps improve current results. To date, the dream of regenerating injured tissues, and tendon tissue in particular, appears to be getting closer and closer, but it still has to contend with grey areas in our biological and biomolecular knowledge of scarring processes and the development of various tissues, and with the legislative and ethical difficulties that this field of research brings with it.
DECLARATIONS
Authors’ contributions
Concept and design: Bertolini M, Faccenda C, Parolo C, Stucchi S, Marchesini A, De Francesco F, Riccio M
Data acquisition, data analysis, and manuscript preparation: Faccenda C, Stucchi S, Marchesini A
Critical revision and completion of the manuscript: Bertolini M, Marchesini A, De Francesco F, Riccio M, Parolo C
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declare that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Informed consent was obtained from all patients.
Copyright
© The Author(s) 2023.
REFERENCES
1. LaSalle WB, Strickland JW. An evaluation of the two-stage flexor tendon reconstruction technique. J Hand Surg Am 1983;8:263-7.
2. Leversedge FJ, Zelouf D, Williams C, Gelberman RH, Seiler JG 3rd. Flexor tendon grafting to the hand: an assessment of the intrasynovial donor tendon-A preliminary single-cohort study. J Hand Surg Am 2000;25:721-30.
3. Coyle MP Jr, Leddy TP, Leddy JP. Staged flexor tendon reconstruction fingertip to palm. J Hand Surg Am 2002;27:581-5.
4. Freilich AM, Chhabra AB. Secondary flexor tendon reconstruction, a review. J Hand Surg Am 2007;32:1436-42.
5. Smith P, Jones M, Grobbelaar A. Two-stage grafting of flexor tendons: results after mobilisation by controlled early active movement. Scand J Plast Reconstr Surg Hand Surg 2004;38:220-7.
6. Boyes JH, Stark HH. Flexor-tendon grafts in the fingers and thumb. J Bone Joint Surg Am 1971;53:1332-42.
7. Schneider LH. Staged flexor tendon reconstruction using the method of Hunter. Clin Orthop Relat Res 1982;171:164-71.
8. Boyer MI, Strickland JW, Engles D, Sachar K, Leversedge FJ. Flexor tendon repair and rehabilitation: state of the art in 2002. Instr Course Lect 2003;52:137-61.
9. Le Viet D. Flexor tendon lengthening by tenotomy at the musculotendinous junction. Ann Plast Surg 1986;17:239-46.
10. Poggetti A, Novi M, Rosati M, Ciclamini D, Scaglione M, Battiston B. Treatment of flexor tendon reconstruction failures: multicentric experience with Brunelli active tendon implant. Eur J Orthop Surg Traumatol 2018;28:877-83.
11. Moore T, Anderson B, Seiler JG 3rd. Flexor tendon reconstruction. J Hand Surg Am 2010;35:1025-30.
12. Harrison SH. Repair of digital flexor tendon injuries in the hand. Br J Plast Surg 1961;14:211-30.
13. Lister GD, Kleinert HE, Kutz JE, Atasoy E. Primary flexor tendon repair followed by immediate controlled mobilization. J Hand Surg Am 1977;2:441-51.
14. Finsen V. Two-stage grafting of digital flexor tendons: a review of 43 patients after 3 to 15 years. Scand J Plast Reconstr Surg Hand Surg 2003;37:159-62.
15. White WL. Tendon grafts: a consideration of their source, procurement and suitability. Surg Clin North Am 1960;40:403-13.
16. Sun S, Ding Y, Ma B, Zhou Y. Two-stage flexor tendon reconstruction in zone II using Hunter's technique. Orthopedics 2010;33:880.
17. Gelberman RH, Seiler JG 3rd, Rosenberg AE, Heyman P, Amiel D. Intercalary flexor tendon grafts. a morphological study of intrasynovial and extrasynovial donor tendons. Scand J Plast Reconstr Surg Hand Surg 1992;26:257-64.
18. Gaspar MP, Wilbur DM, Stern PJ, Culp RW. Modified long toe extensor tendon harvest for use as intercalary graft in upper extremity reconstruction. J Hand Surg Am 2017;42:e209-13.
19. Bertelli JA, Santos MA, Kechele PR, Rost JR, Tacca CP. Flexor tendon grafting using a plantaris tendon with a fragment of attached bone for fixation to the distal phalanx: a preliminary cohort study. J Hand Surg Am 2007;32:1543-8.
20. Sood MK, Elliot D. A new technique of attachment of flexor tendons to the distal phalanx without a button tie-over. J Hand Surg Br 1996;21:629-32.
22. Hunter JM, Salisbury RE. Flexor-tendon reconstruction in severely damaged hands. J Bone Joint Surg Am 1971;53:829-858.
23. Rayner CR. The origin and nature of pseudo-synovium appearing around implanted silastic rods: an experimental study. Hand 1976;8:101-8.
24. Beris AE, Darlis NA, Korompilias AV, Vekris MD, Mitsionis GI, Soucacos PN. Two-stage flexor tendon reconstruction in zone II using a silicone rod and a pedicled intrasynovial graft. J Hand Surg Am 2003;28:652-60.
25. Brug E, Wetterkamp D, Neuber M, Probst A. [Secondary reconstruction of flexor tendon function of the fingers]. Unfallchirurg 1998;101:415-25.
26. Chuinard RG, Dabezies EJ, Mathews RE. Two-stage superficialis tendon reconstruction in severely damaged fingers. J Hand Surg Am 1980;5:135-43.
27. Paneva-Holevich E. Two-stage tenoplasty in injury of the flexor tendons of the hand. J Bone Joint Surg Am 1969;51:21-32.
28. Naam NH. Staged flexor tendon reconstruction using pedicled tendon graft from the flexor digitorum superficialis. J Hand Surg Am 1997;22:323-7.
29. Kessler FB. Use of a pedicled tendon transfer with a silicone rod in complicated secondary flexor tendon repairs. Plast Reconstr Surg 1972;49:439-43.
30. Boyce DE, Giddins G, Shewring DJ. Tendon disorders of the hand and wrist: IFSSH/FESSH instructional course book 2022 1st edition. Thieme Publishing Group; 2022.
31. Guimberteau JC, Bakhach J, Panconi B, Rouzaud S. A fresh look at vascularized flexor tendon transfers: concept, technical aspects and results. J Plast Reconstr Aesthet Surg 2007;60:793-810.
32. Cavadas PC, Pérez-García A, Thione A, Lorca-García C. Single-stage reconstruction of flexor tendons with vascularized tendon transfers. J Hand Surg Eur Vol 2015;40:259-68.
33. Tang JB. How to vent the pulley properly without tendon bowstringing in zone 2 repair. Chirurgie de la Main 2015;34:395-6.
34. Bosco F, Giustra F, Lusso A, Faccenda C, Artiaco S, Massè A. Closed flexor pulley injuries: a literature review and current practice. J Orthop 2022;34:246-9.
35. Artiaco S, Bosco F, Lusso A, Cioffi LL, Battiston B, Massè A. Flexor tendon pulley injuries: a systematic review of the literature and current treatment options. J Hand Microsurg 2022;Online ahead of print.
36. Nishida J, Amadio PC, Bettinger PC, An KN. Flexor tendon-pulley interaction after pulley reconstruction: a biomechanical study in a human model in vitro. J Hand Surg Am 1998;23:665-72.
38. Tang JB. Release of the A4 pulley to facilitate zone II flexor tendon repair. J Hand Surg Am 2014;39:2300-7.
39. Klinert HE, Bennett JB. Digital pulley reconstruction employing the always present rim of the previous pulley. J Hand Surg Am 1978;3:297-8.
40. Odobescu A, Radu A, Brutus JP, Gilardino MS. Modified flexor digitorum superficialis slip technique for A4 pulley reconstruction. J Hand Surg Eur Vol 2010;35:464-8.
41. Gabl M, Reinhart C, Lutz M, Bodner G, Angermann P, Pechlaner S. The use of a graft from the second extensor compartment to reconstruct the A2 flexor pulley in the long finger. J Hand Surg Br 2000;25:98-101.
42. Karev A, Stahl S, Taran A. The mechanical efficiency of the pulley system in normal digits compared with a reconstructed system using the “belt loop” technique. J Hand Surg Am 1987;12:596-601.
43. Lister GD. Reconstruction of pulleys employing extensor retinaculum. J Hand Surg Am 1979;4:461-4.
44. Okutsu I, Ninomiya S, Hiraki S, Inanami H, Kuroshima N. Three-loop technique for A2 pulley reconstruction. J Hand Surg Am 1987;12:790-4.
45. Widstrom CJ, Doyle JR, Johnson G, Manske PR, McGee R. A mechanical study of six digital pulley reconstruction techniques: Part II. strength of individual reconstructions. J Hand Surg Am 1989;14:826-9.
46. Lin G, Amadio P, An K, Cooney P, Chao E. Biomechanical analysis of finger flexor pulley reconstruction. J Hand Surg Br 1989;14:278-82.
47. Kleinert HE, Verdan C. Report of the committee on tendon injuries (international federation of societies for surgery of the hand). J Hand Surg Am 1983;8:794-8.
48. Wehbé MA, Mawr B, Hunter JM, Schneider LH, Goodwyn BL. Two-stage flexor-tendon reconstruction. ten-year experience. J Bone Joint Surg Am 1986;68:752-763.
49. Karakaplan M, Kilinc O, Ceylan MF, Ertem K, Aslanturk O. Mid-term results of two-stage tendon reconstruction of zone II flexor tendon injuries. Niger J Clin Pract 2021;24:1174-80.
50. Thomopoulos S, Parks WC, Rifkin DB, Derwin KA. Mechanisms of tendon injury and repair. J Orthop Res 2015;33:832-9.
51. Maeda E, Shelton JC, Bader DL, Lee DA. Differential regulation of gene expression in isolated tendon fascicles exposed to cyclic tensile strain in vitro. J Appl Physiol 2009;106:506-12.
52. Killian ML, Cavinatto L, Galatz LM, Thomopoulos S. The role of mechanobiology in tendon healing. J Shoulder Elbow Surg 2012;21:228-37.
53. Lehfeldt M, Ray E, Sherman R. MOC-PS(SM) CME article: treatment of flexor tendon laceration. Plast Reconstr Surg 2008;121:1-12.
54. Derby BM, Wilhelmi BJ, Zook EG, Neumeister MW. Flexor tendon reconstruction. Clin Plast Surg 2011;38:607-19.
57. Nolan GS, Kiely AL, Madura T, Karantana A. Wide-awake local anaesthesia no tourniquet (WALANT) vs regional or general anaesthesia for flexor tendon repair in adults: protocol for a systematic review and meta-analysis. Syst Rev 2020;9:264.
58. Fulchignoni C, Bonetti MA, Rovere G, Ziranu A, Maccauro G, Pataia E. Wide awake surgery for flexor tendon primary repair: A literature review. Orthop Rev 2020;12:8668.
59. Türker T, Hassan K, Capdarest-Arest N. Extensor tendon gap reconstruction: a review. J Plast Surg Hand Surg 2016;50:1-6.
60. Salihagić S, Zvizdić Z, Hrustemović D, Čaušević R, Hemaidi A. Modalities of extensor tendon repair related to etiological factors and associated injuries. Med Glas 2021;18:216-21.
61. Rockwell WB, Butler PN, Byrne BA. Extensor tendon: anatomy, injury, and reconstruction. Plast Reconstr Surg 2000;106:1592-603; quiz 1604, 1673.
62. Scheker LR, Langley SJ, Martin DL, Julliard KN. Primary extensor tendon reconstruction in dorsal hand defects requiring free flaps. J Hand Surg Br 1993;18:568-75.
63. Desai MJ, Wanner JP, Lee DH, Gauger EM. Failed extensor tendon repairs: extensor tenolysis and reconstruction. J Am Acad Orthop Surg 2019;27:563-74.
64. Kochevar A, Rayan G, Angel M. Extensor tendon reconstruction for zones II and IV using local tendon flap: a cadaver study. J Hand Surg Am 2009;34:1269-75.
65. Hanz KR, Saint-Cyr M, Semmler MJ, Rohrich RJ. Extensor tendon injuries: acute management and secondary reconstruction. Plast Reconstr Surg 2008;121:109e-20e.
66. Soni P, Stern CA, Foreman KB, Rockwell WB. Advances in extensor tendon diagnosis and therapy. Plast Reconstr Surg 2009;123:52e-7e.
67. Amirtharajah M, Lattanza L. Open extensor tendon injuries. J Hand Surg Am 2015;40:391-7; quiz 398.
68. Elson RA. Rupture of the central slip of the extensor hood of the finger. a test for early diagnosis. J Bone Joint Surg Br 1986;68:229-31.
69. Rubin J, Bozentka DJ, Bora FW. Diagnosis of closed central slip injuries. a cadaveric analysis of non-invasive tests. J Hand Surg Br 1996;21:614-6.
70. Snow JW. A method for reconstruction of the central slip of the extensor tendon of a finger. Plast Reconstr Surg 1976;57:455-9.
71. Chu PJ, Lee HM, Hou YT, Hung ST, Chen JK, Shih JT. Extensor-tendons reconstruction using autogenous palmaris longus tendon grafting for rheumatoid arthritis patients. J Orthop Surg Res 2008;3:16.
72. Schubert CD, Giunta RE. Extensor tendon repair and reconstruction. Clin Plast Surg 2014;41:525-31.
73. Sawaya ET, Choughri H, Pelissier P. One-stage treatment of delayed 'jersey finger' by Z-step lengthening of the flexor digitorum profundus tendon at the wrist. J Plast Reconstr Aesthet Surg 2012;65:264-6.
74. Lobo-Escolar L, López Moreno I, Montoya MP, Bosch-Aguilá M. Functional recovery following an l-lengthening local tendon flap for extensor pollicis longus chronic ruptures. J Hand Surg Am 2017;42:e41-7.
75. Cerovac S, Miranda BH. Tendon 'turnover lengthening' technique. J Plast Reconstr Aesthet Surg 2013;66:1587-90.
76. Nakamura S, Katsuki M. Tendon grafting for multiple extensor tendon ruptures of fingers in rheumatoid hands. J Hand Surg Br 2002;27:326-8.
77. Pulvertaft RG. Tendon grafts for flexor tendon injuries in the fingers and thumb; a study of technique and results. J Bone Joint Surg Br 1956;38:175-94.
78. Türker T, Capdarest-Arest N, Schmahl DT. Zone I extensor reconstruction with tendon salvaged from another finger. J Hand Surg Am 2014;39:976-80.
79. Seiler JG 3rd, Desai MJ, Payne SH. Tendon transfers for radial, median, and ulnar nerve palsy. J Am Acad Orthop Surg 2013;21:675-84.
80. Wang L, Fu J, Li M, Han D, Yang L. Repair of hand defects by transfer of free tissue flaps from toes. Arch Orthop Trauma Surg 2013;133:141-6.
81. Adani R, Marcoccio I, Tarallo L. Flap coverage of dorsum of hand associated with extensor tendons injuries: a completely vascularized single-stage reconstruction. Microsurgery 2003;23:32-9.
82. Ulusal BG, Lin YT, Ulusal AE, Lin CH. Free lateral arm flap for 1-stage reconstruction of soft tissue and composite defects of the hand: a retrospective analysis of 118 cases. Ann Plast Surg 2007;58:173-8.
83. Xie RG, Tang JB. Allograft tendon for second-stage tendon reconstruction. Hand Clin 2012;28:503-9.
84. Chung US, Kim JH, Seo WS, Lee KH. Tendon transfer or tendon graft for ruptured finger extensor tendons in rheumatoid hands. J Hand Surg Eur Vol 2010;35:279-82.
85. Ratner JA, Peljovich A, Kozin SH. Update on tendon transfers for peripheral nerve injuries. J Hand Surg Am 2010;35:1371-81.
86. Peljovich A, Ratner JA, Marino J. Update of the physiology and biomechanics of tendon transfer surgery. J Hand Surg Am 2010;35:1365-9; quiz 1370.
88. Liao JCY, Das De S. Management of tendon and bony injuries of the distal phalanx. Hand Clin 2021;37:27-42.
89. Savvidou C, Thirkannad S. Hemilateral band technique for reconstructing gap defects in the terminal slip of the extensor tendon. Tech Hand Up Extrem Surg 2011;15:177-81.
90. Gu YP, Zhu SM. A new technique for repair of acute or chronic extensor tendon injuries in zone 1. J Bone Joint Surg Br 2012;94:668-70.
91. Inoue G, Tamura Y. Dislocation of the extensor tendons over the metacarpophalangeal joints. J Hand Surg Am 1996;21:464-9.
92. Xu L, Liu Z, Liu S, Jorgensen AM, Hou R, Ju J. Repair of compound dorsal defects of the digits using a free antegrade palmaris longus tendocutaneous venous flap. J Hand Surg Am 2023;48:510.e1-5.
93. Lin CH, Wei FC, Lin YT, Chen CT. Composite palmaris longus-venous flap for simultaneous reconstruction of extensor tendon and dorsal surface defects of the hand--long-term functional result. J Trauma 2004;56:1118-22.
94. Snow JW. Use of a retrograde tendon flap in repairing a severed extensor in the pip joint area. Plast Reconstr Surg 1973;51:555-8.
95. Brown SH, Hentzen ER, Kwan A, Ward SR, Fridén J, Lieber RL. Mechanical strength of the side-to-side versus pulvertaft weave tendon repair. J Hand Surg Am 2010;35:540-5.
96. Fridén J, Tirrell TF, Bhola S, Lieber RL. The mechanical strength of side-to-side tendon repair with mismatched tendon size and shape. J Hand Surg Eur Vol 2015;40:239-45.
97. Al-Qattan MM. Two-staged extensor tendon reconstruction for zone 6 extensor tendon loss of the fingers: indications, technique and results. J Hand Surg Eur Vol 2015;40:276-80.
98. Chester DL, Beale S, Beveridge L, Nancarrow JD, Titley OG. A prospective, controlled, randomized trial comparing early active extension with passive extension using a dynamic splint in the rehabilitation of repaired extensor tendons. J Hand Surg Br 2002;27:283-8.
99. Vyrva O, Kvann J, Karpinsky M, Ozyurekoglu T. A reconstructive extensor tendon centralization technique for sagittal band disruption. Tech Hand Up Extrem Surg 2020;24:20-5.
100. Watson HK, Weinzweig J, Guidera PM. Sagittal band reconstruction. J Hand Surg Am 1997;22:452-6.
101. Takahashi N, Iba K, Hanaka M, Ozasa Y, Kanaya K, Yamashita T. Sagittal band reconstruction in the index finger using a modified Elson technique. J Orthop Surg 2018;26:2309499017749985.
102. Beldner S, Polatsch DB. Arthrodesis of the metacarpophalangeal and interphalangeal joints of the hand: current concepts. J Am Acad Orthop Surg 2016;24:290-7.
103. Shannon FT, Barton NJ. Surgery for rupture of extensor tendons in rheumatoid arthritis. Hand 1976;8:279-86.
104. Bora FW Jr, Osterman AL, Thomas VJ, Maitin EC, Polineni S. The treatment of ruptures of multiple extensor tendons at wrist level by a free tendon graft in the rheumatoid patient. J Hand Surg Am 1987;12:1038-40.
105. Ohshio I, Ogino T, Minami A, Kato H, Miyake. Extensor tendon rupture due to osteoarthritis of the distal radio-ulnar joint. J Hand Surg Br 1991;16:450-3.
106. Moore JR, Weiland AJ, Valdata L. Tendon ruptures in the rheumatoid hand: analysis of treatment and functional results in 60 patients. J Hand Surg Am 1987;12:9-14.
107. Minami M, Kato S, Yamazaki J, Minami A. Tendon ruptures in the rheumatoid hand. In: Vol 1083. Elsevier; 1995.p.515-515.
108. Nalebuff E. Extensor tendon ruptures in rheumatoid arthritis. CV Mosby; 1987.p.385-392.
109. Mason C, Brindley DA, Culme-Seymour EJ, Davie NL. Cell therapy industry: billion dollar global business with unlimited potential. Regen Med 2011;6:265-72.
110. Yang G, Rothrauff BB, Tuan RS. Tendon and ligament regeneration and repair: clinical relevance and developmental paradigm. Birth Defects Res C Embryo Today 2013;99:203-22.
111. Cheng X, Tsao C, Sylvia VL, et al. Platelet-derived growth-factor-releasing aligned collagen-nanoparticle fibers promote the proliferation and tenogenic differentiation of adipose-derived stem cells. Acta Biomater 2014;10:1360-9.
112. Nichols AEC, Best KT, Loiselle AE. The cellular basis of fibrotic tendon healing: challenges and opportunities. Transl Res 2019;209:156-68.
113. Goh JC, Ouyang HW, Teoh SH, Chan CK, Lee EH. Tissue-engineering approach to the repair and regeneration of tendons and ligaments. Tissue Eng 2003;9 Suppl 1:S31-44.
114. Voleti PB, Buckley MR, Soslowsky LJ. Tendon healing: repair and regeneration. Annu Rev Biomed Eng 2012;14:47-71.
115. Zhang L, Bao D, Li P, et al. Particle-induced SIRT1 downregulation promotes osteoclastogenesis and osteolysis through ER stress regulation. Biomed Pharmacother 2018;104:300-6.
116. Caplan AI. Review: mesenchymal stem cells: cell-based reconstructive therapy in orthopedics. Tissue Eng 2005;11:1198-211.
117. Yoshimura K, Shigeura T, Matsumoto D, et al. Characterization of freshly isolated and cultured cells derived from the fatty and fluid portions of liposuction aspirates. J Cell Physiol 2006;208:64-76.
118. De Francesco F, Matta C, Riccio M, Sbarbati A, Mobasheri A. Reevolution of tissue regeneration: from recent advances in adipose stem cells to novel therapeutic approaches. Stem Cells Int 2021;2021:2179429.
119. Vindigni V, Tonello C, Lancerotto L, et al. Preliminary report of in vitro reconstruction of a vascularized tendonlike structure: a novel application for adipose-derived stem cells. Ann Plast Surg 2013;71:664-70.
120. Zocchi ML, Facchin F, Pagani A, et al. New perspectives in regenerative medicine and surgery: the bioactive composite therapies (BACTs). Eur J Plast Surg 2022;45:1-25.
121. Kurtz CA, Loebig TG, Anderson DD, DeMeo PJ, Campbell PG. Insulin-like growth factor I accelerates functional recovery from Achilles tendon injury in a rat model. Am J Sports Med 1999;27:363-9.
122. Klein MB, Yalamanchi N, Pham H, Longaker MT, Chang J. Flexor tendon healing in vitro: effects of TGF-beta on tendon cell collagen production. J Hand Surg Am 2002;27:615-20.
123. Chan BP, Fu S, Qin L, Lee K, Rolf CG, Chan K. Effects of basic fibroblast growth factor (bFGF) on early stages of tendon healing: a rat patellar tendon model. Acta Orthop Scand 2000;71:513-8.
124. Schweitzer R, Chyung JH, Murtaugh LC, et al. Analysis of the tendon cell fate using Scleraxis, a specific marker for tendons and ligaments. Development 2001;128:3855-66.
125. Léjard V, Brideau G, Blais F, et al. Scleraxis and NFATc regulate the expression of the pro-alpha1(I) collagen gene in tendon fibroblasts. J Biol Chem 2007;282:17665-75.
126. Chen S, Wang J, Chen Y, Mo X, Fan C. Tenogenic adipose-derived stem cell sheets with nanoyarn scaffolds for tendon regeneration. Mater Sci Eng C Mater Biol Appl 2021;119:111506.
127. Park A, Hogan MV, Kesturu GS, James R, Balian G, Chhabra AB. Adipose-derived mesenchymal stem cells treated with growth differentiation factor-5 express tendon-specific markers. Tissue Eng Part A 2010;16:2941-51.
128. Jenner JM, van Eijk F, Saris DB, Willems WJ, Dhert WJ, Creemers LB. Effect of transforming growth factor-beta and growth differentiation factor-5 on proliferation and matrix production by human bone marrow stromal cells cultured on braided poly lactic-co-glycolic acid scaffolds for ligament tissue engineering. Tissue Eng 2007;13:1573-82.
129. Haimi S, Vuornos K, Björninen M, et al. Human adipose stem cells differentiated on braided polylactide scaffolds is a potential approach for tendon tissue engineering. Tissue Eng Part A 2016;22:512-23.
130. Lee CH, Shah B, Moioli EK, Mao JJ. CTGF directs fibroblast differentiation from human mesenchymal stem/stromal cells and defines connective tissue healing in a rodent injury model. J Clin Invest 2010;120:3340-9.
131. Lee CH, Moioli EK, Mao JJ. Fibroblastic differentiation of human mesenchymal stem cells using connective tissue growth factor. Conf Proc IEEE Eng Med Biol Soc 2006;2006:775-8.
132. Havis E, Bonnin MA, Olivera-Martinez I, et al. Transcriptomic analysis of mouse limb tendon cells during development. Development 2014;141:3683-96.
133. Guerquin MJ, Charvet B, Nourissat G, et al. Transcription factor EGR1 directs tendon differentiation and promotes tendon repair. J Clin Invest 2013;123:3564-76.
134. Galatz LM, Charlton N, Das R, Kim HM, Havlioglu N, Thomopoulos S. Complete removal of load is detrimental to rotator cuff healing. J Shoulder Elbow Surg 2009;18:669-75.
135. Thomopoulos S, Genin GM, Galatz LM. The development and morphogenesis of the tendon-to-bone insertion - what development can teach us about healing -. J Musculoskelet Neuronal Interact 2010;10:35-45.
136. Kuo CK, Tuan RS. Mechanoactive tenogenic differentiation of human mesenchymal stem cells. Tissue Eng Part A 2008;14:1615-27.
137. Liu Y, Ramanath HS, Wang DA. Tendon tissue engineering using scaffold enhancing strategies. Trends Biotechnol 2008;26:201-9.
138. Kishore V, Bullock W, Sun X, Van Dyke WS, Akkus O. Tenogenic differentiation of human MSCs induced by the topography of electrochemically aligned collagen threads. Biomaterials 2012;33:2137-44.
139. Deeken CR, White AK, Bachman SL, et al. Method of preparing a decellularized porcine tendon using tributyl phosphate. J Biomed Mater Res B Appl Biomater 2011;96:199-206.
140. Chen B, Wang B, Zhang WJ, Zhou G, Cao Y, Liu W. In vivo tendon engineering with skeletal muscle derived cells in a mouse model. Biomaterials 2012;33:6086-97.
141. Wan Y, Chen W, Yang J, Bei J, Wang S. Biodegradable poly(L-lactide)-poly(ethylene glycol) multiblock copolymer: synthesis and evaluation of cell affinity. Biomaterials 2003;24:2195-203.
142. Fessel G, Gerber C, Snedeker JG. Potential of collagen cross-linking therapies to mediate tendon mechanical properties. J Shoulder Elbow Surg 2012;21:209-17.
143. Teh TK, Toh SL, Goh JC. Aligned fibrous scaffolds for enhanced mechanoresponse and tenogenesis of mesenchymal stem cells. Tissue Eng Part A 2013;19:1360-72.
144. Zocchi ML, Vindigni V, Pagani A, et al. Regulatory, ethical, and technical considerations on regenerative technologies and adipose-derived mesenchymal stem cells. Eur J Plast Surg 2019;42:531-48.
145. De Francesco F, Gravina P, Busato A, et al. Stem cells in autologous microfragmented adipose tissue: current perspectives in osteoarthritis disease. Int J Mol Sci 2021;22:10197.
146. Dai Prè E, Busato A, Mannucci S, et al. In vitro characterization of adipose stem cells non-enzymatically extracted from the thigh and abdomen. Int J Mol Sci 2020;21:3081.
147. Senesi L, De Francesco F, Farinelli L, et al. Mechanical and enzymatic procedures to isolate the stromal vascular fraction from adipose tissue: preliminary results. Front Cell Dev Biol 2019;7:88.
148. Busato A, De Francesco F, Biswas R, et al. Simple and rapid non-enzymatic procedure allows the isolation of structurally preserved connective tissue micro-fragments enriched with SVF. Cells 2020;10:36.
149. Botto R, Riccio V, Galosi L, et al. Effects of intra-articular autologous adipose micrograft for the treatment of osteoarthritis in dogs: a prospective, randomized, controlled study. Animals 2022;12:1844.
150. De Francesco F, Mannucci S, Conti L, Dai Prè E, Sbarbati A, Riccio M. A non-enzymatic method to obtain a fat tissue derivative highly enriched in adipose stem cells (ascs) from human lipoaspirates: preliminary results. Int J Mol Sci 2018;19:2061.
151. Riccio M, Battiston B, Pajardi G, et al. Study Group on Tendon Adhesion of Italian Society of Hand Surgery. Efficiency of hyaloglide in the prevention of the recurrence of adhesions after tenolysis of flexor tendons in zone II: a randomized, controlled, multicentre clinical trial. J Hand Surg Eur Vol 2010;35:130-8.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Bertolini M, Faccenda C, Parolo C, Stucchi S, Marchesini A, De Francesco F, Riccio M. Reconstruction of tendon losses. Plast Aesthet Res 2023;10:34. http://dx.doi.org/10.20517/2347-9264.2022.121
AMA Style
Bertolini M, Faccenda C, Parolo C, Stucchi S, Marchesini A, De Francesco F, Riccio M. Reconstruction of tendon losses. Plastic and Aesthetic Research. 2023; 10: 34. http://dx.doi.org/10.20517/2347-9264.2022.121
Chicago/Turabian Style
Bertolini, Maddalena, Carlotta Faccenda, Chiara Parolo, Sara Stucchi, Andrea Marchesini, Francesco De Francesco, Michele Riccio. 2023. "Reconstruction of tendon losses" Plastic and Aesthetic Research. 10: 34. http://dx.doi.org/10.20517/2347-9264.2022.121
ACS Style
Bertolini, M.; Faccenda C.; Parolo C.; Stucchi S.; Marchesini A.; De Francesco F.; Riccio M. Reconstruction of tendon losses. Plast. Aesthet. Res. 2023, 10, 34. http://dx.doi.org/10.20517/2347-9264.2022.121
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 4 clicks
Cite This Article 4 clicks






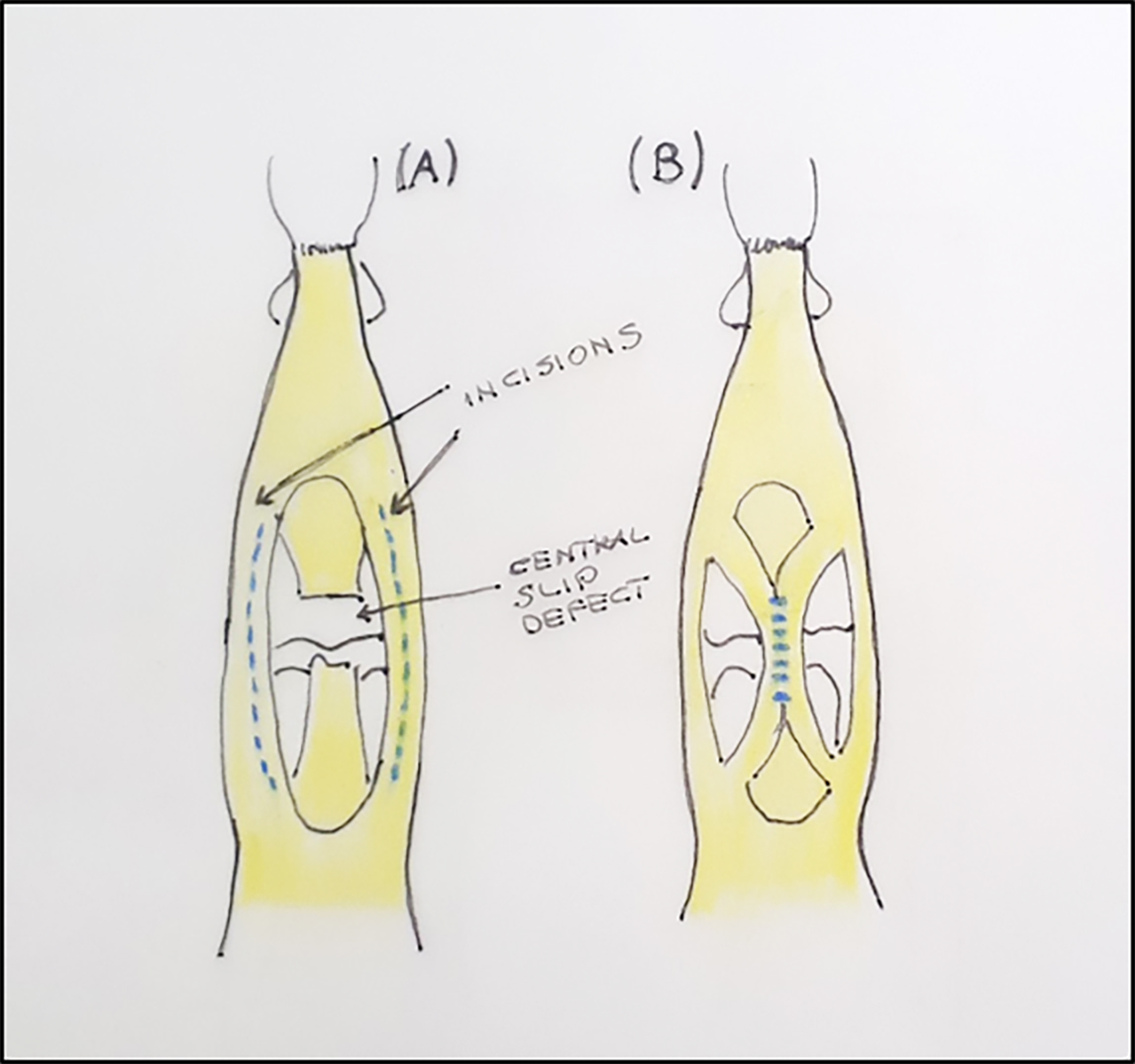










Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.