Imaging after liver-directed therapy: evidenced-based update of the LI-RADS treatment response algorithm
Abstract
There are multiple liver-directed treatment options for hepatocellular carcinoma (HCC), which provide curative intent, help patients achieve remission, and/or provide a bridge to transplant by controlling local tumor progression and downstaging patients. After locoregional therapy (LRT), management of these patients, including liver transplant candidacy, is guided by treatment response assessment. The Liver Imaging Reporting and Data Systems (LI-RADS) treatment response algorithm (TRA) was created to provide a standardized assessment of HCC following LRT. Originally created primarily on expert opinion, subsequent literature has continued to evaluate the validity of this algorithm. In this manuscript, we review emerging literature supporting the use of LI-RADS in the assessment of HCC treatment response after LRT and highlight future updates.
Keywords
INTRODUCTION
Hepatocellular carcinoma (HCC) is the most common cancer in cirrhotic patients and leads to increased morbidity and mortality[1]. Hepatic transplantation is a potentially curative treatment for HCC. However, due to the limited availability of transplant organs and the potential for tumor progression while awaiting transplant, multiple locoregional therapies (LRTs) have been used primarily as a bridge to transplant. Broadly, these treatment options include locoablative, intra-arterial non-radiation, and radiation-based therapies.
The Liver Reporting and Data System (LI-RADS) was created in 2011 to standardize reporting of primary liver tumors using specific diagnostic criteria and algorithms[2]. The LI-RADS treatment response algorithm (LI-RADS TRA) was subsequently added to the existing algorithm in 2017 to provide a guide for the evaluation of tumor viability after LRT. Many studies have since evaluated the accuracy of the LI-RADS TRA[3-6], some of which have been discussed in a prior review article by our group[7].
New literature reporting the performance of the LI-RAD TRA and its ability to predict patient survival continues to emerge. This paper will provide an update highlighting strengths and weaknesses in treatment response assessment after LRT for HCC, and identify areas for future improvements.
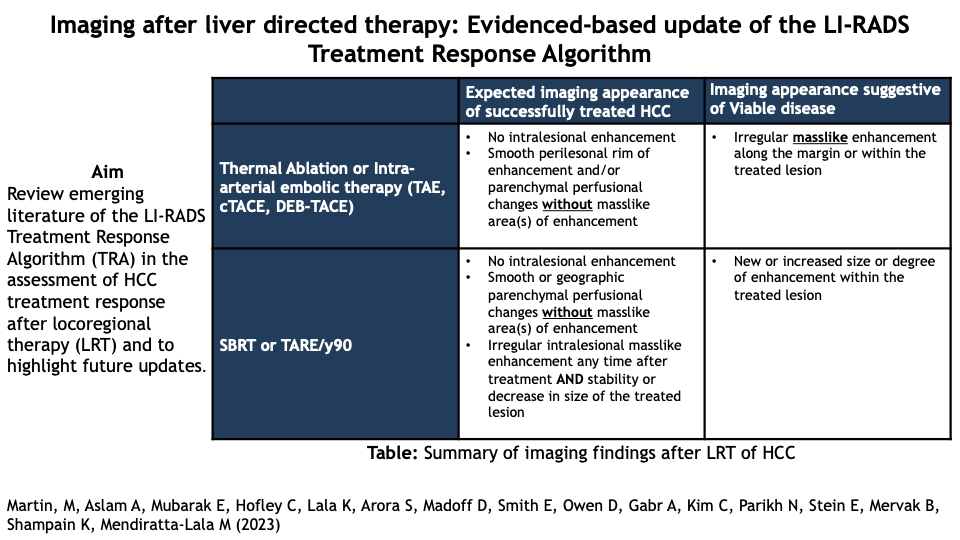
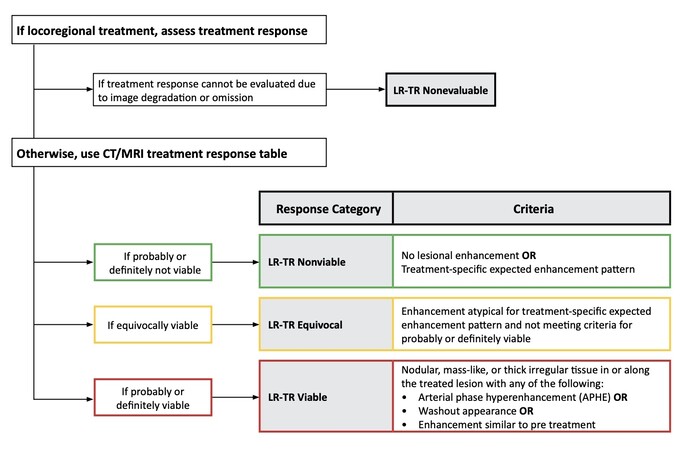
OVERVIEW OF THE LI-RADS TRA
The LI-RADS TRA allows standardization for image acquisition, interpretation, reporting, and data collection for HCC following treatment with LRTs. While other treatment response systems exist, LI-RADS TRA is unique in that it provides an assessment of each individually treated lesion, which is important as these high-risk patients have a dynamic disease process in which new foci of disease can arise anywhere in the liver at any time, independent of previously treated areas. Furthermore, different HCCs can be treated with different modalities. Treatment response following LRT is evaluated by multiphasic contrast-enhanced CT (CECT) or MRI (CEMRI) utilizing either hepatobiliary or extracellular contrast agents. The key imaging feature used for the assessment of viability is arterial phase hyperenhancement (APHE). However, other imaging characteristics that are evaluated include washout on delayed sequences and enhancement similar to pretreatment [Figure 1][2]. Each liver lesion is assessed separately, usually at 3-month intervals during surveillance imaging.
Imaging appearance of HCC following LRTs varies depending on the type of LRT, and therefore the radiologist must understand each therapy used for treatment and the expected post-therapy imaging appearances in order to accurately characterize residual or recurrent neoplasm. In its current for, the LI-RADS TRA has one categorization system to evaluate posttreatment imaging characteristics (APHE, washout, and enhancement similar to pretreatment), which categorize lesions as LI-RADS Treatment Response (LR-TR) viable, nonviable, or equivocal, regardless of the LRT performed. The following section will highlight common appearances of HCC treated with different forms of LRT and will provide guidance on the utilization of the LI-RADS TRA in its current form.
IMAGING APPEARANCES OF TREATED HCC
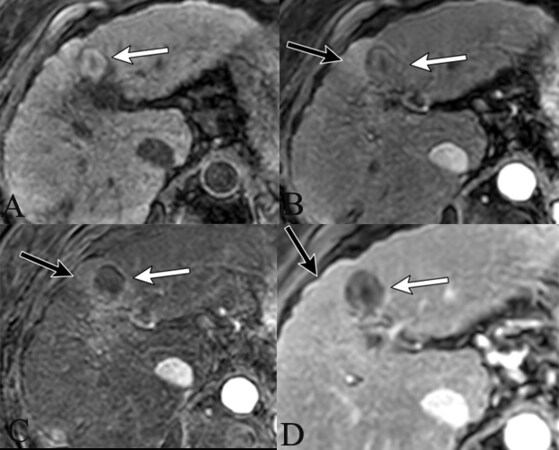
The most commonly performed thermal ablation therapies include radiofrequency ablation (RFA), microwave ablation (MWA), and cryoablation, which use heating or freezing to induce tumoral cell death and necrosis. Key points to recognize after these forms of therapy are that the ablation zone size should be 5-10 mm larger than the original tumor size and that a smooth thin hyperenhancing rim can be seen along the ablation zone margin due to increased arterial flow related to early inflammation [Figure 2][8].
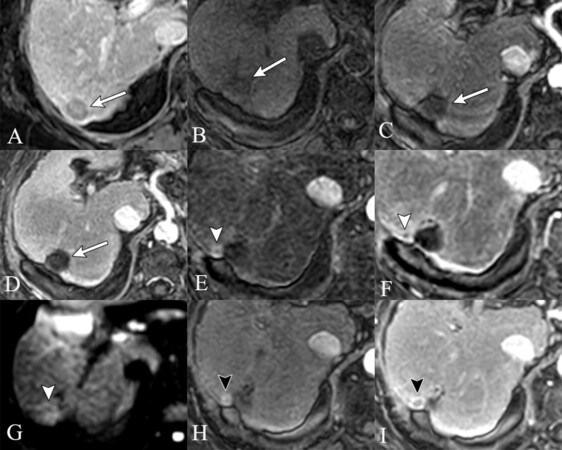
Figure 2. 78-year-old with HCV cirrhosis 3 months status post-MWA for LR 5 HCC segment 4a/b (images not shown). 1 month post-MWA, expected post-thermal ablation findings of central T1 precontrast hyperintensity, consistent with coagulation necrosis (A). There is no intralesional APHE (B) confirmed on subtraction (C), with no additional features on delayed phase (D), LR-TR nonviable (white arrows). Peripheral wedge-shaped area of geographic APHE surrounding the treatment zone, becomes isoenhancing on delayed phases, consistent with posttreatment perfusional changes (black arrows).
Non-radiation intra-arterial therapies include transarterial chemoembolization (TACE), drug-eluting bead TACE (DEB-TACE), and bland transarterial embolization (TAE), which use intra-arterial administration of embolic particles with or without chemotherapy to induce cell death using embolic/ischemic and/or chemotherapeutic mechanisms. Similar to percutaneous ablation, tumor size following treatment may transiently increase due to posttreatment edema or hemorrhage but will eventually decrease over time[9]. Additionally, a thin enhancing rim can be seen along the periphery of the treatment zone [Figure 3][10].
Figure 3. 68-year-old female with chronic HBV presenting with a large LR 5 observation showing APHE (A) and washout (B). Arterial phase MRI 1 month after TACE shows no intralesional enhancement and a smooth perilesional rim of enhancement without masslike areas of enhancement (C).
Similar imaging characteristics are used to evaluate effective treatment or residual viable tumor following LRT with thermal ablation and non-radiation intra-arterial embolic therapy. The defining characteristic of nonviable disease is the complete lack of enhancement of the targeted tumor [Figure 2,3]. Hyperdensity on unenhanced CT and hyperintense signal on precontrast T1-weighted imaging following ablation occurs secondary to coagulative necrosis; therefore, non-contrast/subtraction sequences must be utilized following contrast administration to differentiate between coagulative necrosis and residual/recurrent viable tumor [Figure 2][9,10]. In contrast, nodular, masslike, or irregular APHE within or along the margin of the treatment zone, washout appearance, or an enhancement pattern similar to the pretreatment observation should prompt the radiologist to categorize the treated observation as LR-TR viable [Figure 4][9].
Figure 4. 68-year-old with alcoholic induced cirrhosis presents with biopsy proven HCC in segment 6 (A). 1 month post-MWA there are expected posttreatment imaging findings of central T1 precontrast hyperintense signal related to coagulation necrosis (B), no APHE (C), no washout (D), LR-TR nonviable (white arrows). 6 months post-MWA there is a new 8 mm nodular masslike area of APHE (E), with no corresponding finding on delayed phase (F) (white arrowheads). By strict application of the LI-RADS TRA v2018, this is considered LR-TR viable, however, the reader chose to categorize this observation as LR-TR equivocal. Note the presence of mild diffusion restriction (G). 9 months post-MWA the previously seen area of APHE measures 1.1 cm (H), with washout and capsule appearance (I), now definitively LR-TR viable (black arrowheads). Of note, the use of diffusion restriction as an ancillary feature at 6 months could have upgraded this to definitive LR-TR viable category at 6 months.
A unique imaging appearance is seen after transarterial embolic therapy with iodized oil (i.e., lipiodol). Iodized oil is hyperdense on non-contrast CT, a finding which could limit evaluation for viability as small areas of APHE within and along the area of treatment may not be accurately seen[11]. It is therefore important to carefully compare posttreatment imaging with pretreatment imaging to define the true borders of the tumor. A second unique imaging aspect of iodized oil is that its staining pattern within the targeted tumor can help to provide a more accurate response assessment, which will be discussed in the emerging evidence section below.
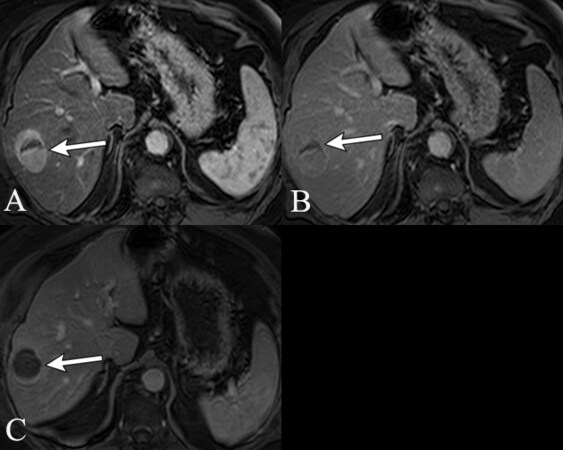
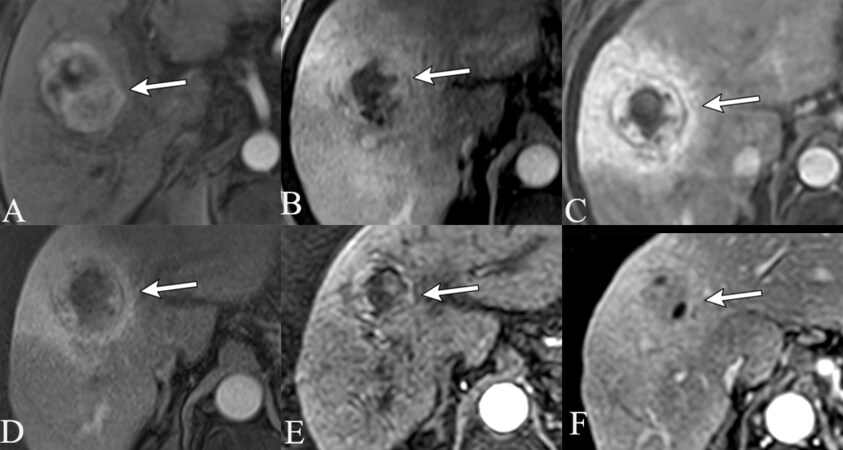
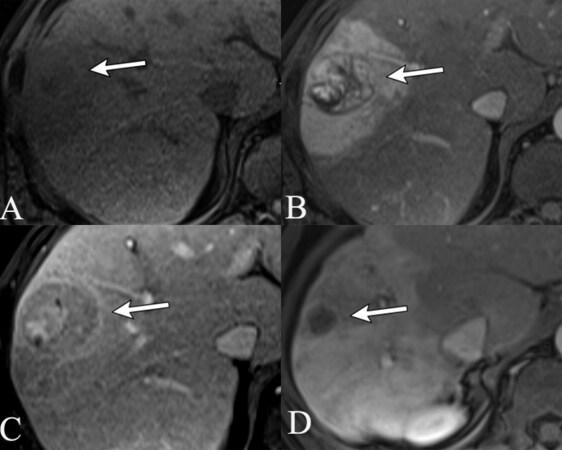
In contrast, lesions treated with radiation-based therapies including stereotactic body radiotherapy (SBRT) and transarterial radiotherapy (TARE, Y-90 radioembolization) have a different expected posttreatment imaging appearance compared to conventional forms of LRT. While post-radiation treated HCC can exhibit immediate non-enhancement, a large proportion of tumors can exhibit persistent APHE with or without a persistent washout appearance. These findings can be seen for up to a year or longer on contrast-enhanced CT or MRI[10]. Literature suggests that both enhancement and size should gradually decrease over time for nonviable lesions, unlike viable tumors where enhancement and/or size increase[12,13]. Using the LI-RADS TRA in its current iteration, radiation (SBRT or TARE) treated HCC would therefore be categorized as nonviable if there is no visualized enhancement, equivocal if there is persistent enhancement either stable or decreased size, and viable if there is new or increasing hyperenhancement and/or an increase in size [Figure 5, Figure 6]. Imaging after radiation therapy should be performed no earlier than 3 months after treatment because of early posttreatment edema. Although MRI and CT can be used for treatment response assessment, MRI is preferred because of better contrast resolution.
Figure 5. 69-year-old with alcohol cirrhosis presents with LR 5 HCC (A). 3 months post-SBRT there is central necrosis with persistent thick peripheral APHE (B). There is also extensive peri-tumoral parenchymal APHE related to radiation changes. 6 (C), 9 (D) and 12 (E) months post-SBRT there is continued decrease in size of the treated tumor with persistent but decreasing thick peripheral rim enhancement. The extensive surrounding parenchymal geographic APHE is maximal at 6 months and then decreases. It eventually converts to delayed phase enhancement, compatible with radiation fibrosis (F). Based on the current LI-RADS v2018 TRA, this tumor would be categorized as LR-TR equivocal at all times points, however, the one year of stability with absence of progression is reassuring that the imaging features are expected post-SBRT findings with no clinically significant viable tumor. In future iterations of the LI-RADS TRA, this would be categorized as LR-TR nonprogressing at all timepoints.
After treatment with radiation-based therapies, extensive perfusional changes are expected within the region of liver parenchyma targeted for treatment. It is therefore essential to compare posttreatment imaging to pretreatment imaging in order to distinguish posttreatment changes from viable tumors. Posttreatment changes demonstrate geographic APHE which becomes either hyperenhancing or isoenhancing relative to background hepatic parenchyma on portal venous and delayed phase imaging, without washout [Figure 5 and Figure 6][10]. This is unlike persistently enhancing tumors, which can demonstrate washout, although persistent APHE and washout are also compatible with expected post-radiation changes. However, if there are new areas of APHE and washout when compared to the original tumor margins, progression must be considered.
Figure 6. 48-year-old with HCV cirrhosis status post TARE of right lobe LR 5 HCC (not shown).(A) 3 months post-TARE the treated mass demonstrates areas of necrosis with persistent heterogeneous mass like intralesional APHE (B) and persistent washout (C). Extensive geographic parenchymal APHE (B) which becomes isoenhancing on PV phase of imaging (C), compatible with post-radiation changes, LR-TR equivocal based on LI-RADS TRA v2018. At 12 months post-TARE, the treated HCC is now small and completely necrotic with no areas of APHE (D), LR-TR nonviable. There is extensive radiation fibrosis in the parenchyma.
Categorization of a treated tumor as equivocal is reserved for lesions that do not meet the criteria for probable or definitely viable tumor, but instead display an enhancement pattern that is atypical for the type of treatment administered. This may be seen in instances where the hepatic tissue surrounding the lesion has been affected by treatment and displays abnormal enhancement. Equivocal categorization of a liver lesion should prompt subsequent reimaging to reassess the possibility of viability. Ancillary features (AF) (including diffusion restriction, mild T2 hyperintensity, transitional and hepatobiliary phase hypointensity) are not included in the current LI-RADS TRA algorithm, unlike the diagnostic LI-RADS algorithm.
Emerging evidence on the performance of LI-RADS TRA
Diagnostic performance for local ablative and non-radiation intra-arterial embolic therapies
Many studies in recent years have assessed the validity and utility of the LI-RADS TRA by analyzing inter-reader reliability and radiologic-pathologic correlation after thermal ablative and intra-arterial embolic therapies. There are two facets that must be considered when evaluating the validity of a treatment response algorithm. First, LR-TR categorization needs to have high inter-reader reliability, as final interpretation impacts patient management. Second, LR-TR categorization should predict outcomes data such as overall survival (OS), time to progression (TTP), and disease-free survival (DFS).
A recent review article summarized the emerging data evaluating the LI-RADS TRA [9] in which the reported studies all validated the use of LI-RADS TRA after treatment with bland embolization, TACE, and thermal ablation, with high interobserver agreements for categorization of viability and nonviability (κ = 0.55-0.75)[3-6].
Similar to many previously published papers[3-6], newer studies using CT to evaluate LI-RADS TRA performance have shown moderate to substantial overall interobserver agreement following RFA (κ = 0.602[14]), bland TAE (κ = 0.68[15]) and conventional TACE (κ = 0.69[16], κ = 0.70[17]) for the viable and nonviable categories. The agreement has been shown to be excellent for nonviable (κ = 0.80, 95%CI: 0.68-0.92), substantial for viable (κ = 0.78, 95%CI: 0.67-0.90), and fair for equivocal (κ = 0.25, 95%CI: 0.02-0.49) LR-TR categories after conventional TACE[17].
Most published data shows high sensitivity of the LI-RADS TRA for detecting viable or nonviable disease. However, data is not as convincing for the LR-TR equivocal category, where the prediction of incomplete necrosis is higher when the LR-TR equivocal category is treated as viable[3,4]. When the equivocal category was treated as viable, there was a higher sensitivity (81%-87%) to predict incomplete necrosis versus 40%-77% when considered nonviable[3]. In addition, specificity improved slightly when the equivocal category was treated as viable versus nonviable (81%-85% vs. 85%-97%, respectively)[3]. Similarly, when the equivocal category was reclassified as viable in another study, the sensitivity for predicting incomplete necrosis was 44% vs. 30% when considered nonviable[6]. Specificity and positive predictive value (PPV) improved from 86% to 99% and 67% to 93%, respectively, for predicting complete necrosis when the equivocal category was considered viable versus nonviable[6]. When considering the equivocal category as viable versus nonviable, accuracies of 60-65% vs. 67-71%, PPVs of 86-96%, and negative predictive values (NPV) of 81-87% have been found[4]. Finally, a recent meta-analysis evaluated four studies in which HCC was treated with either intra-arterial embolization or ablation and demonstrated that a majority (70.5%) of lesions classified as equivocal were pathologically viable[18]. Hence, it can be postulated that most lesions classified as equivocal are in fact incompletely treated following ablation and intra-arterial embolization despite their necrotic imaging appearance[3,4].
Thus far, emerging evidence demonstrates that overall interobserver agreement of the LI-RADS TRA is high in distinguishing viable versus nonviable categories. However, in addition to validation studies for the algorithm, it is also important to assess the agreement of the features involved in LR-TR categorization to ensure its clinical utility. The key imaging components of the LI-RADS TRA include APHE, delayed washout, and enhancement similar to pretreatment. These imaging features are unique compared to existing response classification systems [e.g. modified Response Evaluation Criteria in Solid Tumors (mRECIST), European Association for the Study of the Liver (EASL)]. Agreement has been shown to be highest for APHE following conventional TACE (κ = 0.79)[17] and bland TAE (κ = 0.66)[15], and substantially high for washout appearance (κ = 0.69)[17]. Multiple studies corroborate these findings, demonstrating that the presence of APHE has the highest diagnostic accuracy for predicting incomplete necrosis (AUC 0.69, 95%CI: 0.58-0.80), whereas the lack of APHE and an interval decrease in size have the highest accuracy for predicting complete necrosis (AUC 0.75, 95%CI: 0.62-0.88)[3,4,17,19]. Studies evaluating LR-TR features on CT show relatively high agreement in APHE (κ = 0.71-0.80), washout (κ = 0.67-0.72), and enhancement similar to pretreatment (κ = 0.62 to 0.73)[5,20,21]. Therefore, these studies suggest that posttreatment APHE following thermal ablation or intra-arterial embolic therapy has the highest sensitivity for diagnosing viable HCC, while enhancement similar to pretreatment provided no significant clinical utility, a finding which will be changed in future modifications in the LI-RADS TRA[21].
In addition to validating the current LI-RADS TRA, it is important to investigate the association between LR-TR category and patient outcomes. LR-TR categorization has been shown to have a strong association with overall survival in patients treated with bland TAE ranging from 25.7-26.4 months for viable and 64.2 months for nonviable lesions[15]. Similar results were seen in patients treated with RFA, with significantly lower overall survival in patients with LR-TR viable lesions compared to equivocal and nonviable lesions[14].
Significant differences have been identified in overall survival between nonviable versus viable or equivocal lesions following conventional TACE[16]. Patients with viable and equivocal disease had a median overall survival of 27 months compared to 73 months for nonviable[16]. However, following multivariate analysis, it was noted that the analyzed groups differed significantly in terms of baseline function and Barcelona Clinic Liver Cancer (BCLC) stage, which likely in part contributed to the aforementioned survival differences[16]. Time to progression was not significantly different between viable and nonviable disease categories[16]. While outcomes data seems to correlate with viable versus nonviable disease, LI-RADS TRA should not be used alone to predict patient outcomes after LRT to HCC.
Studies show similar diagnostic performance in TRA after LRT using mRECIST and LI-RADS TRA. However, mRECIST provides a patient-level assessment, whereas LI-RADS TRA provides lesion-level assessment. Therefore, since different liver tumors in the same patient are often treated differently, a lesion-level response system provides better individual lesion assessment after LRT.
Performance of the LI-RADS TRA following Radiation-Based Therapies
As previously mentioned, radiation-treated HCC (SBRT or TARE) has expected posttreatment imaging features, including persistent APHE, a criterion historically used to identify viable disease. The presence of persistent APHE limits the utility of the current response assessment algorithms (LI-RADS TRA, mRECIST), as it leads to LR-TR viable categorization of successfully treated lesions. This could impact patient management as treated lesions showing response may be unnecessarily re-treated. Unfortunately, limited radiology-pathology correlation studies after radiation-based LRT and the unique mechanism of cell death between conventional (thermal ablation and intra-arterial embolization) and radiation-based LRTs complicates the use of the current LI-RADS TRA in patients undergoing radiation therapy for the treatment of HCC. Radiation induces cellular senescence; in other words, the tumor may still be viable and metabolically active but cannot replicate. Therefore, cell death evolves over time[22]. Thus, caution must be applied when using ‘viable’ categorization for persistently enhancing HCC after radiation therapy. Although the cells are still metabolically active, there is a different clinical implication as compared to ‘viable’ categorization after conventional LRTs.
SBRT and TARE are effective treatment options for down-staging and bridging to transplant[23-26], although the lack of prospective clinical trials for evaluation of survival outcomes continues to impart challenges in more widespread clinical adoption and inclusion in updated BCLC staging of this treatment. With that said, data from the LEGACY trial provided the impetus for inclusion of TARE into the updated BCLC 2022 staging system as a treatment option for HCC[27].
HCC treated with SBRT has variable appearances, although most commonly demonstrates APHE which can persist for one year or greater. A recent study assessed 56 SBRT-treated HCCs and found that the imaging appearance evolved over time, with 61% of tumors exhibiting persistent APHE and washout in the first 3-6 months posttreatment, which decreased over time[28]. Additionally, an increase in time from treatment showed an increasing loss of APHE post-SBRT (23% non-enhancing at 3 months versus 77% non-enhancing at 24 months)[28]. Hence, the presence of APHE after radiation therapy can be an expected imaging finding that does not necessarily suggest clinically relevant viable disease, in contrast to post-ablation and post-TACE, where posttreatment APHE is a strong predictor of tumor viability. In addition, successfully treated HCC usually demonstrates a stable to slow decrease in size after SBRT (89% decrease in size after 24 months)[28]. Lesions that progressed tended towards an increase in size post SBRT (11% at 24 months)[28]. Thus, loss of APHE and decrease in tumor size are gradual and expected findings of HCC treated with SBRT, whereas an increase in size or new intralesional APHE of the treated lesion should prompt diagnosis of local recurrence and warrant discussion at multidisciplinary conferences.
Literature review reveals one radiology-pathology concordance study evaluating the accuracy of the LI-RADS TRA for treatment response assessment following HCC treatment with SBRT[29]. In this study, posttreatment decrease in APHE correlated with nonviable tumors on explant, although persistent APHE following treatment was also seen in 45% of nonviable tumors on pathology[29]. Thus, the use of APHE alone to predict tumor viability is flawed after radiation treatment. While inter-reader agreement was fair (κ = 0.22), they found that the LI-RADS TRA can differentiate complete tumor necrosis (sensitivity 71-86%, specificity 85-96%, NPV = 85-96%) from incomplete tumor necrosis (sensitivity 88%-96%, specificity 71%-93%, PPV = 88%-92%) when LR-TR equivocal lesions were considered nonviable and viable respectively[29]. Of lesions classified as equivocal (n = 12/40), the majority [67% (8/12)] were found to be incompletely necrotic at histopathology[29]. Similar to the TARE data, this study also showed that a greater time until transplant following treatment resulted in an increasing loss of APHE (OR 0.68; 95%CI: 0.45-0.91, P = 0.03) and a greater degree of necrosis (OR 0.2; 95%CI: 0.04-0.79, P = 0.03)[29]. These findings suggest that the LI-RADS TRA correlates well with explant pathology findings and that radiated lesions classified as equivocal can undergo imaging follow-up rather than immediately undergoing retreatment, despite potentially harboring pathologically viable tumors as these will eventually demonstrate necrosis.
Similar to SBRT-treated HCC, there are variable imaging characteristics of HCC following TARE, including complete immediate posttreatment tumor necrosis to variable patterns of persistent intralesional APHE which can be seen up to one year or longer[30]. In one study, residual nodular APHE was seen in 61% of TARE-treated HCCs that had complete necrosis on pathology[13]. LI-RADS TRA has been shown to be a more accurate predictor of pathologic necrosis and overall treatment response compared to mRECIST following TARE[31]. Additionally, LI-RADS TRA correlates well with the histopathologic degree of necrosis when assessing HCC treated with TARE[32].
Evaluating the diagnostic performance of li-rads tra using ancillary features
LI-RADS TRA relies on only APHE and washout (major features) to evaluate tumor viability following LRT. Multiple radiology-pathology studies demonstrate the added value of AF on MRI (mild T2 weighted hyperintensity, diffusion restriction, and hepatobiliary phase hypointensity) in improving the sensitivity and specificity to detect viable tumor post-LRT. Inclusion of AF for treatment response assessment results in increased sensitivity for detecting viable tumor [84% (91/108)] compared to enhancement alone on CT [73% (79/108)] and MRI [76% (82/108)] without compromising specificity[20]. The addition of AF in LR-TR category adjustment also improved sensitivity for detecting incomplete necrosis without affecting specificity when using pathology as a gold standard for reference[33]. In this study, the sensitivity and specificity for detecting viable tumors using the LI-RADS TRA was 64.5% and 98%, while the addition of AF increased the sensitivity of detecting viable tumor to 86.9% with no difference in specificity (97%)[33]. In both studies, the presence of AF (mild to moderate T2 hyperintensity, restricted diffusion or hepatobiliary phase hypointensity) within regions of questionable APHE in a treated tumor with equivocal categorization was upgraded to viable[20,33]. Overall, these studies show a decrease in equivocal categorization when adding AF to assist in the evaluation of tumor viability.
Multiple additional studies have confirmed that the presence of AF improves the detection of tumor viability using the LI-RADS TRA. In one study of 181 HCCs, radiology-pathology correlation showed that the presence of hepatobiliary phase hypointensity in a lesion categorized as LR-TR viable or equivocal compared to LR-TR viable category alone showed a higher sensitivity for detection of viable tumor (65.6% vs. 57%) with no significant change in specificity (90.8% vs. 94.3%)[34]. Similarly, there was improved sensitivity when using DWI for viable disease detection as compared to LI-RADS TRA without AF (92% vs. 85%)[35]. With the addition of ancillary features into upcoming revisions of the LI-RADS TRA, MRI may become more beneficial for the detection of early small-volume viable tumors.
LI-RADS TRA: role of contrast-enhanced ultrasound
Recently, CEUS has been used to assess treatment response and detect local recurrence of HCC following LRT due to the high sensitivity and high temporal resolution offered by the modality. Studies have shown high sensitivity and specificity, approximately 80% and 100%, respectively, in assessing treatment response following ablation and TACE[36-38]. A recent meta-analysis demonstrated a sensitivity and specificity of 85% and 94%, respectively, for CEUS in the detection of residual tumor after LRT[39]. A handful of studies suggest that CEUS is superior to CECT in detecting viable tumor, including suggesting that CEUS has a higher sensitivity to assess residual APHE[40], better diagnostic performance for LI-RADS TRA, and improved sensitivity and accuracy in detection of viable tumor after lipiodol TACE[41].
One distinct advantage of CEUS is the real-time response assessment immediately after treatment. CEUS has shown increased sensitivity and specificity for detecting residual tumor compared to MRI performed less than 24 hours post-MWA of HCC (100% and 83% vs. 87% and 67%, respectively)[42]. Similarly, CEUS and CEMRI have demonstrated comparable sensitivity, specificity, and overall accuracy for detecting residual tumors with CEUS (86.5%, 98.3%, 95.7%) vs. CEMRI (84.6%, 98.9%, 95.7%) 1 month post ablation[43]. While there is currently no TRA utilizing CEUS for LRT-treated HCC, emerging evidence is promising and the release of a new algorithm is on the horizon. The upcoming CEUS TRA should be applied after thermal ablation or intraarterial embolic therapy. There is no evidence-based literature on the utility of CEUS after radiation therapy to HCC, and given expected post-treatment enhancement, CEUS would likely confound TRA.
Lipiodol as an Imaging Biomarker to Predict Treatment Response Assessment
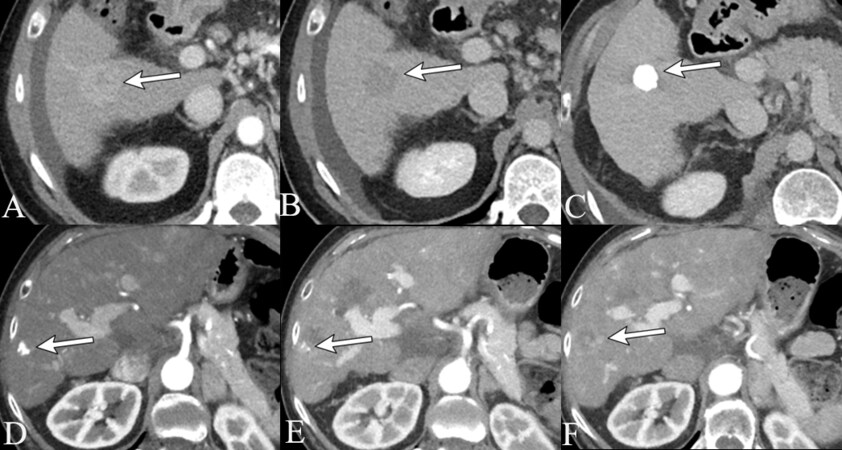
The radiopacity of lipiodol can be used as an imaging biomarker to predict necrosis and outcomes. Specific patterns of lipiodol distribution within and around a targeted tumor can serve as signs of excellent treatment response and have been shown to be associated with lower rates of early posttreatment recurrence[44-46]. Such patterns include increased density of lipiodol deposition, particularly in homogenous patterns, with deposition surrounding the radiographically visible margin of tumor in the normal parenchyma [Figure 7][44-46]. The duration of lipiodol deposition within a treated lesion is variable without consensus literature describing its expected time of resolution. However, enhancement is the main determinant of viability and the presence or absence of lipiodol is not considered a criterion for viability.
Figure 7. 56-year-old female with HCV cirrhosis presenting with LR 5 HCC [APHE (A) and washout (B)]. On immediate post-TACE CT, there is dense, homogenous, and complete staining of the targeted HCC (C), LR-TR nonviable. A second patient, 62-year-old male with alcohol and HCV cirrhosis, presents with focal area of staining within his treated tumor on immediate post-TACE imaging (D), LR-TR nonviable. 1 month after TACE, there is decreasing density of the lipiodol within the tumor and new irregular masslike enhancement at the 6-8 o’clock position, LR-TR viable (E). 3 months after lipiodol TACE there is extensive new and increasing irregular masslike enhancement both along the margin and within the treated tumor (F), LR-TR viable.
LIMITATIONS AND FUTURE DIRECTIONS
While emerging data on expected post-LRT imaging appearances and validity of the LI-RADS TRA in predicting necrosis is overall positive, there are a few key limitations that have become apparent. First, with the increasing use of radiation-based therapies, there is a need to modify the current algorithm to improve treatment response assessment based on persistent APHE seen after radiation treatment, a feature usually associated with tumor viability. This distinction is critical to prevent unnecessary retreatment of radiation-treated lesions. Second, multiple recent studies have demonstrated that AF can improve the sensitivity to detect viable tumor, which ultimately improves patient management. Third, the assessment of treatment response in HCC treated with a combination of LRT and systemic/biologic therapies must be developed, as they are not part of the current algorithm. Fourth, improved structured template reporting will be needed, given the increasing complexity of HCC treatment and posttreatment imaging appearances. This will increase standardization and concordance in image interpretation of this patient population across medical centers. Lastly, even with technological advances in imaging, there remain occult HCCs which may not be detected in the cirrhotic liver, usually with little effect on overall survival, but nonetheless important to understand when interpreting imaging.
CONCLUSION
As the incidence of HCC and the variety of LRTs have increased, treatment response assessment has become more complex. Posttreatment imaging evaluation is critical in guiding patient management, and thus it is essential to understand the imaging findings specific to each form of LRT. LI-RADS TRA uses a lesion-level approach to evaluate treatment response, and emerging evidence suggests this algorithm is both valid and reliable when evaluating treatment response after ablation and intra-arterial embolic therapies. However, LI-RADS TRA should be utilized with caution while evaluating treatment response after radiation therapies (TARE, SBRT), owing to the persistence of APHE within the treated tumor. Emerging data suggest that the use of AF in assessing treatment response improves sensitivity and specificity for detection of viable disease. This emerging evidence has allowed for changes to the current LI-RADS TRA, such that a new algorithm incorporating these changes has been approved by the LI-RADS treatment response working group, steering committee, and is awaiting approval from the American College of Radiology. Perhaps the biggest change is that the new algorithm will consist of a new system for evaluation of radiation-treated HCC. Additionally, AF will be incorporated into the TRA.
DECLARATIONS
Authors’ contributionsMade substantial contributions to conception and design, data analysis, and interpretation: Martin, M, Aslam A, Mubarak E, Hofley C, Lala K, Arora S, Madoff DC, Smith E, Owen D, Gabr A, Kim C, Parikh N, Stein E, Mervak B, Shampain K, Mendiratta-Lala M
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2023.
REFERENCES
1. Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the american association for the study of liver diseases. Hepatology 2018;68:723-50.
2. American College of Radiology Committee on LI-RADS® (Liver). The LI-RADS® v2018 Manual.Available from: https://www.acr.org/-/media/ACR/Files/Clinical-Resources/LIRADS/LI-RADS-2018-Manual-5Dec18.pdf [Last accessed on 24 May 2023].
3. Chaudhry M, McGinty KA, Mervak B, et al. The LI-RADS version 2018 MRI treatment response algorithm: evaluation of ablated hepatocellular carcinoma. Radiology 2020;294:320-6.
4. Shropshire EL, Chaudhry M, Miller CM, et al. LI-RADS treatment response algorithm: performance and diagnostic accuracy. Radiology 2019;292:226-34.
5. Seo N, Kim MS, Park MS, et al. Evaluation of treatment response in hepatocellular carcinoma in the explanted liver with liver imaging reporting and data system version 2017. Eur Radiol 2020;30:261-71.
6. Cools KS, Moon AM, Burke LMB, et al. Validation of the liver imaging reporting and data system treatment response criteria after thermal ablation for hepatocellular carcinoma. Liver Transpl 2020;26:203-14.
7. Aslam A, Do R, Chernyak V, Mendiratta-Lala M. LI-RADS imaging criteria for HCC diagnosis and treatment: emerging evidence. Current Hepatology Reports 2020;19:437-47.
8. Goldberg SN, Gazelle GS, Compton CC, Mueller PR, Tanabe KK. Treatment of intrahepatic malignancy with radiofrequency ablation: radiologic-pathologic correlation. Cancer 2000;88:2452-63.
9. Aslam A, Do RKG, Kambadakone A, et al. Hepatocellular carcinoma liver imaging reporting and data systems treatment response assessment: lessons learned and future directions. World J Hepatol 2020;12:738-53.
10. Voizard N, Cerny M, Assad A, et al. Assessment of hepatocellular carcinoma treatment response with LI-RADS: a pictorial review. Insights Imaging 2019;10:121.
11. Tian G, Yang S, Yuan J, et al. Comparative efficacy of treatment strategies for hepatocellular carcinoma: systematic review and network meta-analysis. BMJ Open 2018;8:e021269.
12. Brook OR, Thornton E, Mendiratta-Lala M, et al. CT imaging findings after stereotactic radiotherapy for liver tumors. Gastroenterol Res Pract 2015;2015:126245.
13. Riaz A, Kulik L, Lewandowski RJ, et al. Radiologic-pathologic correlation of hepatocellular carcinoma treated with internal radiation using yttrium-90 microspheres. Hepatology 2009;49:1185-93.
14. Zhang Y, Wang J, Li H, et al. Performance of LI-RADS version 2018 CT treatment response algorithm in tumor response evaluation and survival prediction of patients with single hepatocellular carcinoma after radiofrequency ablation. Ann Transl Med 2020;8:388.
15. Ormiston WEL, Yarmohammadi H, Lobaugh S, et al. Post-treatment CT LI-RADS categories: predictors of overall survival in hepatocellular carcinoma post bland transarterial embolization. Abdom Radiol 2021;46:3738-47.
16. Bartnik K, Podgórska J, Rosiak G, et al. Performance of initial LI-RADS 2018 treatment response in predicting survival of patients with hepatocellular carcinoma following TACE: a retrospective, single-center cohort study. J Cancer Res Clin Oncol 2021;147:3673-83.
17. Bartnik K, Podgórska J, Rosiak G, Korzeniowski K, Rowiński O. Inter-observer agreement using the LI-RADS version 2018 CT treatment response algorithm in patients with hepatocellular carcinoma treated with conventional transarterial chemoembolization. Abdom Radiol 2022;47:115-22.
18. Gupta P, Bansal A, Das GC, et al. Diagnostic accuracy of liver imaging reporting and data system locoregional treatment response criteria: a systematic review and meta-analysis. Eur Radiol 2021;31:7725-33.
19. Kierans AS, Najjar M, Dutruel SP, et al. Evaluation of the LI-RADS treatment response algorithm in hepatocellular carcinoma after trans-arterial chemoembolization. Clin Imaging 2021;80:117-22.
20. Park S, Joo I, Lee DH, et al. Diagnostic performance of LI-RADS treatment response algorithm for hepatocellular carcinoma: adding ancillary features to MRI Compared with enhancement patterns at CT and MRI. Radiology 2020;296:554-61.
21. Huh YJ, Kim DH, Kim B, Choi JI, Rha SE. Per-feature accuracy of liver imaging reporting and data system locoregional treatment response algorithm: a systematic review and meta-analysis. Cancers 2021;13:4432.
22. Jiao Y, Cao F, Liu H. Radiation-induced cell death and its mechanisms. Health Phys 2022;123:376-86.
23. Salem R, Johnson GE, Kim E, et al. Yttrium-90 radioembolization for the treatment of solitary, unresectable HCC: the LEGACY study. Hepatology 2021;74:2342-52.
24. Mathew AS, Atenafu EG, Owen D, et al. Long term outcomes of stereotactic body radiation therapy for hepatocellular carcinoma without macrovascular invasion. Eur J Cancer 2020;134:41-51.
25. Schaub SK, Hartvigson PE, Lock MI, et al. Stereotactic body radiation therapy for hepatocellular carcinoma: current trends and controversies. Technol Cancer Res Treat 2018;17:1533033818790217.
26. Mastrocostas K, Fischer S, Munoz-Schuffenegger P, et al. Radiological tumor response and histopathological correlation of hepatocellular carcinoma treated with stereotactic body radiation therapy as a bridge to liver transplantation. Abdom Radiol 2021;46:1572-85.
27. Reig M, Forner A, Rimola J, et al. BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol 2022;76:681-93.
28. Mendiratta-Lala M, Masch W, Owen D, et al. Natural history of hepatocellular carcinoma after stereotactic body radiation therapy. Abdom Radiol 2020;45:3698-708.
29. Mendiratta-Lala M, Aslam A, Maturen KE, et al. LI-RADS treatment response algorithm: performance and diagnostic accuracy with radiologic-pathologic explant correlation in patients with SBRT-treated hepatocellular carcinoma. Int J Radiat Oncol Biol Phys 2022;112:704-14.
30. Keppke AL, Salem R, Reddy D, et al. Imaging of hepatocellular carcinoma after treatment with yttrium-90 microspheres. AJR Am J Roentgenol 2007;188:768-75.
31. King MJ, Tong A, Dane B, Huang C, Zhan C, Shanbhogue K. Response assessment of hepatocellular carcinoma treated with yttrium-90 radioembolization: inter-reader variability, comparison with 3D quantitative approach, and role in the prediction of clinical outcomes. Eur J Radiol 2020;133:109351.
32. Vietti Violi N, Gnerre J, Law A, et al. Assessment of HCC response to Yttrium-90 radioembolization with gadoxetate disodium MRI: correlation with histopathology. Eur Radiol 2022;32:6493-503.
33. Kim SW, Joo I, Kim HC, et al. LI-RADS treatment response categorization on gadoxetic acid-enhanced MRI: diagnostic performance compared to mRECIST and added value of ancillary features. Eur Radiol 2020;30:2861-70.
34. Kim YY, Kim MJ, Yoon JK, Shin J, Roh YH. Incorporation of ancillary mri features into the LI-RADS treatment response algorithm: impact on diagnostic performance after locoregional treatment of hepatocellular carcinoma. AJR Am J Roentgenol 2022;218:484-93.
35. Yu JS, Kim JH, Chung JJ, Kim KW. Added value of diffusion-weighted imaging in the MRI assessment of perilesional tumor recurrence after chemoembolization of hepatocellular carcinomas. J Magn Reson Imaging 2009;30:153-60.
36. Meloni MF, Goldberg SN, Livraghi T, et al. Hepatocellular carcinoma treated with radiofrequency ablation: comparison of pulse inversion contrast-enhanced harmonic sonography, contrast-enhanced power Doppler sonography, and helical CT. AJR Am J Roentgenol 2001;177:375-80.
37. Choi D, Lim HK, Lee WJ, et al. Early assessment of the therapeutic response to radio frequency ablation for hepatocellular carcinoma: utility of gray scale harmonic ultrasonography with a microbubble contrast agent. J Ultrasound Med 2003;22:1163-72.
38. Kim CK, Choi D, Lim HK, et al. Therapeutic response assessment of percutaneous radiofrequency ablation for hepatocellular carcinoma: utility of contrast-enhanced agent detection imaging. Eur J Radiol 2005;56:66-73.
39. Hai Y, Savsani E, Chong W, Eisenbrey J, Lyshchik A. Meta-analysis and systematic review of contrast-enhanced ultrasound in evaluating the treatment response after locoregional therapy of hepatocellular carcinoma. Abdom Radiol 2021;46:5162-79.
40. Salvaggio G, Campisi A, Lo Greco V, et al. Evaluation of posttreatment response of hepatocellular carcinoma: comparison of ultrasonography with second-generation ultrasound contrast agent and multidetector CT. Abdom Imaging 2010;35:447-53.
41. Liu M, Lin MX, Lu MD, et al. Comparison of contrast-enhanced ultrasound and contrast-enhanced computed tomography in evaluating the treatment response to transcatheter arterial chemoembolization of hepatocellular carcinoma using modified RECIST. Eur Radiol 2015;25:2502-11.
42. Pregler B, Beyer LP, Wiesinger I, et al. Microwave ablation of large HCC lesions: added value of CEUS examinations for ablation success control. Clin Hemorheol Microcirc 2016;64:483-90.
43. Qu P, Yu X, Liang P, et al. Contrast-enhanced ultrasound in the characterization of hepatocellular carcinomas treated by ablation: comparison with contrast-enhanced magnetic resonance imaging. Ultrasound Med Biol 2013;39:1571-9.
44. Dioguardi Burgio M, Sartoris R, Libotean C, et al. Lipiodol retention pattern after TACE for HCC is a predictor for local progression in lesions with complete response. Cancer Imaging 2019;19:75.
45. Kim DY, Ryu HJ, Choi JY, et al. Radiological response predicts survival following transarterial chemoembolisation in patients with unresectable hepatocellular carcinoma. Aliment Pharmacol Ther 2012;35:1343-50.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Martin M, Aslam A, Mubarak E, Hofley C, Lala K, Arora S, Madoff DC, Smith E, Owen D, Gabr A, Kim C, Parikh N, Stein E, Mervak B, Shampain K, Mendiratta-Lala M. Imaging after liver-directed therapy: evidenced-based update of the LI-RADS treatment response algorithm. Hepatoma Res 2023;9:21. http://dx.doi.org/10.20517/2394-5079.2022.95
AMA Style
Martin M, Aslam A, Mubarak E, Hofley C, Lala K, Arora S, Madoff DC, Smith E, Owen D, Gabr A, Kim C, Parikh N, Stein E, Mervak B, Shampain K, Mendiratta-Lala M. Imaging after liver-directed therapy: evidenced-based update of the LI-RADS treatment response algorithm. Hepatoma Research. 2023; 9: 21. http://dx.doi.org/10.20517/2394-5079.2022.95
Chicago/Turabian Style
Martin, Marisa, Anum Aslam, Eman Mubarak, Cate Hofley, Kayli Lala, Sandeep Arora, David C. Madoff, Elainea Smith, Dawn Owen, Ahmed Gabr, Charles Kim, Neehar Parikh, Erica Stein, Benjamin Mervak, Kimberly Shampain, Mishal Mendiratta-Lala. 2023. "Imaging after liver-directed therapy: evidenced-based update of the LI-RADS treatment response algorithm" Hepatoma Research. 9: 21. http://dx.doi.org/10.20517/2394-5079.2022.95
ACS Style
Martin, M.; Aslam A.; Mubarak E.; Hofley C.; Lala K.; Arora S.; Madoff DC.; Smith E.; Owen D.; Gabr A.; Kim C.; Parikh N.; Stein E.; Mervak B.; Shampain K.; Mendiratta-Lala M. Imaging after liver-directed therapy: evidenced-based update of the LI-RADS treatment response algorithm. Hepatoma. Res. 2023, 9, 21. http://dx.doi.org/10.20517/2394-5079.2022.95
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 9 clicks
Cite This Article 9 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.