Management of soft tissue defects of the thumb
Abstract
Hand surgery has undergone substantial changes in recent years, especially for reconstructive surgery techniques. We discuss the management of soft tissue defects of the thumb, discussing indications, and operative pearls and pitfalls. We cover non-operative treatment and local advancement flaps for small distal soft tissue defects and pedicled flaps for more significant defects. We also discuss composite vascularized free flaps such as second-toe neurocutaneous flaps and partial hallux transfer for compound defects or total amputations. This article aims to provide hand surgeons with an update on reconstructing an injured thumb.
Keywords
INTRODUCTION
The thumb is the most important digit; its loss causes up to 40% of hand impairment[1]. There are many things that a surgeon should know about the beauty of this crucial digit. However, as this article is surgical, the discussion will be oriented to the operative reconstruction of the thumb. We divided the subject into terminal defects and intercalated defects. The aim is to give the reader an idea of how to approach an injured thumb.
The objective in reconstruction is a normal thumb, and we should stress that nothing is like the original. No reconstructive procedure can be compared to a successful replantation; therefore, it is mandatory to attempt replantation in every amputation[2]. The goals for reconstruction are (first and foremost) a pain-free thumb simply because a painful one will not be used. Similarly, length is critical-a short thumb will be relatively unable to grab large objects or pinch and pick up smaller ones.
Before managing any thumb injury, it is worth stressing the importance of not introducing scars that might hinder the definitive reconstruction. If the surgeon is unsure of the appropriate procedure, the wisest thing is to clean the wound, debride devitalized tissues, and send the patient to a specialized center. One should avoid attempting primary closure if doing so entails sacrificing essential tissue, particularly functioning joints. If this is not feasible, a suitable alternative is to cover the stump with a groin or other flap[3,4]; doing so prevents the sacrifice of structures that might be crucial for later reconstruction and will allow time for proper planning.
TERMINAL DEFECTS
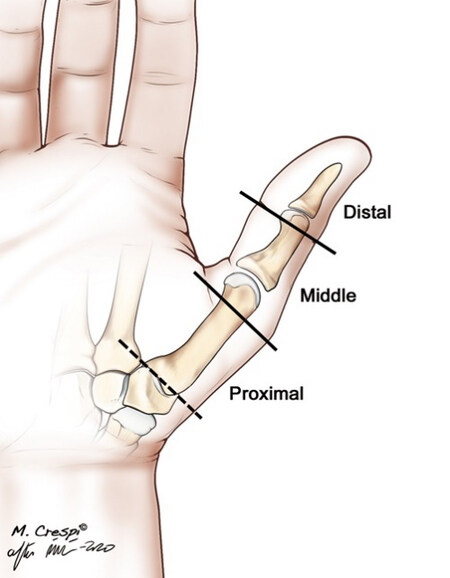
We adhere to the classification system of Dr. Strickland set out in the first edition of Green’s[5] [Figure 1]. It is most beneficial to define the precise anatomical location of the amputation. Length is essential; however, one should also consider thenar muscle damage, skin quality, nerve avulsion, and the functionality of the joints proximal to the amputation.
Figure 1. Areas of thumb loss considered (© Dr. Piñal 2020)[6].
There is no one-size-fits-all method for treating distal defects. The choice depends on the obliquity, the nail defect, and the amount of missing bone. Of these, the nail defect should have the most impact on decision-making. Amputations proximal to the eponychial fold are more conducive to a hallux transfer.
Soft tissue defects
In the most common type of distal amputation, a part of the sterile matrix is preserved. In these cases, efforts to preserve length and to provide sensitive, non-painful cover are the goal. Immediate wound coverage is the highest priority to prevent further tissue desiccation and length loss. In recent years, we witnessed considerable advances in flap design, owing to a better understanding of the blood supply to the thumb[7-9]. This has entailed that cross-finger flaps and many distant flaps are currently either reserved for extreme situations, or plainly discarded, and thus will not be discussed.
Smaller than 50% of the pulp surface
Semi-occlusive dressing
Healing by secondary intention by application of semi-occlusive dressing, as described by Mennen and Weiss, is a simple and inexpensive method for small defects without fracture or tendon exposure; it provides a consistent pulp with excellent contouring and a satisfactory return of sensation[10-13].
The stump is covered with a semi-occlusive transparent adhesive dressing after cleaning and debridement, which is changed weekly. The patient is allowed to use the thumb freely. The patient should be informed that a foul odor is normal and advised of the importance of keeping the dressing in place while healing occurs.
Volar advancement flap
Small soft tissue defects that require less than 5 mm of advancement can be covered readily by local advancement with palmar V-Y plasty, bilateral V-Y plasty, or modifications thereof[14-16]. The choice is based on the preference and experience of the surgeon, as all flaps are equally effective.
Moberg volar advancement flap
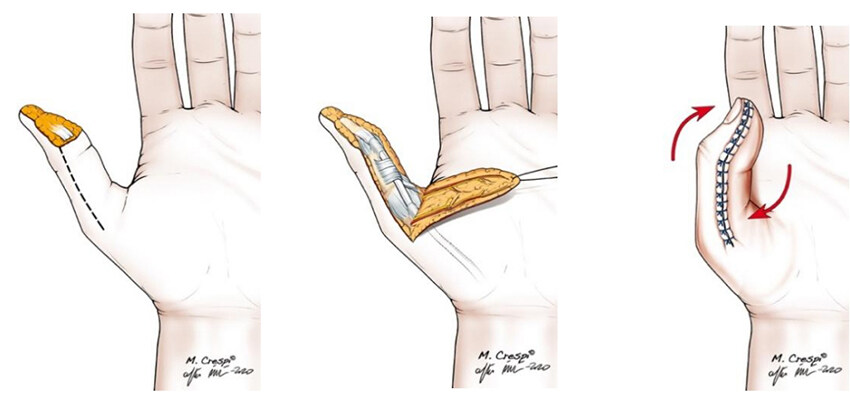
Moberg described a flap based on proper neurovascular bundles for coverage of palmar defects of the pulp[17] [Figure 2]. The flap permits covering moderate-size defects and provides sensitive skin simultaneously. If good coverage of the pulp requires more than 45º of interphalangeal (IP)-joint flexion, transforming the flap into a true island[18] or combining the advancement with a V-Y flap[19],or Z-plasty can provide some extra length[20].
Figure 2. The flap is raised through two midaxial incisions. Both neurovascular bundles are included in the flap. Some flexion contracture is permitted temporarily for closure (© Dr. Piñal 2020)[6].
Defects up to 2 cm (about half the pulp length) can be covered with this flap; however, this benefit comes at the price of causing a flexion contracture of the IP joint that can result in a painful thumb and a beaked nail deformity. Problems ensue when asking too much of the flap [Figure 3].
Figure 3. A: Excessive demands on the volar advancement flap cause painful flexion contracture of the IP joint. B: By lifting the flap, resecting the fibrotic tendon sheath, and releasing the volar plate, the true defect spanning the whole pulp was revealed. C: The defect was treated with a hemipulp flap (© Dr. Piñal 2020) larger than 50% of the pulp surface.
Larger than 50% of the pulp surface
Dorso-ulnar homodigital flap (Brunelli)
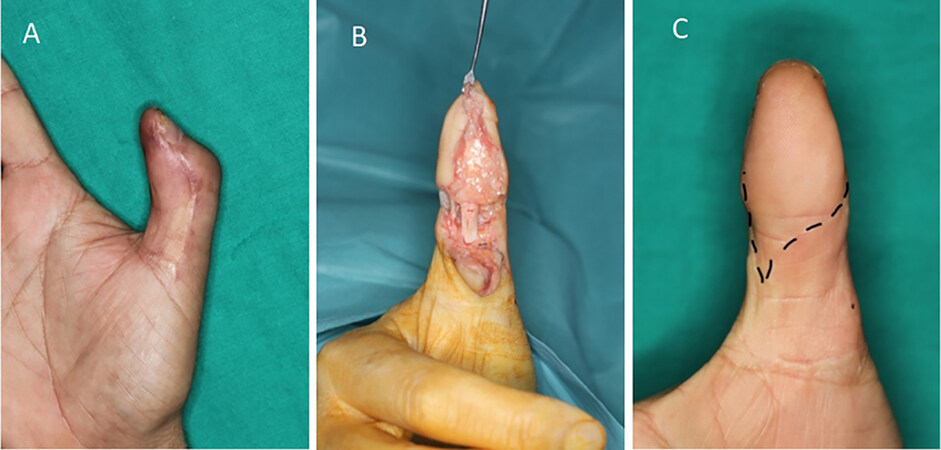
Brunelli et al. studied the arteries’ layout on the thumb’s dorsal surface[7,21]. The constant disposition and anastomoses permitted raising a distally-based flap safely from the dorso-ulnar region of the metacarpophalangeal joint[22,23].
This flap is based on the ulnar dorsal digital artery of the thumb, which (like its radial counterpart) has a peculiar anatomy [Figure 4]. During its short course, it has two constant anastomoses that allow this flap to rotate in two locations. The first pivot point is located at the neck of the proximal phalanx (2.5 cm proximal to the cuticle), reaching dorsal thumb defects; the second is located at the level of the nail fold arcade (0.9 to 1 cm proximal to the cuticle), providing the possibility to cover the nail and the pulp.
Figure 4. Arterial disposition of the dorsal arteries of the thumb. Note that the radial dorsal digital artery only reaches the nail fold arcade in 20% of the cases, while on the ulnar side, this connection is constant (© Dr. Piñal 2020)[6].
Several essential details should be considered. First, the flap may only be used if the area of cross anastomosis is intact. Second, venous congestion might occur if the skin over the pedicle is closed or tunneling is performed; therefore, skin grafting is recommended. Third, a first-web contracture might occur if the donor site is closed overly tight; therefore, skin grafting is recommended if large flaps are raised[24,25].
This flap does not provide sensitive skin, even when the dorsal branch of the radial nerve is connected to the ulnar digital nerve. For this reason, we only recommend it for more than 50% pulp loss in older adults, where sensory recovery is frequently poor, irrespective of the reconstructive option selected, or in patients that do not want a more complex reconstruction.
Dorso-radial advancement flap (Moschella and Cordova)
Moschella and Cordova described a similar flap based on the radial dorsal digital artery to treat radial and dorsal thumb defects[21,26] [Figure 4].
The rotation point of this flap is always the middle of the proximal phalanx. This is so because it has a different arterial communicating pattern than the ulnar counterpart, with a distal arcade only being present in about 20%. The flap can be quite large (up to 3 cm × 4 cm) while still achieving primary closure, as there is no risk of web contracture[26,27]. The flap is a rapid and safe solution for many lateral and dorsal defects of the thumb.
First dorsal metacarpal island flap (Kite flap/Foucher flap)
One of the most popular procedures for thumb defects is the first dorsal metacarpal artery flap, also known as the “kite flap”, initially described by Foucher and Braun in 1978[28] [Figure 5]. The flap was devised for dorsal defects and as a vein carrier for thumb replantation. However, the fact that it can include a sensory branch from the radial nerve has made it usable for covering palmar defects, particularly in older adults[29].
Figure 5. Technique for raising a kite flap from the dorsum of the proximal phalanx of the index and transferring to the dorsum of the thumb. The vascular pedicle comprises the first dorsal metacarpal artery (with the perivascular fat and adjacent part of the aponeurosis), one or two superficial veins, and the radial nerve branches. (Modified from Littler)[28] (© Dr Piñal 2020)[6].
The arterial supply of the flap is based on the dorsal radial artery of the index. This branch originates from the first dorsal metacarpal artery, which takes off from the radial artery between the crossing of the extensor pollicis longus and its penetration into the apex of the first interosseus space. The dorsal radial artery of the index is constant[28].
We prefer to assess the vascularity of the flap only after it has been sutured onto its final position. Doing otherwise will not prevent later necrosis due to pedicle kinking by a fascial band or constriction in the tunnel.
The flap is particularly indicated for dorsal thumb defects. We do not consider this flap applicable for pulp defects, except in older adults[29]. The donor site can be a source of hypertrophic scarring and painful ulcerations. To prevent this, the flap should not trespass the metacarpophalangeal or proximal interphalangeal joint creases, and the peritenon should be left intact. Furthermore, the kite flap plays an indisputable starring role for dorsal thumb defects combined with venous outflow difficulties[30] [Figure 6].
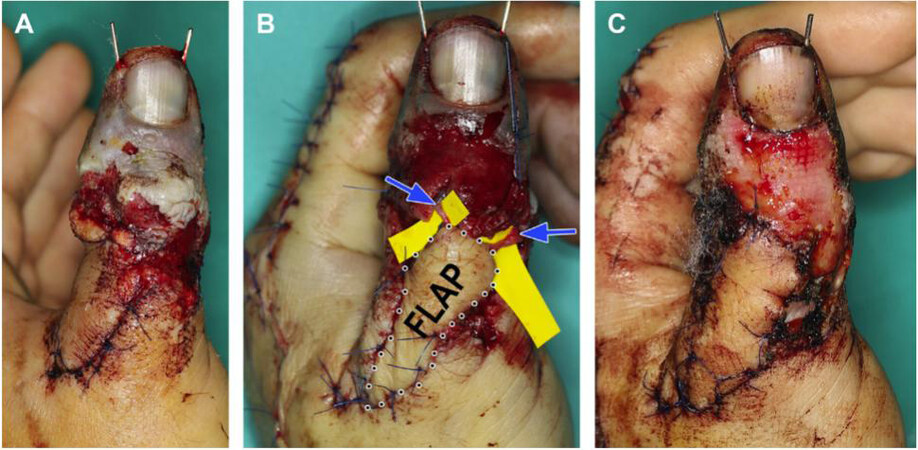
Figure 6. A: This patient was referred 48 hours after replantation for impending venous failure. B: A 1.0 cm × 2.5 cm first dorsal metacarpal flap was elevated from the dorsum of the index permitting primary closure of the donor site. The flap eased the circular soft tissue constriction of the thumb and (most importantly) carried two veins restoring the outflow of the thumb (blue arrows). C: Complete survival at two weeks (© Dr. Piñal 2016)[30].
Heterodigital island flap (Littler flap)
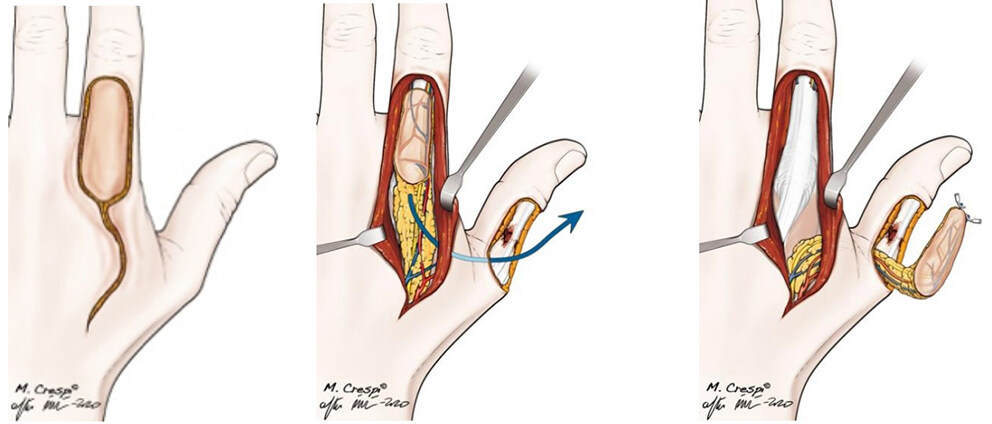
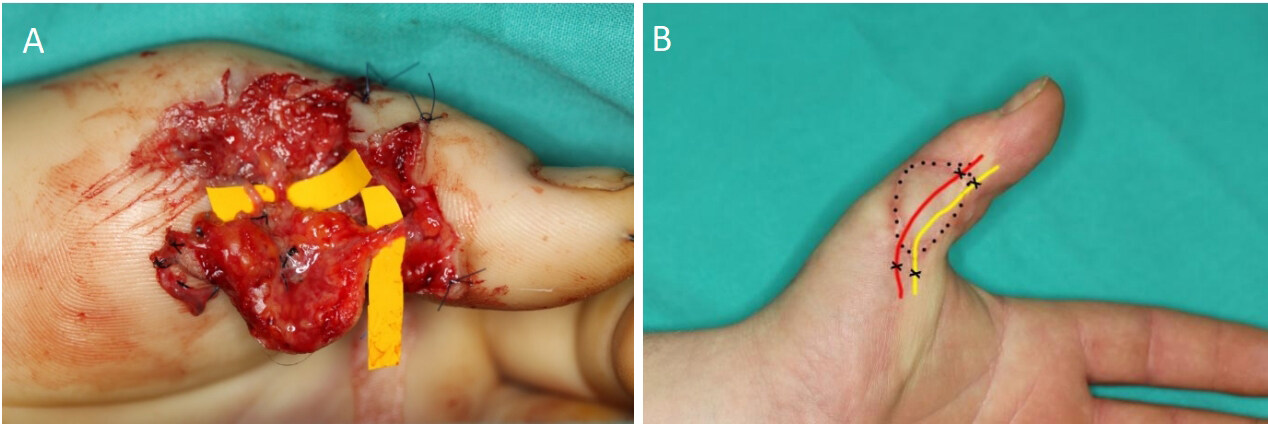
The Littler flap[31] is taken from the ulnar aspect of the middle finger and tunneled to the pulp of the thumb, based on its neurovascular bundle, providing sensation to the pulp [Figure 7].
Figure 7. A: An extended island flap is designed on the ulnar side of the long finger with an identical defect pattern over the palmar aspect of the thumb. B: Mobilization of the island flap on its neurovascular pedicle and preparation of the recipient bed on the thumb. C: Completed transfer of the neurovascular island flap with a full-thickness skin graft on the donor area of the long finger. Care must be taken to avoid a longitudinal scar along the palmar aspect of the donor finger. Note the area of undermining in the palm (© Dr. Piñal 2020)[6].
During the elevation of the flap, the utmost care should be taken to preserve the sheath of the flexors and the peritendineum of the extensor; otherwise, the bed may not be graftable. To safely pass the flap to the thumb, the tunnel should be large, and the graft should be pushed rather than pulled into the recipient side.
The flap is safe and effective in many respects but has problems and limitations. The most significant drawback derives from the fact that this is a sensitive flap with innervation for the middle finger, and hoping for cortical reorientation often ends in disappointment[32-35]. Therefore, if there are nerves available, to avoid cortical disorientation, it is preferable to connect the recipient thumb ulnar nerve and the nerve of the flap[32,33].
Flexion contracture of the middle finger is a common complication that occurs more frequently when a large flap has been raised, when the skin graft has not taken well or when proper aftercare is neglected. We prevent contracture by night-splinting the proximal interphalangeal joint in extension. Venous problems might occur in large flaps and in case of pedicle skeletonizing and can be prevented by including a dorsal vein and connecting it in the recipient site. For the standard-sized flap, this is not necessary. If the pedicle is insufficiently dissected, the flap will reach the thumb with difficulties, causing a painful band in the palm.
In summary, this flap is used in patients with considerable bone exposure and who do not wish for more complex reconstruction.
Nail defects
Not only is the nail an important cosmetic element, but it also allows us to pick up small objects and offers stability to the pulp when pinching. The problem of nail loss is compounded because it is often associated with bone loss. Hence, a length problem is added to the functional and cosmetic issues. The nail grows short and lacks adherence if the entire sterile matrix is lost. The patient may wish to have their nail removed completely to prevent this from happening.
An alternative is to transfer the sterile matrix and the bone from the hallux as a free onycho-osteo-cutaneous flap. Remarkably, the matrix of the toe will “meld” with the remaining thumbnail[36,37] [Figure 8]. Microvascular reconstruction appears to be the only method that procures consistent results[38-42].
Figure 8. A customized flap has treated the problem of a non-adhering nail. In the inset, the donor site (©Dr Piñal 2014)[36].
Total distal amputation
While a substantial number of papers concede that in amputations distal to the interphalangeal joint of the thumb, the loss of function is negligible[43,44], our experience is radically different. Patients whose thumb was amputated at the distal phalanx performed delicate tasks poorly and expressed a deep concern for the cosmetic outcome[36]. Furthermore, the locking effect of the thumb distal phalanx (the so-called “vice grip”, as termed by Buncke and Valauri)[45] is also lost. Several surgeons reported the salutary effect of reconstruction by a partial great toe transfer and the minimal morbidity on foot[36,37,46].
Partial hallux transfer
Partial toe is not beginner’s stuff. Apart from the need for familiarity with handling small vessels and anastomosis, in order to achieve a good cosmetic result, the dissection must go to the tip of the hallux to reduce the bone in the sagittal and coronal planes. The hallux is much larger than the thumb. I strongly recommend early transfer for distal amputation cases, not only for preserving exposed tissue but (above all) for smooth and straightforward surgery. Furthermore, early coverage of the stump-with the toe-preserves structures without needing temporary flaps.
There are some technical particularities worth emphasizing when dealing with mini-hallux flaps. The ipsilateral hallux is preferred as this permits the dominant artery and nerve to be oriented along the ulnar side of the thumb. Veins are dissected first, and this procedure is greatly facilitated if there is some blood in the veins; therefore, we elevate the tourniquet without emptying the limb using an Esmarch bandage.
Harvesting is facilitated by including the entire nail, as large dorsal veins proximal to the eponychial fold can be included. By contrast, partial nail harvesting obliges one to dissect the veins on the lateral aspect of the pulp, which are minute, fragile, and easily torn.
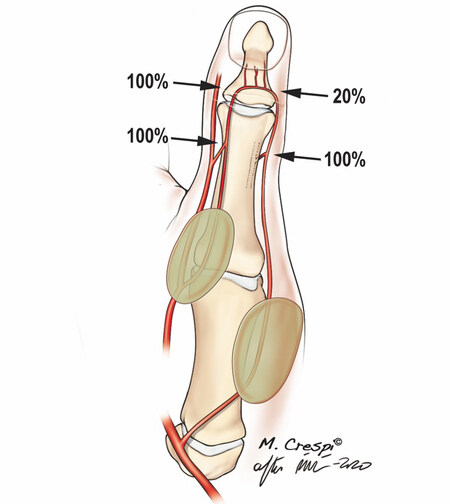
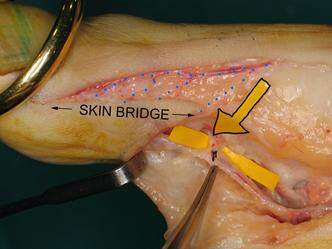
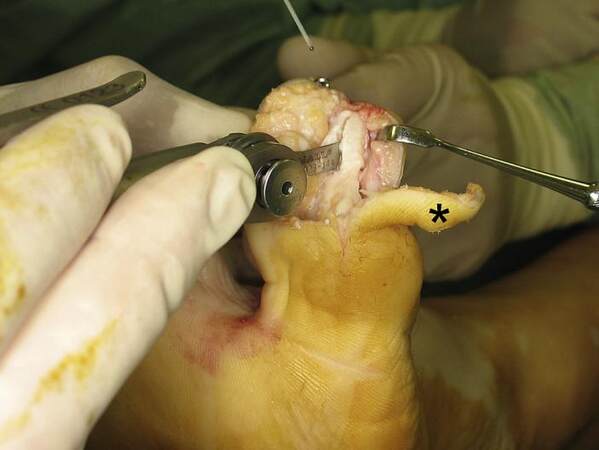
Regarding the arterial inflow, in most cases, I take only the peroneal digital artery. This maneuver accelerates harvesting at the price of a smaller vessel for the anastomosis. Most importantly, it minimizes donor site morbidity. We take utmost care in identifying, isolating, and ligating a constant branch immediately proximal to the neck of the first phalanx. Should this structure be avulsed, it could endanger the blood supply to the transfer [Figure 9].
Figure 9. A portion of the pulp must include a skin bridge to preserve the tiny and fragile veins in the skin that drain into the more prominent dorsal veins (blue dots). The yellow arrow points to the constant transverse digital artery (©Dr Piñal 2014)[36].
A segment of the lateral digital nerve is always included, and depending on the size of the toe pulp harvested, a part of the medial digital nerve can be included. After the dissection of the pulp of the phalanx, to reproduce the thumb shape, the bone should be trimmed in the sagittal and coronal planes [Figure 10].
Figure 10. Trimming of the medial side of the toe. Asterisk: medial-sided flap used as a V-Y advancement for closure (©Dr Piñal in 2014)[36].
Nerve(s) and vessels are passed through subcutaneous tunnels to avoid scarring. We usually revascularize a single artery and vein by end-to-end anastomoses with 10-0 nylon on a 100-µm needle.
The donor site is closed using a V-Y advancement flap from the medial side. If the whole nail has been elevated, we also place a skin graft on top of the periosteum to provide a nail-like appearance [Figure 11]
Figure 11. Placing a skin graft on the periosteum of the distal phalanx provides for a facsimile nail(©Dr Piñal 2014)[36].
Postoperatively, patients are perfused with heparin 500 U/h for two days, reduced to 250 U/h for another two days, and then switched to subcutaneous heparin for two weeks.
INTERCALATED DEFECTS
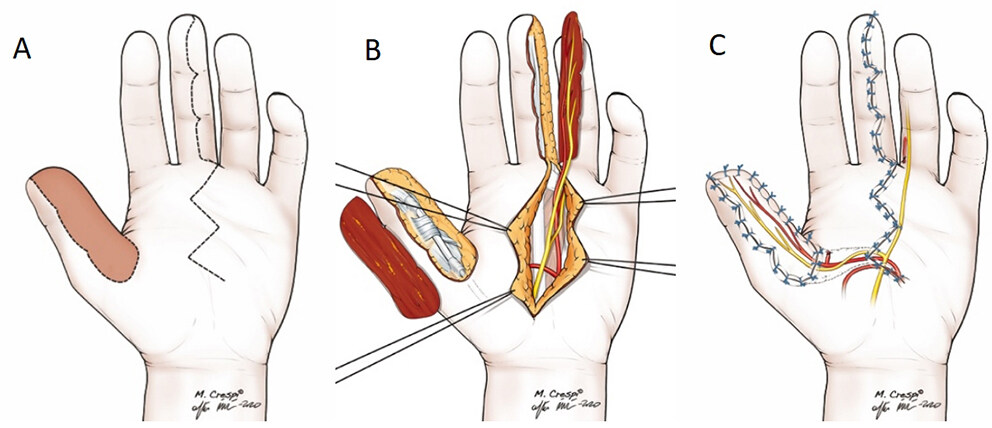
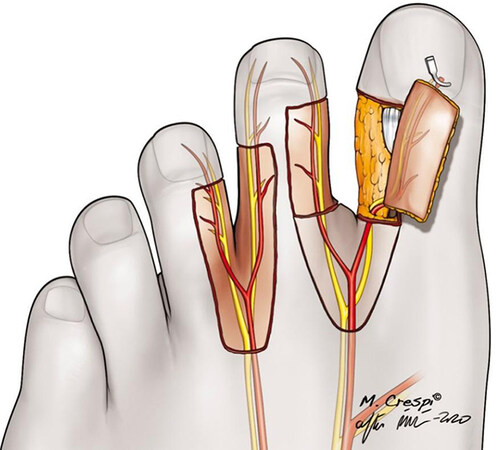
Traditionally, our attention has been focused on terminal defects of the thumb; however, intercalated injuries can cause as much damage as a complete loss. The reconstructive surgeon has tools to replace any intermediate portions lost. The foot is the primary donor site to replace like with like. Major nerve/vasculature/soft tissue and bone defects are usually managed by resorting to the second toe as the chief donor site[47-50] [Figure 12]. However, any area of the body that may fit into the defect and complete the jigsaw of any loss is most welcome.
Figure 12. Neurocutaneous flaps from the hallux or second toe can be planned to match complex digital defects (© Dr. Piñal 2020)[6].
Tibial second-toe vascularized neurocutaneous free flap
The surgeon may encounter an alive thumb that is poorly by dorsal arterial branches [Figure 13]. If untreated, the result is a painful atrophic thumb with a dystrophic nail, poor sensation, and cold intolerance. The results of flow-through versions of the toe neurocutaneous flap are unparalleled for these indications[51]. These flaps provide suitable cover, which is always necessary, excellent quality vessels to bypass small defects, and a vascularized nerve graft to provide sensibility [Figure 14]. Planning is essential to prevent dangerous crossover of vessels that may jeopardize arterial or venous flow. Rehearsals on paper are strongly recommended[48].
Figure 13. Compound defect includes the skin, vascular and nervous loss of the dorso-radial aspect of the thumb, including the radial digital nerve (© Dr. Piñal 2020)[6].
Figure 14. A: Tibial second-toe neurocutaneous free flap provided a one-stage reconstruction of soft tissue loss. B: Result at six months postoperatively (© Dr. Piñal 2020)[6].
Although the contents of the flap might require modification according to the patient’s specific needs, the elevation technique is comparable to that of other partial toe flaps, as we have covered above. Harvesting of the veins, which are very small and easily damaged, is typically the most critical part of the intervention. Therefore, we prefer dissecting them proximally in the dorsum of the foot and tracking them distally to the proximal edge of the flap, which is much faster and safer. Dissection of the arteries is much easier. The digital artery is dissected distally and followed proximally. Our preferred donor artery is the peroneal digital artery, which we dissect until the toe web. With the pedicle isolated, further elevation of the flap itself is relatively simple, following the periosteum medially and flexor sheath plane volarly with sharp dissection. The nerve can be included if necessary.
We rarely need to sacrifice the donor toe. In the soft tissue variant flaps, a full-thickness skin graft applied to the periosteum will do the job nicely. If a phalanx is harvested, we perform a resection arthroplasty or interphalangeal arthrodesis. When we use a large piece of bone, we perform syndactyly with the third toe.
CONCLUSION
The thumb is crucial to hand function. Whether the surgeon reconstructs the most distal tip injury or provides a complex reconstruction, the upgrade from the previous situation will be outstanding, and patient satisfaction will be high. We covered the current state of thumb coverage but intentionally did not broach the subject of more proximal amputations and devastating injuries, which are beyond the scope of this article. All hand surgeons should be confident in providing adequate soft tissue coverage of the thumb.
DECLARATIONS
Author’s contributionsThe investigation, writing the original draft, review, and editing: Van Hove B
Conceptualization, methodology, investigation, writing, reviewing, and editing: Del Piñal F
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateAll procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Consent for publicationInformed consent was obtained from the patients involved in the report, as was the consent for publication.
Copyright© The Author(s) 2023.
REFERENCES
2. Haas F, Hubmer M, Rappl T, Koch H, Parvizi I, Parvizi D. Long-term subjective and functional evaluation after thumb replantation with special attention to the Quick DASH questionnaire and a specially designed trauma score called modified Mayo score. J Trauma 2011;71:460-6.
3. Al-Qattan MM, Al-Qattan AM. Defining the indications of pedicled groin and abdominal flaps in hand reconstruction in the current microsurgery era. J Hand Surg Am 2016;41:917-27.
4. Wei FC. Tissue preservation in hand injury: the first step to toe-to-hand transplantation. Plast Reconstr Surg 1998;102:2497-501.
5. Strickland JW. Thumb reconstruction. In: Green DP (Ed) Green’s operative hand surgery, 1st Ed, New York: Churchill Livingstone; 1982. p. 1563-618.
6. del Piñal F. Thumb reconstruction. In: Green’s operative hand surgery, 8th edition; 2020. p. 1849-905.
7. Brunelli F, Gilbert A. Vascularization of the thumb. Anatomy and surgical applications. Hand Clin 2001;17:123-38.
8. Ames EL, Bissonnette M, Acland R, Lister G, Firrell J. Arterial anatomy of the thumb. J Hand Surg Br 1993;18:427-36.
9. Earley MJ. The arterial supply of the thumb, first web and index finger and its surgical application. J Hand Surg Br 1986;11:163-74.
11. Mühldorfer-Fodor M, Hohendorff B, Vorderwinkler KP, van Schoonhoven J, Prommersberger KJ. Treatment of fingertip defect injuries with a semiocclusive dressing according to Mennen and Wiese. Oper Orthop Traumatol 2013;25:104-14.
12. Mennen U, Wiese A. Fingertip injuries management with semi-occlusive dressing. J Hand Surg Br 1993;18:416-22.
13. Fox JW 4th, Golden GT, Rodeheaver G, Edgerton MT, Edlich RF. Nonoperative management of fingertip pulp amputation by occlusive dressings. Am J Surg 1977;133:255-6.
14. Atasoy E, Ioakimidis E, Kasdan ML, Kutz JE, Kleinert HE. Reconstruction of the amputated finger tip with a triangular volar flap. A new surgical procedure. J Bone Joint Surg Am 1970;52:921-6.
15. Bakhach J, Guimberteau JC, Panconi B. The Gigogne flap: an original technique for an optimal pulp reconstruction. J Hand Surg Eur Vol 2009;34:227-34.
17. Moberg E. Aspects of sensation in reconstructive surgery of the upper extremity. J. Bone Joint Surg Am 1964;46:817-25.
18. O'Brien B. Neurovascular island pedicle flaps for terminal amputations and digital scars. Br J Plast Surg 1968;21:258-61.
19. Elliot D, Wilson Y. V-Y advancement of the entire volar soft tissue of the thumb in distal reconstruction. J Hand Surg Br 1993;18:399-402.
21. Moschella F, Cordova A, Pirrello R, Brunelli F. Anatomic basis for the dorsal radial flap of the thumb: clinical applications. Surg Radiol Anat 1996;18:179-81.
23. Brunelli F, Vigasio A, Valenti P, Brunelli G. Arterial anatomy and clinical application of the dorsoulnar flap of the thumb. J Hand Surg Am 1999;24:803-11.
24. Terán P, Carnero S, Miranda R, Trillo E, Estefanía M. Refinements in dorsoulnar flap of the thumb: 15 cases. J Hand Surg Am 2010;35:1356-9.
25. Germann G, Sauerbier M, Rudolf KD, Hrabowski M. Management of thumb tip injuries. J Hand Surg Am 2015;40:614-22.
26. Moschella F, Cordova A. Reverse homodigital dorsal radial flap of the thumb. Plast Reconstr Surg 2006;117:920-6.
27. Hrabowski M, Kloeters O, Germann G. Reverse homodigital dorsoradial flap for thumb soft tissue reconstruction: surgical technique. J Hand Surg Am 2010;35:659-62.
28. Foucher G, Braun J. A new island flap transfer from the dorsum of the index to the thumb. Plast Reconstr Surg 1979;63:344-9.
29. Tränkle M, Sauerbier M, Heitmann C, Germann G. Restoration of thumb sensibility with the innervated first dorsal metacarpal artery island flap. J Hand Surg Am 2003;28:758-66.
30. Piñal F, Pennazzato D, Urrutia E. Primary thumb reconstruction in a mutilated hand. Hand Clinics 2016;32:519-31.
31. Littler JW. The neurovascular pedicle method of digital transposition for reconstruction of the thumb. Plast Reconstr Surg 1953;12:303-19.
32. Adani R, Squarzina PB, Castagnetti C, Laganá A, Pancaldi G, Caroli A. A comparative study of the heterodigital neurovascular island flap in thumb reconstruction, with and without nerve reconnection. J Hand Surg Br 1994;19:552-9.
33. Foucher G, Braun FM, Merle M, Michon J. La technique du “débranchement-rebranchement” du lambeau en îlot pédiculé. Ann Chir 1981;35:303-3.
34. Henderson HP, Reid DAC. Long term follow up of neurovascular island flaps. Hand 1980;os-12:113-22.
35. Murray JF, Ord JV, Gavelin GE. The neurovascular island pedicle flap. An assessment of late results in sixteen cases. J Bone Joint Surg Am 1967;49:1285-97.
36. Piñal F, Moraleda E, de Piero GH, Ruas JS, Galindo C. Onycho-osteo-cutaneous defects of the thumb reconstructed by partial hallux transfer. J Hand Surg Am 2014;39:29-36.
37. Woo S, Lee G, Kim K, Ha S, Kim J. Immediate partial great toe transfer for the reconstruction of composite defects of the distal thumb. Plast Reconstr Surg 2006;117:1906-15.
38. Wei F, Chen H, Chuang DC, Jeng S, Lin C. Aesthetic refinements in toe-to-hand transfer surgery. Plast Reconstr Surg 1996;98:485-90.
39. M1, Seki T, Yoshizu T, Saito H, Tajima T. Microsurgical toenail transfer to the hand. Plast Reconstr Surg 1991;88:102-110.
40. Foucher G, Braun FM, Smith DJ. Custom-made free vascularized compound toe transfer for traumatic dorsal loss of the thumb. Plast Reconstr Surg 1991;87:310-4.
41. Foucher G, Nagel D, Briand E. Microvascular great toenail transfer after conventional thumb reconstruction. Plast Reconstr Surg 1999;103:570-6.
42. Foucher G, Merle M, Maneaud M, Michon J. Microsurgical free partial toe transfer in hand reconstruction: a report of 12 cases. Plast Reconstr Surg 1980;65:616-26.
43. Azari K, Lee W. Thumb reconstruction. In: Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, editors. Green’s operative hand surgery. 6th ed. Philadelphia: Elsevier; 2011:1839-82.
46. Adani R, Cardon LJ, Castagnetti C, Pinelli M. Distal thumb reconstruction using a mini wrap-around flap from the great toe. J Hand Surg Br 1999;24:437-42.
47. del Piñal F. “Neurocutaneous toe free flap with pulp”, in ASSH Surgical Anatomy: Flap Reconstruction. Chicago, Ill: American Society for Surgery of the Hand;2018:313-320, S. Moran and K. Chung, Eds. Available from: https://drpinal.com/neurocutaneous-toe-free-flap-with-pulp/ [Last accessed on 3 Jan 2023].
48. del Piñal F. Partial toe transfer. In: The art of microsurgical hand reconstruction. Thiem: New York; 2013. p. 420-426.
49. Piñal F, García-bernal FJ, Regalado J, Studer A, Cagigal L, Ayala H. The tibial second toe vascularized neurocutaneous free flap for major digital nerve defects. J Hand Surg Am 2007;32:209-17.
50. Piñal F, García-bernal FJ, Delgado J, Sanmartín M, Regalado J, Cagigal L. Vascularized bone blocks from the toe phalanx to solve complex intercalated defects in the fingers. J Hand Surg Am 2006;31:1075-82.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Van Hove B, Del Piñal F. Management of soft tissue defects of the thumb. Plast Aesthet Res 2023;10:8. http://dx.doi.org/10.20517/2347-9264.2022.59
AMA Style
Van Hove B, Del Piñal F. Management of soft tissue defects of the thumb. Plastic and Aesthetic Research. 2023; 10: 8. http://dx.doi.org/10.20517/2347-9264.2022.59
Chicago/Turabian Style
Van Hove, Bram, Francisco Del Piñal. 2023. "Management of soft tissue defects of the thumb" Plastic and Aesthetic Research. 10: 8. http://dx.doi.org/10.20517/2347-9264.2022.59
ACS Style
Van Hove, B.; Del Piñal F. Management of soft tissue defects of the thumb. Plast. Aesthet. Res. 2023, 10, 8. http://dx.doi.org/10.20517/2347-9264.2022.59
About This Article
Special Issue
Copyright
Data & Comments
Data

 Cite This Article 8 clicks
Cite This Article 8 clicks














Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.