An analysis of the role of targeted muscle reinnervation (TMR) in quality of life and pain outcomes: a case series
Abstract
Aim: Targeted muscle reinnervation (TMR) surgery has fundamentally changed the management of patients who have suffered or are about to undergo amputation. Providing nerve stumps with a muscle target has been shown to have profound effects on levels of post-amputation pain in relation to phantom limb pain (PLP) and neuroma pain (NP). The primary objective of this report was to quantify pain parameters for this population and to measure the impact on health-related quality of life (HRQol) before and after TMR surgery. In this case series, we evaluate the role of TMR in addressing both pain and the impact of the surgery on the patient’s quality of life.
Methods: A retrospective analysis of 15 upper limb amputee patients who underwent TMR by the Relimb Unit in London, UK. Participants’ perceptions of pain were determined using the 11-point numerical (Pain) rating scale (NRS) and HRQoL was calculated using the Euroqol EQ-5D-5L questionnaire at two time points, comparing both pain and perceived quality of life pre and post surgery. The Wilcoxon Signed Rank Test was used for the NRS data and a paired sample t-test was used for the EQ-VAS data.
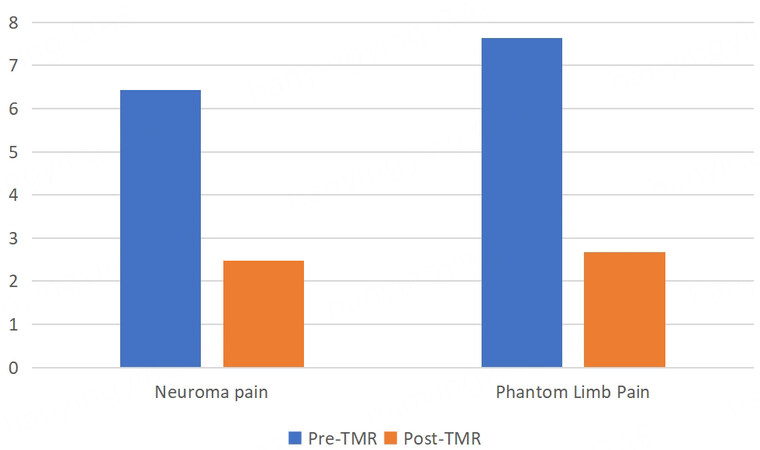
Results: A total of 15 patients completed the evaluation. We observed statistically significant reductions in both PLP (pre-operative mean: 7.6, post-operative mean: 2.7, P < 0.05) and NP (pre-operative mean: 6.4, post-operative mean: 2.5, P < 0.05) in these patients. Similarly, HRQoL observed on the EQ-VAS scale demonstrated a significant improvement in quality of life, from 68 pre-operatively to 78 post-procedure (P < 0.05).
Conclusion: This is the first quantified evaluation of changes in HRQoL after TMR surgery for upper limb amputation. There appears to be a significant improvement in both HRQoL and overall perception of pain. This finding may have important implications for funding and national resource allocation for TMR surgery.
Keywords
INTRODUCTION
There are an estimated 10,000 upper limb amputations annually in the United Kingdom[1]; most are digital amputations, with approximately 300 major limb amputations (e.g., transhumeral or transradial). The adverse impact of an upper limb amputation on mental health and pain is well established[2]. There are additional functional sequelae associated with the loss of the limb, which adversely impact health-related quality of life (HRQoL)[3]. Functional reconstruction can be achieved through upper limb prosthesis; however, their accessibility may be precluded by high upfront and running costs, even in a developed nation such as the UK. These costs are difficult to determine due to a wide range of available devices and the extent of prosthesis required, which in turn is dependent on the level of amputation[4]. In the United States, one source has estimated the mean cost of a myoelectric prosthesis for partial hand amputations at $18,703, $20,329 for transradial amputations, $59,664 for Transhumeral amputations, and approximately $62,000 for shoulder and forequarter amputations[5]. Overall, prosthesis-related expenses can range between £31,890 to $117,440, clearly highlighting a significant financial burden on both the patients and the healthcare system[4].
The nerve-related pain experienced after upper limb amputation can be both persistent and debilitating[6]. The two main nociceptive sensations after amputation are neuroma pain (NP) and phantom limb pain (PLP), which can be differentiated based on their character, location and triggers[7]. NP is typically initiated by direct pressure over the end of the injured nerve, while PLP is any pain or discomfort that is perceived to occur in the now absent limb[8]. The sustained and persistent nature of these two types of pain has been demonstrated to adversely impact the patient’s HRQoL[9]. Although the introduction of neuropathic agents (e.g., gabapentin) has had a transformational effect on the management of both of these types of pain, these drugs cannot abolish pain and patients often suffer from a variety of debilitating side effects or may be completely intolerant of the medication[10]. Chronic use of the medication is also costly for many healthcare systems.
Targeted muscle reinnervation (TMR) has shown great promise in the treatment of both types of nerve-related pain[11]. By providing a muscle target to the regenerating nerve stumps after amputation, TMR surgery appears to reduce the reformation of painful neuromas while simultaneously providing feedback to the central nervous system (CNS), which appears to reduce the perception of PLP. However, to date, there has been no work to quantify the impact of TMR surgery on the quality of life in this population.
METHODS
We performed a retrospective review of all upper limb amputees with NP and/or PLP who underwent TMR surgery between October 2013 and September 2021 by the Relimb Unit, Royal Free Hospital, London, United Kingdom. Data were collected from patient records and telephone interviews. Additional baseline characteristics were also collected from the study participants, including; age, gender, date of procedure and indication for TMR. Our primary outcome measures evaluated pain and quality of life. Subjects were contacted and asked to complete the surveys at two time points: pre-operatively, and at the time of interview. For pain measures, we used the 11-point numerical (Pain) rating scale (NRS), where 0 indicates “no pain” and 10 indicates “the worst possible pain”. Pain levels were identified separately as either NP and PLP, pre-operatively and at the time of the interview. As previously indicated, NP was defined as pain occurring within the stump – located over the ends of the nerve stumps, and PLP was defined as painful sensations perceived in the absent limb.
Quality of life was evaluated using the EuroQol EQ5D-5L questionnaire (with permission from EuroQol). The seven metrics provided by the EQ-5D questionnaire were evaluated (five domains, an index score, and a Visual Analogue Scale/VAS score).
Surgical technique
The surgical techniques used by the Relimb unit are based on Kuiken and Dumanian’s description of TMR surgery[12] and these have been described previously[13].
Statistical analysis
A statistical analysis was performed with IBM SPSS Statistics (IBM Corporation, Armonk, New York, USA). The NRS data were evaluated using the Wilcoxon Signed Rank Test, identifying any changes pre and post-surgical intervention. The EQ-5D VAS data were analysed using a paired sample t-test, evaluating HRQoL pre and post-surgical intervention.
RESULTS
A total of 15 patients completed the evaluation. The mean age of the study participants was 55.8 years, and five of the 15 participants were female (33%). All patients underwent TMR surgery between October 2013 and September 2021. The indication for TMR in these patients was for secondary treatment of NP or residual limb pain (RLP) and/or PLP, sequelae of upper limb amputation. As such, TMR surgery was offered to our patients several years after their initial amputation surgery.
The data show a statistically significant reduction in both PLP (pre-operative mean: 7.6, post-operative mean: 2.7, P < 0.05) and NP (pre-operative mean: 6.4, post-operative mean: 2.5, P < 0.05) [Figure 1].
Figure 1. Demonstrates the changes in NP and PLP both prior to and after TMR intervention. NP demonstrated a reduction from 6.4 to 2.5 and PLP from 7.6 to 2.7 after TMR. TMR: Targeted muscle reinnervation; PLP: phantom limb pain; NP: neuroma pain.
Table 1 demonstrates the changes in score across each of the EQ-5D domains. The green colour denotes an improvement in a domain and red denotes a reduction in domain function. A total of 12 patients experienced a change in their EQ-5D domains. Nine patients noted improvements and five patients noted reductions in functionality.
Demonstrating the change in pre- and post-operative EQ-5D
| Change in EQ-5D | ||||||
| Patient number | Mobility | Self-care | Usual activities | Pain | Anxiety | VAS |
| 1 | 0 | -1 | -1 | -2 | -1 | 15 |
| 2 | 0 | 0 | 1 | 0 | 0 | 0 |
| 3 | n/a | n/a | n/a | n/a | n/a | n/a |
| 4 | n/a | n/a | n/a | n/a | n/a | n/a |
| 5 | 0 | 0 | 0 | -2 | 0 | 15 |
| 6 | 0 | -1 | -1 | -3 | 0 | 20 |
| 7 | 1 | 0 | -2 | -1 | 0 | 5 |
| 8 | 0 | 0 | 0 | 0 | 0 | 0 |
| 9 | 0 | 0 | 0 | -1 | 1 | 50 |
| 10 | 0 | 0 | 1 | -1 | 0 | 10 |
| 11 | 0 | 0 | 0 | 0 | 0 | 0 |
| 12 | -2 | -2 | -1 | -2 | -2 | 55 |
| 13 | n/a | n/a | n/a | n/a | n/a | n/a |
| 14 | 1 | 0 | 0 | 1 | 0 | 0 |
| 15 | 0 | 0 | 0 | -3 | 0 | 0 |
| 16 | 0 | 0 | 0 | 0 | 0 | 0 |
| 17 | n/a | n/a | n/a | n/a | n/a | n/a |
| 18 | n/a | n/a | n/a | n/a | n/a | n/a |
| 19 | 0 | 0 | 0 | -1 | -2 | 30 |
| 20 | 0 | 0 | 0 | -2 | -2 | 35 |
Ten of the 11 patients reporting changes in pain as part of their EQ-5D found an improvement in this domain. Changes in HRQoL were observed for the EQ-VAS scale, and these demonstrate an improvement in quality of life from 68 pre-operatively to 78 post-procedure (P < 0.05).
DISCUSSION
In many instances since 2008, the evaluation of the quality of life has been based on the EQ-5D, Euroqol questionnaires[14]. Ernstsson and colleagues evaluated the use of EQ-5D questionnaire to assess HRQoL following lower limb amputation surgery. They highlight the correlation between factors such as pain due to NP/RLP or PLP, reduced mobility and impaired activities of daily living with poor HRQoL. The authors conclude that the EQ-5D-5L questionnaire has high validity and feasibility to assess HRQoL, particularly in lower limb amputees[15]. Globally, access to healthcare can be challenging due to limited resources, healthcare provider expertise and funding. A recent study identified an average cost of $28,961 to the patient for upper extremity amputation. Equally, the healthcare system saw an overall cost of $166 million over a 15-year period[16]. Lifetime costs to an amputee patient can exceed $500,000[4]. The EQ-5D-5L questionnaire is a reproducible and informative resource that provides practical insight into the impact on a patient’s quality of life. The international impact of the EQ-5D and its applicability is a testament to its wide-ranging benefits and further supports policy makers at national and firm levels in their decision making to fund the interventions.
Previous articles have already established the reproducible nature of TMR in improving symptoms of NP and PLP after amputation. However, there has been no work specifically evaluating the interplay between the chronic pain caused by NP and PLP on quality of life after upper limb amputation. Moreover, while recognised by NICE as a key metric[17], assessing changes in (pain) quality of life is not routinely performed after upper limb amputation. Our study highlights the efficacy of TMR in improving HRQoL, with 66% of patients reporting an overall improvement following their intervention. It is important to assess why five (33.3%) patients reported a decrease in functionality for some domains such as pain, mobility and usual activities following TMR. We hypothesise that this could be multifactorial. Some reasons may include individual patient perception towards domains such as pain and anxiety, extent of the initial injury, degree of amputation and site of injury. Other reasons include non-specific questions such as mobility, which some patients may have perceived as pertaining to lower limb mobility rather than upper limb, and further could be a function of other confounding variables as it may sometimes be challenging to discern the changes patients experience from surgery versus over time. In addition, the retrospective nature of our study gives rise to the potential impact of recall bias. Patients may not recall the impact that TMR may have had on their HRQoL, particularly if a number of years have elapsed since their surgery. Our study was conducted in December 2021 on patients who initially had their TMR operation as far back as October 2013. Amongst the five patients with a reduction in domain function, three (60%) demonstrated positive improvements in other domains [Table 1]. Therefore, despite these drawbacks, most patients in our study reported an overall improvement in their HRQoL following TMR, as evidenced by their Q-5D-5L domain scores and VAS. Our study provides precedence for further investigation into the HRQoL benefits associated with TMR surgery for secondary NP/RLP and/or PLP associated with upper limb amputation. Ideally, this should be performed in the context of a multi-centre randomised control trial.
For this analysis, we used a numerical (pain) rating scale (NRS) which was simple, reproducible, and easily understood (by patients and researchers) to perform surveys over the telephone. This was necessary because of the restrictions on face-to-face contact during the COVID-19 pandemic. However, we accept that further work could be done to evaluate the complexity of the questionnaires we administered, their reproducibility and error rate to create a better framework for future trials.
Funding for TMR surgery in the UK is currently determined on a local level. Since there are no OPCS codes for this procedure, the codes for a number of different procedures (e.g., nerve repair, nerve transfers, free tissue transfer) are often put together to cover the cost of the TMR procedures. However, the absence of any uniformity of what constitutes a TMR procedure may contribute to further inequities in healthcare provision in the future. As a first step towards reducing these inequities, we have tried to quantify the size of the improvements in quality of life produced by TMR surgery after upper limb amputation. Based on our analysis, we believe that there is sufficient evidence to inform any future Health Technology Assessments and Appraisal, and this may enable NICE to make recommendations on the future (national) provision for TMR surgery. However, the complex nature of the surgery (especially in the upper limb) means that it is likely to need that such care will only ever be possible on a tertiary or quaternary basis.
Limitations
The main limitation of this study is its retrospective nature. Our methodology draws on the (validated) retrospective use of the EQ-5D questionnaire in an orthopaedic population[18]. Our small sample size and the lack of a control group could be enhanced with future work, although it is important to note that the novelty of the intervention precluded greater patient recruitment.
Conclusions
In this study, TMR appears to have improved the quality of the lives of a small cohort of upper limb amputees with NP and PLP. This improvement was evident across many metrics, and more broadly in quality-of-life assessments. The implications of these findings require further analysis, including randomized control trials to potentially inform policy and national commissioning to ensure equitable access to this type of surgery for patients who have experienced limb loss.
DECLARATIONS
AcknowledgmentsWe would like to acknowledge Tamar Makin for her help with the study.
Authors’ contributionsMade substantial contributions to the conception and design of the study and performed data analysis and interpretation: Zargaran D, Nagra R, Zargaran A, Akella M, Ajam Y, Woollard A, Kang N
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateAll patients agreed to participate in this study.
Consent for publicationInformed consent of the patient has been obtained.
Copyright© The Author(s) 2023.
REFERENCES
1. Specialised Commissioning Team NE. Hand and upper limb reconstruction using vascularised composite allotransplantation (HAUL-VCA). Available from: https://www.england.nhs.uk/wp-content/uploads/2018/07/Hand-and-upper-limb-reconstruction-using-vascularised-composite-allotransplantation.pdf [Last accessed on 16 Mar 2023].
2. Roșca AC, Baciu CC, Burtăverde V, Mateizer A. Psychological consequences in patients with amputation of a limb. An interpretative-phenomenological analysis. Front Psychol 2021;12:537493.
3. Resnik L, Borgia M, Clark M. Function and quality of life of unilateral major upper limb amputees: effect of prosthesis use and type. Arch Phys Med Rehabil 2020;101:1396-406.
4. Efanov JI, Tchiloemba B, Izadpanah A, Harris PG, Danino MA. A review of utilities and costs of treating upper extremity amputations with vascularized composite allotransplantation versus myoelectric prostheses in Canada. JPRAS Open 2022;32:150-60.
5. Blough DK, Hubbard S, McFarland Lv, Smith DG, Gambel JM, Reiber GE. Prosthetic cost projections for servicemembers with major limb loss from vietnam and OIF/OEF. J Rehabil Res Dev 2010;47:387-402.
6. Wartan SW, Hamann W, Wedley JR, Mccoll I. Phantom pain and sensation among British veteran amputees. Br J Anaesth 1997;652:121-9.
7. Hsu E, Cohen SP. Postamputation pain: epidemiology, mechanisms, and treatment. J Pain Res 2013;6:121-36.
8. Collins KL, Russell HG, Schumacher PJ, et al. A review of current theories and treatments for phantom limb pain. J Clin Invest 2018;2168:121-76.
9. Kim M, Kim Y, Ryu GW, Choi M. Functional status and health-related quality of life in patients with peripheral artery disease: a cross-sectional study. Int J Environ Res Public Health 2021;18:10941.
11. Dumanian GA, Potter BK, Mioton LM, et al. Targeted muscle reinnervation treats neuroma and phantom pain in major limb amputees: a randomized clinical trial. Ann Surg 2019;270:238-46.
12. Souza JM, Cheesborough JE, Ko JH, Cho MS, Kuiken TA, Dumanian GA. Targeted muscle reinnervation: a novel approach to postamputation neuroma pain. Clin Orthop Relat Res 2014;472:2984-90.
13. Kang NV, Woollard A, Michno DA, Al-Ajam Y, Tan J, Hansen E. A consecutive series of targeted muscle reinnervation (TMR) cases for relief of neuroma and phantom limb pain: UK perspective. J Plast Reconstr Aesthet Surg 2022;75:960-9.
14. NICE. Position statement on use of the EQ-5D-5L value set for England (updated October 2019). Available from: https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/technology-appraisal-guidance/eq-5d-5l [Last accessed on 16 Mar 2023].
15. Ernstsson O, Hagberg K, Janssen MF, Bonsel GJ, Korkmaz S, Zethraeus N, et al. Health-related quality of life in patients with lower limb amputation-an assessment of the measurement properties of EQ-5D-3L and EQ-5D-5L using data from the Swedish Amputation and Prosthetics Registry. Disabil Rehabil 2022;44:8471-9.
16. Vakhshori V, Bouz GJ, Mayfield CK, Alluri RK, Stevanovic M, Ghiassi A. Trends in pediatric traumatic upper extremity amputations. Hand 2019;14:782-90.
17. Bullinger M, Quitmann J. Quality of life as patient-reported outcomes: principles of assessment. Dialogues Clin Neurosci 2014;16:137-45.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Zargaran D, Nagra R, Zargaran A, Akella M, Ajam Y, Woollard A, Kang N. An analysis of the role of targeted muscle reinnervation (TMR) in quality of life and pain outcomes: a case series. Plast Aesthet Res 2023;10:10. http://dx.doi.org/10.20517/2347-9264.2022.42
AMA Style
Zargaran D, Nagra R, Zargaran A, Akella M, Ajam Y, Woollard A, Kang N. An analysis of the role of targeted muscle reinnervation (TMR) in quality of life and pain outcomes: a case series. Plastic and Aesthetic Research. 2023; 10: 10. http://dx.doi.org/10.20517/2347-9264.2022.42
Chicago/Turabian Style
Zargaran, David, Raveenjot Nagra, Alexander Zargaran, Medha Akella, Yazan Ajam, Alex Woollard, Norbert Kang. 2023. "An analysis of the role of targeted muscle reinnervation (TMR) in quality of life and pain outcomes: a case series" Plastic and Aesthetic Research. 10: 10. http://dx.doi.org/10.20517/2347-9264.2022.42
ACS Style
Zargaran, D.; Nagra R.; Zargaran A.; Akella M.; Ajam Y.; Woollard A.; Kang N. An analysis of the role of targeted muscle reinnervation (TMR) in quality of life and pain outcomes: a case series. Plast. Aesthet. Res. 2023, 10, 10. http://dx.doi.org/10.20517/2347-9264.2022.42
About This Article
Special Issue
Copyright
Data & Comments
Data

 Cite This Article 3 clicks
Cite This Article 3 clicks










Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.