Lymph nodes of the perimandibular area: from anatomical classification to pathological role in cancer of the oral cavity, oropharynx and skin
Abstract
Lymph node status of the neck is the most important prognostic factor in head and neck cancer. Neck dissection, which consists of the systematic excision of the neck nodes, represents the gold standard of surgical treatment in clinically positive necks. In cases in which metastases to lymph nodes of the neck are not detectable, the decision to perform an elective neck dissection depends on the stage and the site of the primary tumor. This narrative review focuses on the anatomical description and oncological role of a group of lymph nodes of the neck that historically has not been well defined. Over the years, several authors have described the groups of lymph nodes that lie where the facial vein crosses the mandible, but to date, no unique definition or a clear view of their oncological role has been proposed. Recently, the term “perimarginal nodes” was coined to refer to this group of lymph nodes, and emphasis was placed on the risk of leaving them undissected during neck dissection. This paper aims to provide a surgical-anatomical classification of these lymph nodes and describe their oncological role on the basis of a review of the relevant literature.
Keywords
INTRODUCTION
Cervical lymph node status is the most important prognostic factor in head and neck cancer. Neck dissection (ND) is one of the key steps in the treatment of these cancers[1,2]. The history of ND begins in the 19th century when surgeons attempted to remove cervical lymph node disease en bloc at the same time as the primary cancer. The first systematic description offered by Jawdynski in 1888 and later popularized by Crile in the early 20th century formed the basis of the current techniques[3,4]. The technique has evolved over time, moving on to conservative ND (proposed by Suarez), selective ND, where only the nodal groups considered at greatest risk for metastasis from a given primary site are dissected, and superselective ND, defined as complete removal of all nodes and all fibrofatty tissue contents along the defined boundaries of one or two contiguous neck levels[1,5]. Over the years, the focus on preserving function and minimizing morbidity has made ND the far less invasive surgery that is widely employed today[1]. In 1998, in order to provide a standard nomenclature to guide ND, Robbins proposed a classification that divided the lymph nodes of the neck into levels and sublevels, a classification now adopted by all head and neck surgeons worldwide[6]. The submandibular triangle (or submaxillary or digastric triangle) corresponds to that region of the neck that is immediately below the body of the mandible. Classical anatomical descriptions indicate the upper limit of this area as the lower border of the body of the mandible and a line drawn from its angle to the mastoid process, while the lower limit is given by the anterior and posterior belly of the digastric muscle. The mylohyoid muscle and hyoglossal muscle form the floor of this triangle. The stylomandibular ligament divides the submandibular triangle into two parts[7]. In the Robbins classification, the submandibular triangle corresponds to level IB, even though the limits of the posterior part differ slightly; following the Robbins classification, level IB is bounded by the body of the mandible, the posterior belly of the digastric muscle, the stylohyoid muscle, and the anterior belly of the digastric muscle[6].
Within this triangle lies a group of lymph nodes whose anatomy and oncological role has only been clarified in recent years, the so-called “perimarginal nodes (PMN)”[8,9]. The aim of this paper is to review the anatomical description and oncological role of these lymph nodes. To this end, we carried out a PubMed search using the keywords “perimarginal nodes/lymph nodes” (2 results), “perifacial nodes/lymph nodes”
ANATOMY OF LYMPHATICS OF THE SUBMANDIBULAR AREA
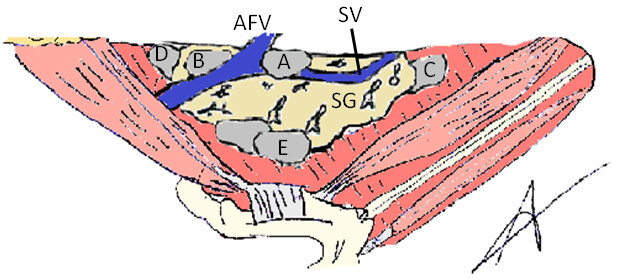
The first description of a constant node in the area where the facial artery crosses the horizontal branch of the mandible was made by the German anatomist and pathologist Hermann Stahr, and that description was later also reported in Henry Gray’s Anatomy[9,10]. In 1932, Henri Rouvière published his “Anatomie des lymphatiques de l’homme”, in which he precisely described the submandibular lymph nodes, dividing them into five groups (preglandular, prevascular, retrovascular, retroglandular, intraglandular)[11]. In his description, three to six lymph nodes were identified, with a number that was inversely proportional to their size. He described the preglandular group, delimited by the submandibular gland, the mandible and the anterior belly of the digastric muscle, and the retroglandular group that lies posterior to the submandibular gland, medial to and below the angle of the mandible. The group of prevascular and retrovascular lymph nodes consisted of lymph nodes defined in relation to the anterior facial vein (AFV), the former corresponding to the Stahr gland. Finally, he described the group of intracapsular submandibular lymph nodes consisting of lymph nodes within the submandibular gland[12,13]. In 1998, DiNardo revisited and refined Rouvière’s classification of the submandibular lymphatics, confirming the anatomist’s description but adding a sixth group of submandibular nodes, called deep submandibular nodes. These lymph nodes, when present, are small and are found on the deep surface of the submandibular gland. They are superficial to the mylohyoid muscle or posterior to the hyoglossal muscle[14]. This classification has been used in the recent surgical oncology literature, such as the study by Dhiwakar et al. which attempted to determine whether all lymph nodes in sublevel IB could be oncologically safely extirpated without removing the submandibular gland[15]. [Figure 1]
Figure 1. Lymph nodes of the submandibular area according to Rouviere’s classification. AVF: Anterior Facial Vein; SM: submandibular Vein; SG: submandibular Gland; A: prevascular node a.k.a. Node of Stahr; B: retrovascular node; C: preglandular node; D: retroglandular node; E: intraglandular nodes. A+B aka Perifacial nodes; A+B+C+D aka Perimarginal nodes.
PERIFACIAL NODES
The retrovascular and prevascular lymph nodes are also defined by some authors as perifacial nodes (PFN), because of their relation to the AVF. Despite the similar name, these nodes do not belong to the facial node group. Facial nodes were classified by Rouvière into four groups: inferior maxillary, buccinator, infraorbital (nasolabial), and malar[10]. They lie above the inferior limit of the mandible, whereas the PFN, being below this limit, must be considered part of level IB[13]. According to the literature, the PFN drain from the oral mucosa, oropharyngeal mucosa and the skin and subcutaneous tissue of the face[2,16]. Few studies have investigated the role of the PFN in head and neck cancer, and some of them consider the PFN as a different group of lymph nodes. Creighton et al. tried to determine the frequency of nodal metastases from skin malignancy (melanoma 63.5%, squamous cell carcinoma 20.1%) of the head and neck in non-traditional lymph node stations. In his study, the PFN are considered a non-traditional nodal group and were distinguished from levels of the neck[17]. The primary tumors were located in the scalp, forehead, cheek, ear, nose, periocular area and lip, and PFN metastases were present in 10/145 (6.9%) of cases, especially when the primary tumor was located in the nose (3/7; 42.9%) and lip (2/6; 33.3%), but also in the forehead, scalp and cheek. The study concluded that dissection of the PFN should be performed in all elective and completion lymphadenectomies for primary malignancies of the nose and lips[17]. In a study aiming to identify factors associated with recurrence of squamous cell carcinoma (SCC) involving the temporal bone, McRackan et al. described the PFN as a different group and concluded that, as compared to cervical lymph node involvement, involvement of the PFN was not associated with an increased risk of recurrence[18]. Additionally, Scurry et al. considered the PFN to be a different node group. In their systematic review assessing whether the regional recurrence of nasal cavity SCC was higher than previously suspected, they reported a rate of 18.1% and recommended that patients with intranasal SCC and additional high-risk characteristics should be treated with ND or radiotherapy, suggesting that the PFN region should be treated with radiotherapy because of the difficulty and potential morbidity of surgical dissection in that area[19]. In a retrospective study, Lim et al. investigated the incidence of metastases to the PFN[2]. They considered the PFN as nodal pads that lie anterior or posterior to the AFV on top of the facial artery in the submandibular gland triangle. Patients with oral or oropharyngeal SCC and with clinically node-positive necks were included. The incidence of PFN metastases was 10 (15%) cases. In 35% of them, the primary lesion was in the oral cavity, while in 8%, it was located in the oropharynx. Seven of 63 (11%) cases, which had no clinically positive lymph nodes in level I, had PFN metastases, of which 4/15 (27%) were from an oral cavity primary cancer and 3/48 (6%) were from an oropharyngeal primary[2].
In another study, Lim et al. analyzed the incidence of occult metastasis in the PFN and nodal recurrence in these nodal pads in SCC of the tongue and floor of mouth[16]. They found that 4/72 (5.5%) patients with tongue cancer and 2/27 (7.4%) patients with the floor of mouth cancer had a positive metastatic PFN node, with an incidence of regional recurrence at level I of 3 in 45 (6.7%)[16]. Agarwal et al. studied the incidence of isolated PFN metastasis in 231 oral SCC patients who had a clinically negative neck[20]. The primary tumor was located in the buccal mucosa in 116/231 (50.2%) and in the oral tongue in 84/231 (36.36%). Nineteen of 231 (8.22%) patients had ipsilateral isolated PFN metastasis, but the incidence did not differ between oral tongue (6/84; 7.1%) and buccal mucosa (9/116; 7.7%). In his series, the incidence of isolated PFN was statistically significant in patients with cancers stage T3 and T4[20].
PREGLANDULAR NODES
The preglandular nodes are the other subgroup of submandibular nodes identified by Rouvière that is of particular scientific interest. The preglandular nodes are those nodes situated in the triangular space bounded posteriorly by the submandibular gland, superiorly by the mandible and inferiorly and anteriorly by the anterior belly of the digastric muscle. Frequently, the preglandular nodes are in contact with the submental vein and embedded in fibrofatty tissue above the mylohyoid muscle[14]. Ballenger, in his milestone textbook “Otolaryngology Head & Neck Surgery” describes the preglandular nodes as a group of submandibular triangle nodes that serve as the primary drainage site for cancers of the buccal and lingual mucosa. Indeed, the superficial lymphatic vessels of the mouth floor and gingival system connect with each other before draining into the preglandular nodes. Ballenger also states that the deep collecting system drains into the preglandular nodes before draining into the subdigastric nodes[21]. In 2003, Abe et al. analyzed 90 formalin-fixed cadaveric specimens in order to study the lymph vessels of the submandibular nodes[22]. Afferent vessels were not always identified, while efferent vessels were a constant finding. In 19/20 (95%) specimens, collecting vessels appearing on the mylohyoid surface and emptying into the pregandular nodes were identified. The authors demonstrated how the collecting vessel system was still unclear, but in some specimens, they described direct lymphatic drainage vessels which originate from the oral region and pass through the mylohyoid muscle before draining into the preglandular nodes[22]. Few studies have addressed the specific incidence of metastasis to the preglandular lymph nodes; DiNardo found metastases in preglandular nodes in 4/41 (9.8%) patients who had SCC of the floor of mouth[14].
PERIMARGINAL NODES
In 2018, a prospective study by our group described a group of submandibular nodes at risk of being left undissected during ND performed with the Hayes Martin maneuver[13]. The study recruited 47 patients (for a total of 62 neck dissections) with oral, oropharyngeal and facial skin SCC with clinically negative necks. Following the classical steps of ND, they dissected the AFV until they reached the inferior border of the mandible. All nodes lying adjacent to the AFV within 1 to 2 cm below the mandibular border that were superficial to or contained within the superficial cervical fascia were considered nodes at risk and were all removed separately from the ND specimen. To avoid injury to the marginal mandibular nerve, the dissection was performed with the support of nerve integrity monitoring[13,23,24]. In 84% of specimens, they found at least one node that would have been left undissected if the Hayes Martin maneuver had been performed[13]. The mean greatest diameter of these nodes was 12.5 mm; no other studies have ever described the size of nodes in this area. In 76% of cases, only one node would have been left; in 19%, 2 nodes and in 5%, 3 nodes. The average number of PFN described by our group was 1.6 (range 0-5), that is, lower than the 2.1 (range 0 - 8) reported by Lim et al. One of the most important findings of the study is that, owing to the AFV anatomical variables relative to the submandibular gland, Rouvière’s classical distinction between
Perimarginal nodes in oral cancer
In 2019, Tirelli et al. assessed the incidence of PMN metastasis from oral cavity SCC. Thirty-nine patients affected by oral cancer were included and PMN metastases were found in 8 patients (20.5%)[8]. Extranodal extension, a well-known predictor of poor prognosis, was present in 2 of 8 cases (25%) in which the PMN were involved[8,25]. Five of 39 (12.8%) patients had only PMN metastases, consistent with the findings of Agarwal et al., who identified isolated PFN metastases in 19 /231 patients (8.2%)[20]. No patient or primary tumor characteristics were found to correlate with a higher risk of PMN metastases. The same trend was later confirmed in a larger study by the same group (17.5%)[7]. In this later study, a significant correlation was found between PMN involvement and the upper zone of the oral cavity (P < 0.001). Even though no statistical correlation was found between primary tumor or patient characteristics and PMN metastases, in both of these studies by Tirelli, a trend of increasing incidence of metastasis in high-grade primary tumors was appreciated[8,9]. This finding is in agreement with the findings of Agarwal et al. who reported a significantly higher rate of PFN metastases in patients with T3 and T4 stage oral cavity SCC[20].
These findings seem to indicate that the only characteristics of the primary tumor that correlate with an increased incidence of PMN metastases are a high grade (mild correlation) and the site of origin of the tumor. It has indeed been shown - although the finding has yet to be confirmed by larger patient series - that tumors originating from the upper oral cavity are more likely to metastasize to the PMN compared with tumors of the lower oral cavity[8,9,16]. This apparently unexpected finding may be accounted for by the lymphatic drainage routes of the oral cavity. While the lower parts of the mouth (tongue, floor of mouth,
Studies reporting the number of perimarginal (aka peripheral) lymph nodes involved in metastases
| Study design | Number of patients included | Number of cases with PMN/PFN nodes involved | Oral cancer | Oropharyngeal cancer | Skin cancer | Lip cancer | CUP | |
| DiNardo[14] | Prospective study | 41 | 16/41 (39%) | 16/41 (39%) | - | - | - | - |
| Netterville et al.,[29] | Retrospective study | 13 | 12/13 (92.3%) | - | - | 12/13 (92.3%) | - | - |
| Lim et al.,[2] | Retrospective study | 66 | 10/66 (15%) | 6/17 (35%) | 4/49 (8%) | - | - | - |
| Creighton et al.,[17] | Retrospective study | 145 | 10/145 (6.9%) | - | - | 8/139 (5.8%) | 2/6 (33.3%) | |
| Agarwal et al.,[20] | Prospective study | 231 | 19/231 (8.2%) | 19/231 (8.2%) | - | - | - | - |
| Tirelli et al.,[8] | Prospective study | 39 | 8/39 (20.5%) | 8 (20.5%) | - | - | - | - |
| Tirelli et al.,[9] | Prospective study | 136 | 19/136 (14%) | 15/86 (17.4%) | 0/31 (0%) | 1/8 (12.5%) | 3/6 (50%) | 0/5 (0%) |
Perimarginal nodes in oropharyngeal cancer
The incidence of metastases to submandibular nodes from oropharyngeal SCC is known to be very low, and indeed, the guidelines on elective ND in oropharyngeal cancers do not consider level IB dissection to be mandatory[27]. In detail, three articles in the literature have analyzed the incidence of oropharyngeal cancer metastases to the PMN. In the retrospective study of Lim et al., the majority of patients included (49/66, 74%) had an oropharyngeal tumor, and metastases to the PFN were found in 4/49 (8%)[2]. This finding is in contrast with the report of Riffat et al. who retrospectively analyzed recurrences within the PFN region from 2004 to 2009 in patients with oropharyngeal SCC who underwent ND without systematic removal of the PFN[28]. Similarly, in a recent study by our group, assessing the prevalence of PMN metastasis from various primaries, oropharyngeal SCC was not found to have metastasized to the PMN in any of the 31 patients included (0%)[9]. In the same study, no metastases were detected in the small subset of patients, in whom the PMN were removed during ND for cancer of unknown primary. However, this is not surprising as it is well known that head and neck cancers classified as “unknown primary” almost always originate from the oropharynx[9]. Despite these apparently conflicting results, it should be noted that in
Perimarginal nodes in skin SCC
Although the involvement of the PMN by SCC of the skin has been reported, the numbers are low.
Perimarginal nodes in lip SCC
Although the involvement of level IB lymph nodes by lip cancer is well known, only one study specifically analyzed the prevalence of PMN metastases from SCC in this area. Tirelli et al. demonstrated an incidence of metastasis in 3/6 (50%) patients with primary lip cancer[9]. Also in this case, it has to be noted that the lip tumors drain through lymphatics close to the course of the labial arteries that drain directly into the AFV’s lymphatic system.
RADIOLOGICAL ASPECTS
Radiological examination of the cervicolateral nodes has a fundamental role in head and neck cancer, and ultrasound is a highly useful imaging modality in this setting. As reported by many authors, ultrasound has high accuracy and sensitivity and is also inexpensive, especially when compared with other imaging techniques such as MRI and CT[30-32]. Additionally, several studies have demonstrated that ultrasound and CT have similar effectiveness[33-36]. The choice between CT and MRI for the study of the cervical lymph nodes has been addressed by several investigations, at times with conflicting results[36-41]. Whenever possible, these modalities should be used in combination to obtain the most effective and reliable results[42]. In DiNardo’s study, the role of imaging for the detection of submandibular metastases from oral cavity cancers was still unclear. CT and MRI appear to be the most commonly used techniques for the detection of lymph nodes and assessment of their size and features in metastatic disease[14,43,44]. However, some studies have failed to demonstrate their effectiveness in providing an imaging assessment of level IB; in Carvalho et al.’s study, for example, despite CT having high accuracy, sensitivity and specificity in the detection of laterocervical metastases, its only false negative results were found in the submandibular region[45]. A study by Chaukar et al. analyzed 70 patients with oral SCC and N0, who subsequently underwent neck dissection[46]. The patients were studied with PET/CT, CT and ultrasound. The results show that for level IB CT performed better in terms of specificity and accuracy compared with the other two modalities: CT specificity was 86% compared with 72% for ultrasound and 71% for PET/CT, whereas its accuracy for level IB was 81%, compared with 73% and 69% for ultrasound and PET/CT, respectively[46]. These findings are consistent with those of Jank et al., who compared the sensitivity and specificity of ultrasound and CT for various laterocervical nodal levels in occult metastases from head and neck SCC[47]. Here, the sensitivity of ultrasound for level I was 80%, compared with 38% of CT, whereas specificity was 92% for CT and 80% for ultrasound[47].
SURGICAL IMPLICATIONS
Over half of the patients with head and neck SCC experience locoregional recurrence, which is associated with poor outcomes, and only about 10%-15% of patients who have locoregional relapses can be salvaged[48]. In the clinical experience of head and neck surgeons, the occurrence of relapses in the perimandibular area is not infrequent, and distinguishing between nodal or local relapses is often not easy. These relapses are challenging to treat and frequently require the sacrifice of a portion of the mandible. PMN metastasis is often undetectable due to the fact that they tend to be micrometastases that go unnoticed in routine clinical and radiological examination. The data therefore suggest that they should be removed in all cases undergoing elective ND for cancers of the oral cavity. [Table 2]
Levels indicated for elective neck dissection according to primary tumor site
| Site of primary cancer | Neck levels according to Robbins et al.,[54] | Indication for dissection of perimarginal nodes |
| Oral cavity | I-III | Yes |
| Lip | I - III | Yes |
| Oropharynx | II-IV | No |
| Skin of the head - Area along the course of the facial vein | I-III, parotid and facial nodes | Yes |
| Skin of the head - Other subsites - Posterior scalp and Upper neck | II-V, suboccipital and postauricolar nodes | Not enough data/No scientific evidence |
| Skin of the head - Other subsites - Preauricolar, Anterior scalp and Temporal region | I-III, parotid and facial nodes | Not enough data/No scientific evidence |
The main reason why these lymph nodes are traditionally not routinely excised during elective ND is the risk of injury to the marginal mandibular nerve[13]. Marginal mandibular nerve injury is a complication that causes an aesthetic defect that greatly impacts the patient’s quality of life, often resulting in medicolegal actions. Many surgical recommendations and techniques have been adopted over the years, but none of them has been able to totally prevent nerve damage[23,49,50]. The most widespread technique during ND is the Hayes Martin maneuver which, however, is oncologically unsafe and should be avoided during oncological surgery[13,51].
Since PMN metastasis mainly concerns oral cavity tumors, mention should be made of their possible involvement during the sentinel node biopsy procedure. While not yet universally accepted, sentinel node biopsy is now incorporated in many national guidelines also for early stage oral cavity SCC[52]. Although some papers have reported the presence of positive sentinel nodes at level IIB, it should be noted that the position of the PMN may hinder the detection of such nodes during the procedure because of the shine-through phenomenon, particularly if the primary tumor is located in the lower oral cavity (floor of mouth, tongue, inferior alveolar ridge)[53]. A recent study indeed suggests routinely removing level IB, or at least the preglandular triangle, in the floor of mouth tumors even when the sentinel node biopsy is negative, on account of the increased risk of false negative results due to the shine-through phenomenon[52].
CONCLUSIONS
Based on our review of the literature, it is imperative to remove the PMN during ND in all cases of treatment for oral cavity and lip cancer, regardless of location, tumor stage and neck status. In addition, their rare involvement in oropharyngeal cancer suggests that removal of the PMN is not mandatory in these cases and should be avoided due to the risk of injury to the marginal mandibular nerve. Moreover, their removal should also be considered in facial skin SCC, especially when the tumor originates along the course of the AFV. Future research on larger series of facial skin SCC will help to further assess the correlation between the facial region involved by the tumor and metastases to the PMN. Further studies with a long-term follow-up are needed to verify whether PMN removal could lead to a reduction in locoregional relapses and an increase in survival.
DECLARATIONS
AcknowledgmentsThe authors thank Itala Mary Ann Brancaleone, MA, RSA Dip TEFLA, teacher of Medical English at the University of Trieste, for her support in editing the manuscript.
Authors’ contributionsWriting, review, and revision: Tirelli G, Uderzo F, Gardenal N, Boscolo-Rizzo P, Marcuzzo AV
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declare that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2023.
REFERENCES
1. Ferlito A, Rinaldo A, Robbins KT, Silver CE. Neck dissection: past, present and future? J Laryngol Otol 2006;120:87-92.
2. Lim YC, Lee JS, Choi EC. Perifacial lymph node metastasis in the submandibular triangle of patients with oral and oropharyngeal squamous cell carcinoma with clinically node-positive neck. Laryngoscope 2006;116:2187-90.
3. Ferlito A, Rinaldo A, Silver CE, et al. Neck dissection: then and now. Auris Nasus Larynx 2006;33:365-74.
4. Rinaldo A, Ferlito A, Silver CE. Early history of neck dissection. Eur Arch Otorhinolaryngol 2008;265:1535-8.
5. Suárez C, Rodrigo JP, Robbins KT, et al. Superselective neck dissection: rationale, indications, and results. Eur Arch Otorhinolaryngol 2013;270:2815-21.
6. Robbins KT. Classification of neck dissection: current concepts and future considerations. Otolaryngol Clin North Am 1998;31:639-55.
7. Gray H. Anatomy of the human body, 26th ed. Philadelphia, PA: Lea & Febiger; 1954.
8. Tirelli G, Gatto A, Marcuzzo AV. Perimarginal lymph nodes: an undervalued entity in oral cancer. Eur Arch Otorhinolaryngol 2019;276:1147-51.
9. Tirelli G, Bussani R, Marchiori V, Gardenal N, Boscolo-Rizzo P, Marcuzzo AV. Relevance of perimarginal nodes for head and neck cancer. Eur Arch Otorhinolaryngol 2022;279:2603-9.
10. Iwanaga J, Lofton C, He P, Dumont AS, Tubbs RS. Lymphatic system of the head and neck. J Craniofac Surg 2021;32:1901-5.
11. Sheahan P, Colreavy M, Toner M, Timon CV. Facial node involvement in head and neck cancer. Head Neck 2004;26:531-6.
13. Tirelli G, Marcuzzo AV. Lymph nodes of the perimandibular area and the hazard of the hayes martin maneuver in neck dissection. Otolaryngol Head Neck Surg 2018;159:692-7.
14. DiNardo LJ. Lymphatics of the submandibular space: an anatomic, clinical, and pathologic study with applications to floor-of-mouth carcinoma. Laryngoscope 1998;108:206-14.
15. Dhiwakar M, Ronen O, Malone J, et al. Feasibility of submandibular gland preservation in neck dissection: a prospective anatomic-pathologic study. Head Neck 2011;33:603-9.
16. Lim YC, Kim JW, Koh YW, et al. Perivascular-submandibular lymph node metastasis in squamous cell carcinoma of the tongue and floor of mouth. Eur J Surg Oncol 2004;30:692-8.
17. Creighton F, Bergmark R, Emerick K. Drainage patterns to nontraditional nodal regions and level IIB in cutaneous head and neck malignancy. Otolaryngol Head Neck Surg 2016;155:1005-11.
18. McRackan TR, Fang TY, Pelosi S, et al. Factors associated with recurrence of squamous cell carcinoma involving the temporal bone. Ann Otol Rhinol Laryngol 2014;123:235-9.
19. Scurry WC Jr, Goldenberg D, Chee MY, Lengerich EJ, Liu Y, Fedok FG. Regional recurrence of squamous cell carcinoma of the nasal cavity: a systematic review and meta-analysis. Arch Otolaryngol Head Neck Surg 2007;133:796-800.
20. Agarwal SK, Arora SK, Kumar G, Sarin D. Isolated perifacial lymph node metastasis in oral squamous cell carcinoma with clinically node-negative neck. Laryngoscope 2016;126:2252-6.
21. . Wackym Ashley P, Snow James B, Ballenger’s otorhinolaryngology: head and neck surgery, 18th ed. USA: PMPH-USA; 2016.
22. Abe M, Murakami G, Noguchi M, Yajima T, Kohama GI. Afferent and efferent lymph-collecting vessels of the submandibular nodes with special reference to the lymphatic route passing through the mylohyoid muscle. Head Neck 2003;25:59-66.
23. Tirelli G, Bergamini PR, Scardoni A, Gatto A, Boscolo Nata F, Marcuzzo AV. Intraoperative monitoring of marginal mandibular nerve during neck dissection. Head Neck 2018;40:1016-23.
24. Marcuzzo AV, Šuran-Brunelli AN, Dal Cin E, et al. Surgical anatomy of the marginal mandibular nerve: a systematic review and meta-analysis. Clin Anat 2020;33:739-50.
25. Tirelli G, de Groodt J, Sia E, et al. Accuracy of the anatomage table in detecting extranodal extension in head and neck cancer: a pilot study. J Med Imaging 2021;8:014502.
26. Malik A, Joshi P, Mishra A, et al. Prospective study of the pattern of lymphatic metastasis in relation to the submandibular gland in patients with carcinoma of the oral cavity. Head Neck 2016;38:1703-7.
27. Sanguineti G, Califano J, Stafford E, et al. Defining the risk of involvement for each neck nodal level in patients with early T-stage node-positive oropharyngeal carcinoma. Int J Radiat Oncol Biol Phys 2009;74:1356-64.
28. Riffat F, Buchanan MA, Mahrous AK, Fish BM, Jani P. Oncological safety of the Hayes-Martin manoeuvre in neck dissections for node-positive oropharyngeal squamous cell carcinoma. J Laryngol Otol 2012;126:1045-8.
29. Netterville JL, Sinard RJ, Bryant GL, Burkey BB. Delayed regional metastasis from midfacial squamous carcinomas. Head Neck 1998;20:328-33.
30. Ashraf M, Biswas J, Jha J, et al. Clinical utility and prospective comparison of ultrasonography and computed tomography imaging in staging of neck metastases in head and neck squamous cell cancer in an Indian setup. Int J Clin Oncol 2011;16:686-93.
31. Jhony JK, Pg B, Patil S, Mk S, George NA. A prospective observational study to determine the correlation of clinical, ultrasonography, and pathological examination of cervical lymph nodal staging in oral squamous cell carcinoma. Indian J Surg Oncol 2021;12:512-6.
32. Sumi M, Ohki M, Nakamura T. Comparison of sonography and CT for differentiating benign from malignant cervical lymph nodes in patients with squamous cell carcinoma of the head and neck. AJR Am J Roentgenol 2001;176:1019-24.
33. Rottey S, Petrovic M, Bauters W, et al. Evaluation of metastatic lymph nodes in head and neck cancer: a comparative study between palpation, ultrasonography, ultrasound-guided fine needle aspiration cytology and computed tomography. Acta Clin Belg 2006;61:236-41.
34. Sarvanan K, Bapuraj JR, Sharma SC, Radotra BD, Khandelwal N, Suri S. Computed tomography and ultrasonographic evaluation of metastatic cervical lymph nodes with surgicoclinicopathologic correlation. J Laryngol Otol 2002;116:194-9.
35. Akoğlu E, Dutipek M, Bekiş R, Değirmenci B, Ada E, Güneri A. Assessment of cervical lymph node metastasis with different imaging methods in patients with head and neck squamous cell carcinoma. J Otolaryngol 2005;34:384-94.
36. Shetty D, Jayade BV, Joshi SK, Gopalkrishnan K. Accuracy of palpation, ultrasonography, and computed tomography in the evaluation of metastatic cervical lymph nodes in head and neck cancer. Indian J Dent 2015;6:121-4.
37. Atula TS, Varpula MJ, Kurki TJ, Klemi PJ, Grénman R. Assessment of cervical lymph node status in head and neck cancer patients: palpation, computed tomography and low field magnetic resonance imaging compared with ultrasound-guided fine-needle aspiration cytology. Eur J Radiol 1997;25:152-61.
38. Curtin HD, Ishwaran H, Mancuso AA, Dalley RW, Caudry DJ, McNeil BJ. Comparison of CT and MR imaging in staging of neck metastases. Radiology 1998;207:123-30.
39. King AD, Tse GM, Yuen EH, et al. Comparison of CT and MR imaging for the detection of extranodal neoplastic spread in metastatic neck nodes. Eur J Radiol 2004;52:264-70.
40. Madison MT, Remley KB, Latchaw RE, Mitchell SL. Radiologic diagnosis and staging of head and neck squamous cell carcinoma. Otolaryngol Clin North Am 1998;31:727-54.
41. Rumboldt Z, Gordon L, Gordon L, Bonsall R, Ackermann S. Imaging in head and neck cancer. Curr Treat Options Oncol 2006;7:23-34.
42. Haberal I, Celik H, Göçmen H, Akmansu H, Yörük M, Ozeri C. Which is important in the evaluation of metastatic lymph nodes in head and neck cancer: palpation, ultrasonography, or computed tomography? Otolaryngol Head Neck Surg 2004;130:197-201.
44. Don DM, Anzai Y, Lufkin RB, Fu YS, Calcaterra TC. Evaluation of cervical lymph node metastases in squamous cell carcinoma of the head and neck. Laryngoscope 1995;105:669-74.
45. Carvalho P, Baldwin D, Carter R, Parsons C. Accuracy of CT in detecting squamous carcinoma metastases in cervical lymph nodes. Clin Radiol 1991;44:79-81.
46. Chaukar D, Dandekar M, Kane S, et al. Relative value of ultrasound, computed tomography and positron emission tomography imaging in the clinically node-negative neck in oral cancer. Asia Pac J Clin Oncol 2016;12:e332-8.
47. Jank S, Robatscher P, Emshoff R, Strobl H, Gojer G, Norer B. The diagnostic value of ultrasonography to detect occult lymph node involvement at different levels in patients with squamous cell carcinoma in the maxillofacial region. Int J Oral Maxillofac Surg 2003;32:39-42.
48. Borsetto D, Sethi M, Polesel J, et al. The risk of recurrence in surgically treated head and neck squamous cell carcinomas: a conditional probability approach. Acta Oncol 2021;60:942-7.
49. Batstone MD, Scott B, Lowe D, Rogers SN. Marginal mandibular nerve injury during neck dissection and its impact on patient perception of appearance. Head Neck 2009;31:673-8.
50. Al-Qahtani K, Mlynarek A, Adamis J, Harris J, Seikaly H, Islam T. Intraoperative localization of the marginal mandibular nerve: a landmark study. BMC Res Notes 2015;8:382.
51. Murthy SP, Paderno A, Balasubramanian D. Management of the marginal mandibular nerve during and after neck dissection. Curr Opin Otolaryngol Head Neck Surg 2019;27:104-9.
52. de Bree R, de Keizer B, Civantos FJ, et al. What is the role of sentinel lymph node biopsy in the management of oral cancer in 2020? Eur Arch Otorhinolaryngol 2021;278:3181-91.
53. Zeeuw M, Mahieu R, de Keizer B, de Bree R. Evaluation of a streamlined sentinel lymph-node imaging protocol in early-stage oral cancer. Ann Nucl Med 2021;35:1353-60.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Tirelli G, Uderzo F, Gardenal N, Boscolo-Rizzo P, Marcuzzo AV. Lymph nodes of the perimandibular area: from anatomical classification to pathological role in cancer of the oral cavity, oropharynx and skin. J Cancer Metastasis Treat 2023;9:20. http://dx.doi.org/10.20517/2394-4722.2022.98
AMA Style
Tirelli G, Uderzo F, Gardenal N, Boscolo-Rizzo P, Marcuzzo AV. Lymph nodes of the perimandibular area: from anatomical classification to pathological role in cancer of the oral cavity, oropharynx and skin. Journal of Cancer Metastasis and Treatment. 2023; 9: 20. http://dx.doi.org/10.20517/2394-4722.2022.98
Chicago/Turabian Style
Tirelli, Giancarlo, Francesco Uderzo, Nicoletta Gardenal, Paolo Boscolo-Rizzo, Alberto Vito Marcuzzo. 2023. "Lymph nodes of the perimandibular area: from anatomical classification to pathological role in cancer of the oral cavity, oropharynx and skin" Journal of Cancer Metastasis and Treatment. 9: 20. http://dx.doi.org/10.20517/2394-4722.2022.98
ACS Style
Tirelli, G.; Uderzo F.; Gardenal N.; Boscolo-Rizzo P.; Marcuzzo AV. Lymph nodes of the perimandibular area: from anatomical classification to pathological role in cancer of the oral cavity, oropharynx and skin. J. Cancer. Metastasis. Treat. 2023, 9, 20. http://dx.doi.org/10.20517/2394-4722.2022.98
About This Article
Special Issue
Copyright
Data & Comments
Data

 Cite This Article 11 clicks
Cite This Article 11 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.