Vascularized lymph node transfer for the treatment of lymphedema: a systematic review and meta-analysis of clinical and patient-reported outcomes
Abstract
Aim: The aim of this systematic review was to summarize clinical and patient-reported outcomes (PROs) for various vascularized lymph node transfer (VLNT) donor sites and identify gaps in the literature to guide future research.
Methods: A literature search of five databases was performed for articles related to VLNT that were published prior to November 2021. Studies that included clinical outcomes or PROs from at least five adult patients who received VLNTs to treat lymphedema were included.
Results: Sixty-six studies met the study criteria. Most studies reported improved limb circumference/volume, reduction or discontinuation of conservative therapy, infection rate reduction, improved PROs, or postoperative imaging findings reflecting functional lymph nodes. There were significantly lower infection rates (P < 0.05) and a trend towards improved PROs in patients who received intra-abdominal flaps, but overall few studies reported these outcomes. There were no significant differences in complication rates at the donor or recipient site based on VLNT donor sites, or between intra-abdominal vs. extra-abdominal VLNT donor sites, although these outcomes are not uniformly reported.
Conclusion: This meta-analysis identified that intra-abdominal donor sites have the potential to reduce postoperative infectious episodes more than extra-abdominal donor sites. Though recent investigations address many understudied VLNT donor sites, larger comparative studies and a standardized methodology are needed to better characterize postoperative outcomes, which can offer more concrete evidence to guide surgical practice.
Keywords
INTRODUCTION
Lymphedema is a chronic condition characterized by the accumulation of protein-rich lymphatic fluid within the interstitium, leading to swelling of the affected limb and overlying skin and tissue changes[1]. Lymphedema can result in significant functional and psychological morbidity for patients, as it can be disfiguring, lead to infection, and limit the range of motion[2-5]. Regardless of disease severity, conservative treatment remains a cornerstone of management[6,7]. The main conservative treatments involve complete decongestive therapy (CDT), compression bandages, exercise, and meticulous skin care[7].
In some patients, surgical options may be of benefit. Amongst these options, lymphovenous anastomosis (LVA) and vascularized lymph node transfer (VLNT) have become increasingly popularized in recent years[6,7]. LVA involves the creation of a shunt between a high-pressure lymphatic system and a lower-pressure venule system, allowing for increased lymph drainage[8]. Vascularized lymph node transfer is theorized to operate through a different mechanism: the lymph nodes act like a “pump”, siphoning lymph from the surrounding tissues and draining through natural lymphovenous anastomoses within the flap[9,10].
Since its introduction, VLNTs have expanded to involve various novel donor sites[11]. Apart from the groin, where VLNT was initially described, supraclavicular, submental, lateral thoracic, omental, and jejunal mesenteric lymph node flaps have also been reported[11]. More research is needed to clarify the outcomes for upper and lower extremity lymphedema following the use of each of these donor sites. This systematic review thus presents the current evidence regarding clinical and patient-reported outcomes (PROs) based on these various VLNT donor sites and identifies gaps in the literature.
METHODS
A literature search was performed using a combination of keywords and controlled vocabulary in Embase.com 1947-, Ovid Medline 1946-, Scopus 1823-, The Cochrane Database of Systematic Reviews (CDSR), Cochrane Central Register of Controlled Trials (CENTRAL), and Clinicaltrials.gov 1997-. The search strategy encompassed variations of terminology, including synonyms and differences in spelling, and was agreed upon by the authors of this review. All search strategies were completed on November 12, 2021, with no added limits. Fully reproducible search strategies for each database can be found in the Appendix
The articles obtained from the search were uploaded to Covidence. Studies were included if they adhered to the following criteria: (1) included at least 5 patients aged 18 years or older; (2) addressed VLNT;
Three reviewers (Raman S, Sanka S, Ji J) independently screened investigations based on title/abstracts. Two research personnel reviewed each full-text article. A third reviewer was used in each instance where there was dissonance of opinion. Data from full-text articles were extracted and stored in Microsoft Excel
After full-text articles were identified, duplicate studies which included patients from the same institution from the same time period were removed to avoid confounding any meta-analysis. If multiple articles included the same group of patients and reported the same clinical outcome variables, the investigation reporting the most variety of clinical outcomes or greatest sample size was included in this systematic review.
Data extracted from each article included study-specific information (author, year of publication, country, study design, and inclusion/exclusion criteria of patients for the study); clinical outcomes (limb circumference or volume differences postoperatively, infection rate reduction, and reduction in need for conservative therapy); imaging outcomes; patient sample demographics [age, body mass index (BMI), gender, comorbidities, etiology of lymphedema, duration of lymphedema]; number of patients in each experimental arm; details of surgical intervention (procedure performed, donor and recipient site); staging criteria utilized; method in which clinical outcome variables were obtained including the location in the limb for circumference/volume measurements; clinical outcomes reported [limb circumference or volume difference, infection rate reduction (annual episodes of infection), and reductions in conservative treatment]; PROs for each investigation in which a validated questionnaire was utilized; complications related to donor or recipient site; and length of follow-up. An American Society of Plastic Surgeons Level of Evidence was assigned to each investigation[16]. PROs were recorded for each domain in which a value was reported.
Studies reporting infection rates were reviewed to identify those that presented this information in a standard fashion (episodes of infection/year preoperatively and postoperatively) to encourage comparability between studies. Due to significant variability in methodology and study design, outcomes related to improvement in limb size and reductions in conservative treatment were qualitatively summarized in table format. Patients were stratified based on donor and recipient site (upper or lower limb lymphedema) for meta-analysis of infection rate reduction and PROs. Continuous variables were summarized with mean and standard deviation. Categorical variables were summarized with frequencies or percentages.
Statistical analysis was performed using GraphPad Prism 9.2.0 (Dotmatics, Boston, MA, USA) with a statistical significance set to 0.05. Weighted means and fixed-effects pooled variances were tabulated for each variable, and these values were used to perform statistical analyses. To compare continuous variables, Kruskall-Wallis or Mann-Whitney tests were performed, as appropriate. Meta-analysis heterogeneity was calculated using the meta[17] and metafor packages[18] in R version 4.0.3[19] on the R Studio version 2022.02.3 platform. Missing variances were imputed using the prognostic method described by Ma et al., substituting mean variances for the missing values[20].
RESULTS
Summary of articles
Using the standardized search strategy, 1,301 studies with relevant titles and abstracts were retrieved from all databases. A total of 751 duplicate records were deleted after applying a deduplication process[21], and 550 citations were then imported into the project library. One further duplicate article was removed using Covidence.org. A total of 77 full-text investigations initially met the inclusion criteria for this study. Upon further review, 11 studies reporting the same outcomes from the same population were identified and removed. Ultimately, 66 studies were included in the systematic review. The selection process is described in a flowchart [Figure 1].
Figure 1. Flowchart depicting the screening process for inclusion of articles within our systematic review. Adhering to the inclusion/exclusion criteria of this study, 66 articles were included in the final review.
The ASPS level of evidence[16] for these articles ranged from Level II to Level IV [Table 1]. The majority of the studies (42 out of 66, 63.6%) were retrospective [Table 1].
Article characteristics
| Characteristic | Number of articles, n (%) |
| Retrospective | 42 (63.6) |
| Prospective | 24 (36.4) |
| Levels of evidence | |
| I | 0 (0) |
| II | 24 (36.4) |
| III | 41 (62.1) |
| IV | 1 (1.5) |
| V | 0 (0) |
| Staging scale | |
| ISL | 30 (45.5) |
| Cheng | 8 (12.1) |
| Taiwan | 1 (1.5) |
| MD anderson scale | 2 (3.0) |
| Campisi | 1 (1.5) |
| ICGN | 1 (1.5) |
| Unspecified | 2 (3.0) |
| None | 22 (33.3) |
Several staging scales were used to assess the severity of lymphedema. The most commonly used was the International Society of Lymphology scale (30 articles, 45.5%). A large subset (22 out of 66, 33.3%) did not use any imaging for staging [Table 1].
Out of all studies, 8 unique donor sites were identified: groin, submental, omentum, supraclavicular, lateral thoracic, appendicular, ileocecal, and jejunal mesenteric. Of note, twenty studies evaluated numerous VLNT donor sites in their investigation. Over half of all included studies (38 out of 66, 57.6%) addressed groin VLNT, followed by 20 (30.3%) which addressed omental, 14 (21.2%) submental, 13 (19.7%) supraclavicular, 9 (13.6%) lateral thoracic, and 2 (3.0%) each for appendicular and ileocecal, and 1 (1.5%) jejunal mesenteric. One article (1.5%) had a donor site from the neck region but was unclear about the specific flap utilized. The earliest investigations from our systematic review identify the groin VLNT as the initial donor site that propelled forward the era of VLNT. From 2010-2020, outcome-based research related to submental, supraclavicular, lateral thoracic, and jejunal mesenteric donor sites was published. The latest additions to VLNT within the past 5 years included additional intra-abdominal donor sites, such as appendicular and ileocecal.
Patient-reported outcomes using validated questionnaires were addressed in 16 (24.2%) of the investigations. These outcomes were most frequently from studies addressing groin, submental, and omental VLNT, while jejunal mesenteric, appendicular, and ileocecal VLNT had no articles addressing PROs for patients. Most studies (71.2%) reported on recipient-site complications, while 68.1% reported on donor complications.
Patient demographics
There were a total of 2316 patients and 2376 VLNTs reported in the 66 articles [Table 2]. It should be noted that not all investigations reported every patient demographic characteristic. Out of the studies reporting the gender of the patients, the majority of patients were female (63.9%). Overall, the mean age of patients was 54.0 ± 5.4 years and the mean BMI was 27.2 ± 2.5. Most of the patients (79.4%) had a secondary cause of lymphedema [Table 2]. Patients experienced symptoms for 51.1 ± 34.1 months prior to their surgery.
Patient demographics. Only data extractable from studies was reported
| Variable | Outcome |
| Total number of patients | 2316 |
| Total number of flaps | 2376 |
| Gender (n patients, % of total) | |
| Male | 175 (7.6) |
| Female | 1479 (63.9) |
| Unspecified | 662 (28.5) |
| Age (mean ± SD) | 54.0 ± 5.4 |
| BMI (mean ± SD) | 27.2 ± 2.5 |
| Etiology of lymphedema | |
| Primary | 145 (6.3) |
| Secondary | 1838 (79.4) |
| Unspecified | 333 (14.4) |
| Medical comorbidities | |
| Radiation | 636 (27.5) |
| Chemotherapy | 314 (13.6) |
| Diabetes | 31 (1.3) |
| HTN | 59 (2.5) |
| Smoking | 18 (0.8) |
| Duration of lymphedema (months) | 51.1 ± 34.1 |
| Donor site (n patients, % of total) | |
| Groin | 604 (26.1) |
| Submental | 304 (13.1) |
| Omentum | 467 (20.2) |
| Supraclavicular | 206 (8.9) |
| Lateral Thoracic | 62 (2.7) |
| Appendicular | 1 (0.04) |
| Ileocecal | 2 (0.09) |
| Jejunal mesenteric | N.S. |
| Unspecified † | 670 (28.9) |
| Extra- or intra-abdominal site | |
| Extra-abdominal site | 1606 (69.3) |
| Intra-abdominal site | 499 (21.5) |
| Unspecified † | 211 (9.1) |
| Recipient site (n patients, % of total) | |
| Upper extremity | 877 (37.9) |
| Lower extremity | 624 (26.9) |
| Upper and lower extremity* | 722 (31.2) |
| Unspecified | 93 (4.0) |
| Mean length of follow-up (months) | 24.1 ± 16.4 |
Large subsets of the overall sample received groin (26.1%) or omental (20.2%) flaps. Fewer received jejunal mesenteric, appendicular, and ileocecal VLNTs. More patients were treated for upper extremity lymphedema than lower extremity lymphedema. On average, patients followed up for 24.1 ± 16.4 months after surgery [Table 2].
Clinical outcomes
Overall, 47 out of 66 (71.2%) studies reported differences in limb circumference or volume postoperatively
Fourteen (21.2%) studies reported reduction or discontinuation of conservative therapy following the VLNT. In all studies assessing this outcome, a reduction or discontinuation of conservative therapy was observed postoperatively [Supplementary Table 3].
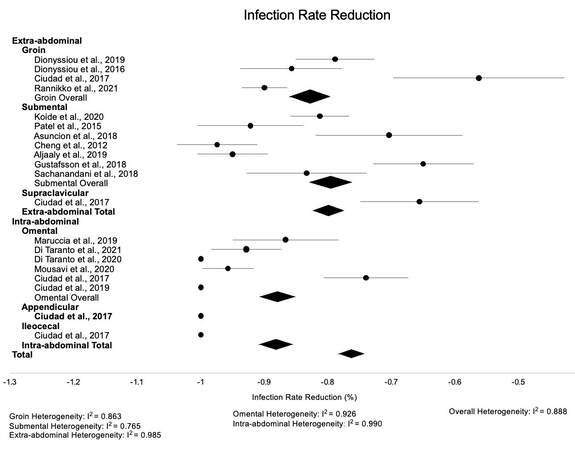
Twenty-four (36.4%) studies reported preoperative and postoperative episodes of cellulitis. The overall reduction of infection was 76.6% ± 1.4 % postoperatively [Table 3].
Infection rate reduction based on recipient and donor sites
| Anatomical site | Infection rate reduction (%) |
| Total | 76.6 ± 1.4 |
| Donor site | |
| Groin | 83.0 ± 3.2 |
| Submental | 79.5 ± 3.1 |
| Omentum | 87.9 ± 2.9 |
| Supraclavicular | 65.6 ± 9.5 |
| Lateral thoracic | N/A* |
| Appendicular | N/A* |
| Ileocecal | 100 ± 0 |
| Jejunal mesenteric | 100 ± 0 |
| Unspecified † | N/A# |
| Intra-abdominal donor site | 88.2 ± 2.8* |
| Extra-abdominal donor site | 79.9 ± 2.2* |
| Recipient site | |
| Upper extremity | 86.8 ± 1.6 |
| Lower extremity | 73.3 ± 2.5 |
Intra-abdominal flaps had a more significant reduction in postoperative infectious episodes than extra-abdominal flaps, 88.2% ± 2.8 % vs. 79.9% ± 2.2%, respectively (P = 0.009). There was no significant difference in infection rate reduction for patients who underwent VLNT for treatment of upper limb lymphedema and lower limb lymphedema, 86.8% ± 1.6% vs. 73.3% ± 2.5 %, respectively (P = 0.81). Additionally, differences in infection rate reduction between the different donor sites were not significant
Intra-abdominal vs. extra-abdominal
The donor sites were also grouped into intra-abdominal and extra-abdominal sites for further analysis. Omental, jejunal mesenteric, ileocecal, and appendicular flaps were recorded as intra-abdominal, while submental, groin, supraclavicular, lateral thoracic, and unspecified “neck” flaps were considered extra-abdominal. The majority of patients (69.3%) received an extra-abdominal VLNT, while 21.5% received an intra-abdominal flap [Table 2]. Investigations containing the remaining 9.1% of patients reported joint results from intra- and extra-abdominal flaps.
On average, the infection rate decreased by 81.3% ± 2.9% after surgery, with significantly more infection reduction for intra-abdominal flaps (88.2% ± 5.5 %) and extra-abdominal flaps (79.9% ± 4.3 %) (P = 0.009) [Table 3].
Complications
Fifty-seven (86.4%) of 66 articles reported donor, recipient, or medical complications. Only 42 of these articles were included in the meta-analysis since 15 investigations did not contain extractable data, either due to not reporting the number of patients who experienced a complication or not differentiating complications between various VLNT donor sites. There were no significant differences in donor site, recipient site, and medical complication rates between VLNT donor sites (P = 0.50 ; P = 0.95; P = 0.29) [Table 4]. There were also no statistically significant differences in donor site, recipient site, and medical complication rates when comparing intra-abdominal and extra-abdominal VLNT donor sites
Complication rates based on donor site
| Complication type | Donor sites | P-value | |||||||
| Omental | Jejunal mesenteric † | Groin | Lateral thoracic | Submental | Supraclavicular | Appendicular | Ileocecal | ||
| Donor, % | 10.4% | - | 11.0% | 12.2% | 3.8% | 6.1% | 0.0% | 0.0% | 0.50 |
| Recipient, % | 8.6% | - | 6.1% | 4.9% | 2.1% | 7.1% | 0.0% | 0.0% | 0.95 |
| Medical, % | 4.0% | - | 1.4% | - | 1.3% | - | - | - | 0.29 |
Lateral thoracic donor sites had the highest donor site complication rate (12.2%), while the omental VLNT donor site had the highest recipient site complication rate (8.6%) [Table 4].
Patient-reported outcomes
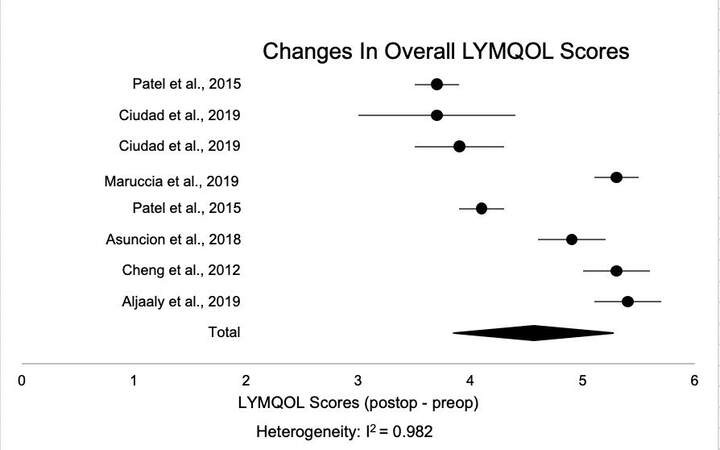
Sixteen articles (24.2%) reported validated patient-reported scale outcomes for VLNT patients, but only 11 articles (16.7%) were used in statistical analysis due to inconsistent reporting within the remaining studies. The most commonly used instruments were LYMQOL (Lymphedema Quality Of Life) questionnaires, employed in 12 (75.0%) out of 16 studies. There are 2 versions of the LYMQOL scale, one for upper extremity and one for lower extremity[22,23]. Other validated measures utilized were the Upper Limb Lymphedema 27 (ULL-27) questionnaire, the Lymphedema Life Impact Scale version 2 (LLISv2), and the Patient Scar Assessment Questionnaire (PSAQ), which were all utilized by one investigation each. The pain and heaviness visual analog scale (VAS) was used in two studies.
Submental flaps had the largest number of articles that included patient-reported outcomes, with 6 articles. This is followed by 5 articles, each reporting on patient-reported outcomes for omental and groin flaps. There were no studies that addressed patient-reported outcomes in patients who received appendicular, ileocecal, and jejunal mesenteric flaps.
LYMQOL results were analyzed and compared. There are 2 versions of the LYMQOL scale, one for upper extremity and one for lower extremity[22,23]. Overall, there was an improvement in each of the 5 LYMQOL domains: symptoms, body image/appearance, function, mood, and overall quality of life, after VLNT [Table 5]. When conducting a meta-analysis, studies containing intervention groups involving multiple donor sites were excluded. Based on this consideration, only studies addressing submental and omental VLNT could be included for analysis [Figure 3]. No statistically significant difference was found when comparing each LYMQOL domain for omental and submental VLNT (P = 0.06).
Figure 3. Forest plot depicting the average improvement in overall LYMQOL scores for each of these studies. Studies that did not report the standard deviations of the scores were excluded from this plot.
Patient-reported outcomes. A lower score in the functional, appearance, symptom, and mood domains of the LYMQOL reflect a more satisfactory patient response in those categories, while a higher score in the overall domain in the LYMQOL reflects a more satisfactory patient response.
| LYMQOL* | VAS* | Lymphedema life impact scale V2* | Patient scar Questionnaire* | Upper limb lymphedema Questionnaire* | |||||||||||||
| F | A | S | M | O | PN | H | O | P | PS | F | A | S | P | PS | SO | O | |
| Total | -14.7 | -6.2 | -8.1 | -6.7 | 4.1 | -4.0 | -5.4 | -4.3 | -1.8 | -1.0 | -1.0 | 1.8 | 1.5 | 20 | 12 | 19 | 18 |
| Donor | |||||||||||||||||
| Groin | -13.8 | -6.5 | -7.8 | -5.8 | 3.5 | -4.8 | -5.4 | -4.3 | - | - | - | - | - | 20 | 12 | 19 | 18 |
| Submental | -15.4 | -4.6 | -8.0 | -6.2 | 4.4 | - | - | - | - | - | - | - | - | - | - | - | - |
| Omentum | -18.1 | -10.0 | -10.2 | -11.6 | 4.7 | -3.2 | - | - | -1.8 | -1.0 | -1.0 | 1.8 | 1.5 | - | - | - | - |
| Supraclavicular† | -0.91 | -1.0 | -1.1 | -0.8 | 2.1 | - | - | - | - | - | - | - | - | - | - | - | - |
| Lateral thoracic† | -0.91 | -1.0 | -1.1 | -0.8 | 2.1 | - | - | - | - | - | - | - | - | - | - | - | - |
| Appendicular | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Ileocecal | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Jejunal Mesenteric | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Intra-abdominal Donor site | -18.1 | -10.0 | -10.2 | -11.6 | 4.7 | -3.2 | - | - | -1.8 | -1.0 | -1.0 | 1.8 | 1.5 | - | - | - | - |
| Extra-abdominal Donor site | -14.1 | -5.5 | -7.7 | -5.8 | 4.0 | -4.8 | -5.4 | -4.3 | - | - | - | - | - | 20 | 12 | 19 | 18 |
| Recipient site | |||||||||||||||||
| Upper extremity | -15.9 | -6.3 | -8.6 | -6.8 | 4.1 | -4.8 | -5.4 | -4.3 | -1.2 | -0.55 | -0.50 | 1.5 | 1.2 | 20 | 12 | 19 | 18 |
| Lower extremity | -2.9 | -2.3 | -2.1 | -2.4 | 4.8 | -3.2 | - | - | -2.6 | -1.5 | -1.7 | 2.3 | 2.0 | - | - | - | - |
Eight articles reported LYMQOL measures for patients who had upper limb lymphedema and 7 articles reported LYMQOL measures for patients with lower limb lymphedema. Overall, no statistical significance was achieved when comparing upper and lower recipient sites for each LYMQOL domain (P = 0.15).
Imaging outcomes
Thirty of the 66 articles (45.5%) evaluated imaging outcomes. Of these 30 studies, most (22, 73.3%) used lymphoscintigraphy. Seven of these studies looked for the presence of nodes after VLNT, with two of these studies reporting that the majority of transplanted nodes were functioning postoperatively. Sixteen studies examined lymphatic drainage patterns, and the majority (14, 87.5%) indicated that flow improved after VLNT. The findings of these investigations are summarized in Supplementary Table 4.
DISCUSSION
Lymphedema is a chronic, progressive condition that can significantly diminish the quality of life of patients[24]. Though conservative therapy is currently still the gold standard for management, evidence for physiologic procedures such as VLNT is increasing[25,26]. Given their recent development, this systematic review found that jejunal mesenteric, appendicular, and ileocecal donor sites have been relatively understudied and warrant more consideration in future research. Overall, standardization in protocols and outcome measures is lacking.
Clinical outcomes
There is limited data available to guide donor site selection in VLNT, leaving surgeon preference, considerations for patient preference, and prior surgery or anatomic concerns to determine current practice. Furthermore, the available studies implemented a variety of methodologies and study designs, which restricted direct comparisons between investigations and made it difficult to draw definitive conclusions regarding the optimal VLNT donor site
Overall, some outcomes were reported in the literature more uniformly than others. For instance, the majority of investigations reported limb measurements as an outcome to characterize the efficacy of the procedure. From these studies, the vast majority reported reductions in limb size [Supplementary Table 3]. It cannot be understated, however, that contrasting methodologies could significantly affect the generalizability of these results. Limbs were measured in circumference[27-29] or volume[30,31], though variances were also present beyond these two categories, including circumference rate reduction[32-34], upper/lower extremity lymphedema index[35-37], and volume ratios[38] [Supplementary Table 2]. The specific method used to obtain circumference and volume measurements differed between investigations as well
For the studies that reported reduction or discontinuation of conservative therapy following the procedure, it appeared that patients could rely less heavily on these treatments postoperatively. Variations in postoperative conservative treatment protocols and follow-up time points restricted direct comparisons between studies. There were also numerous investigations with unclear postoperative therapy protocols[30,31,44].
Infection rates were another more commonly reported outcome. It has been previously established in the literature that lymphedema increases the risk of developing cellulitis in the affected limb[45,46]. Specifically, the obstruction of lymphatic flow and accumulation of protein-rich colloid in the interstitium results in localized immunosuppression and a subsequent increase in infections[47]. Therefore, a procedure restoring lymphatic flow within the affected limb would be expected to mitigate the mechanism that propagates infection[47]. In this systematic review, only studies reporting the number of preoperative and postoperative episodes of cellulitis were included for meta-analysis purposes. All investigations reporting this outcome reported a successful reduction of postoperative infection following the VLNT. Particularly, patients who underwent intra-abdominal VLNT experienced a significant reduction in infectious episodes compared to those with an extra-abdominal donor site. Importantly, it should be noted that the majority of the intra-abdominal donor data regarding infection rate reduction was from omental VLNT. Therefore, more research is needed to clarify this advantage with intra-abdominal flaps, as ileocecal, appendiceal, and jejunal mesenteric VLNTs have especially limited evidence surrounding this outcome.
Another interesting finding related to the reduction of annual infectious episodes was observed when stratifying the data based on upper and lower limb recipient sites. Patients with upper limb lymphedema had a trend toward greater reduction (83.8 ± 3.4 %) in postoperative infectious episodes than those with lower extremity lymphedema (77.4 ± 4.8 %). Though lower extremity lymphedema patients are more likely to experience infection, the exact mechanism behind this predisposition is unclear in the literature[46]. Potentially, given that the lower extremities are in the dependent region of the body, disruptions in lymphatic flow could result in more significant accumulations of lymph, with markedly poorer responses to infection. This postulation could explain why, even after VLNT, the reduction in infectious episodes would be less substantial in comparison to upper limb recipient sites.
Intra-abdominal vs. extra-abdominal
In recent years, additional donor sites for lymphatic tissue have been found. There are several benefits to obtaining lymph nodes and tissue from the abdominal cavity, as it can mitigate the risk for donor-site lymphedema-a major concern when it comes to VLNTs from extra-abdominal sites[48]. Intra-abdominal sites also allow for the ability to harvest up to 3 vascularized flaps from 1 donor site[48]. With the possibility of laparoscopic harvest, the risk of donor-site morbidity may be reduced and minimal donor-site scars can be well-hidden[48,49].
The most common intra-abdominal flap is derived from the omentum[49]. The omentum is highly vascularized and large in size, with large lymphatic channels, and lymphatic lakes, which make it a potentially ideal donor site candidate[48-50]. While VLNTs from other intra-abdominal donor sites like the ileocecum and appendix are being explored, currently, there is limited data on the efficacy and safety of these specific flaps.
The literature overall reveals the potential for improved outcomes with intra-abdominal flaps. On average, patients who received intra-abdominal flaps had significantly fewer episodes of infection postoperatively. This is likely due to the great angiogenic and immunomodulatory potential of the omentum[51]. However, despite the absence of iatrogenic lymphedema in patients who received intra-abdominal flaps, omental VLNT had the highest rate of recipient-site complications and one of the highest donor-site complication rates reported. Concerning donor-site complications, intra-abdominal sources of lymph nodes possess unique risks that are inherent with these procedures, such as ventral hernias and small bowel obstruction[35]. Overall, when interpreting these results, it should be noted that since few studies specifically reported complications, it is likely that the true frequency of many complications for both extra-abdominal and intra-abdominal flaps was not captured.
While the current research on intra-abdominal VLNT donor sites is promising, it is still unclear whether the benefits are significant enough to overcome the additional risks that come with intra-abdominal surgery. More research needs to be done on the efficacy of intra-abdominal flaps, especially the non-omental intra-abdominal sites, and techniques refined and standardized to minimize the risk of donor-site complications.
Patient-reported outcomes
The inclusion of patient-reported measures is crucial in analyzing outcomes of lymphedema treatment. Previous studies have shown that the severity of limb edema may not correlate with the amount of change in patient-reported outcomes, as patients can report significant impairments even when volume changes may not be evident[52-54]. Unfortunately, the vast majority of studies (50 articles out of 66, 75.8%) in this systematic review did not include any patient-reported outcomes using validated questionnaires/scales. For the studies that did address PROs, the lack of standardization in reporting the results made it difficult to compare these outcomes across studies. This was likely due to the fact that earlier studies often used non-validated tools or non-lymphedema-specific tools[52]. However, once the LYMQOL scale was validated in 2010, it became the most commonly used tool[52]. Using this scale, there is a trend toward patients who received omental flaps reporting the greatest improvement in LYMQOL scores, while those who received lateral thoracic flaps had the least improvement. Interestingly, patients with lateral thoracic flaps also had the highest rate of donor site complications, which could potentially explain the reduced postoperative PROs scores for lateral thoracic VLNT.
The LYMQOL showed greater improvement in scores in functional, appearance, symptom, and mood domains for patients who underwent VLNT for upper limb lymphedema, but the overall quality of life improved more after VLNT to the lower extremity.
Limitations
Limitations of the present study should be recognized. Inconsistent reporting of data, as well as significant heterogeneity of study design and methodology, prevented meta-analysis with many of the reported outcomes. Additionally, small sample sizes for some VLNT donor sites could have impacted statistical outcomes and, in some instances, precluded any statistical analysis. Nevertheless, our study remains a comprehensive systematic review of the current outcome-based research on VLNT and should encourage future studies to standardize clinical staging, methodologies, and outcome measures.
CONCLUSION
VLNT is a promising treatment modality for many patients with lymphedema, which has previously been thought to be a progressive, chronic disease. New donor sites, such as the omental, appendiceal, ileocecal, and jejunal mesenteric, have offered possible advantages in mitigating the risk of donor-site lymphedema for patients while overall resulting in a greater reduction in infectious episodes in comparison to extra-abdominal donor sites. This warrants additional consideration in the literature. With more consistent methodology and reporting, patient-reported outcomes and clinical outcomes could be better compared between studies and offer more robust data to guide surgical practice in VLNT for lymphedema patients.
DECLARATIONS
Authors’ contributionsInitial literature search: Yaeger L
Made substantial contributions to conception and design of the study and performed data analysis and interpretation: Christensen JM, Raman S, Sanka SA, Ji J, Skolnick GB
Performed data acquisition, as well as provided substantial contributions to the manuscript: Raman S,
Provided significant guidance and feedback in manuscript editing process: Christensen JM, Skolnick GB
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot Applicable.
Consent for publicationNot Applicable.
Copyright© The Author(s) 2023.
Supplementary MaterialsREFERENCES
1. Sleigh BC, Manna B. Lymphedema. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537239/ [Last accessed on 16 Feb 2023].
2. Cormier JN, Askew RL, Mungovan KS, Xing Y, Ross MI, Armer JM. Lymphedema beyond breast cancer: a systematic review and meta-analysis of cancer-related secondary lymphedema. Cancer 2010;116:5138-49.
3. Grada AA, Phillips TJ. Lymphedema: pathophysiology and clinical manifestations. J Am Acad Dermatol 2017;77:1009-20.
5. Hinrichs CS, Watroba NL, Rezaishiraz H, et al. Lymphedema secondary to postmastectomy radiation: incidence and risk factors. Ann Surg Oncol 2004;11:573-80.
6. Granzow JW, Soderberg JM, Kaji AH, Dauphine C. Review of current surgical treatments for lymphedema. Ann Surg Oncol 2014;21:1195-201.
7. Ko DS, Lerner R, Klose G, Cosimi AB. Effective treatment of lymphedema of the extremities. Arch Surg 1998;133:452-8.
8. Ciudad P, Sabbagh MD, Agko M, et al. Surgical management of lower extremity lymphedema: a comprehensive review. Indian J Plast Surg 2019;52:81-92.
9. Raju A, Chang DW. Vascularized lymph node transfer for treatment of lymphedema: a comprehensive literature review. Ann Surg 2015;261:1013-23.
10. Cheng MH, Huang JJ, Nguyen DH, et al. A novel approach to the treatment of lower extremity lymphedema by transferring a vascularized submental lymph node flap to the ankle. Gynecol Oncol 2012;126:93-8.
11. Chang EI, Chu CK, Hanson SE, Selber JC, Hanasono MM, Schaverien MV. Comprehensive overview of available donor sites for vascularized lymph node transfer. Plast Reconstr Surg Glob Open ;8:e2675.
12. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71.
13. Institute of Medicine (US) Committee on Standards for Systematic Reviews of Comparative Effectiveness Research. Finding what works in health care: standards for systematic reviews. Eden J, Levit L, Berg A, Morton S, editors. Washington (DC): National Academies Press (US); 2011.
14. Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions 2020. Available from: https://training.cochrane.org/handbook [Last accessed on 16 Feb 2023].
15. McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol 2016;75:40-6.
16. ASPS Evidence Rating Scales. Available from: https://www.plasticsurgery.org/documents/medical-professionals/health-policy/evidence-practice/ASPS-Rating-Scale-March-2011.pdf [Last accessed on 16 Feb 2023].
17. Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health 2019;22:153-60.
19. R Software. R foundation for statistical computing. Available from: https://www.R-project.org/ [Last accessed on 16 Feb 2023].
20. Ma J, Liu W, Hunter A, Zhang W. Performing meta-analysis with incomplete statistical information in clinical trials. BMC Med Res Methodol 2008;8:56.
21. Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc 2016;104:240-3.
22. Wedin M, Fredrikson M, Ahlner E, et al. Validation of the lymphoedema quality of life questionnaire (LYMQOL) in swedish cancer patients. Acta Oncol 2020;59:365-71.
23. Keeley V, Crooks S, Locke J, Veigas D, Riches K, Hilliam R. . A quality of life measure for limb lymphoedema (LYMQOL). Available from: https://www.researchgate.net/publication/284904179_A_quality_of_life_measure_for_limb_lymphoedema_LYMQOL [Last accessed on 16 Feb 2023]
24. Brucker B, Zeltzer A, Seidenstuecker K, Hendrickx B, Adriaenssens N, Hamdi M. Breast cancer-related lymphedema: quality of life after lymph node transfer. Plast Reconstr Surg 2016;137:1673-80.
25. Kung TA, Champaneria MC, Maki JH, Neligan PC. Current concepts in the surgical management of lymphedema. Plast Reconstr Surg 2017;139:1003e-13e.
27. Engel H, Lin CY, Huang JJ, Cheng MH. Outcomes of lymphedema microsurgery for breast cancer-related lymphedema with or without microvascular breast reconstruction. Ann Surg 2018;268:1076-83.
28. Lin CY, Liu HE, Cheng MH. Factors associated with professional healthcare advice seeking in breast cancer-related lymphedema. J Surg Oncol 2020;121:67-74.
29. Koide S, Lin CY, Chen C, Cheng MH. Long-term outcome of lower extremity lymphedema treated with vascularized lymph node flap transfer with or without venous complications. J Surg Oncol 2020;121:129-37.
30. Ngo QD, Munot S, Mackie H, et al. Vascularized lymph node transfer for patients with breast cancer-related lymphedema can potentially reduce the burden of ongoing conservative management. Lymphat Res Biol 2020;18:357-64.
31. Granzow JW, Soderberg JM, Kaji AH, Dauphine C. An effective system of surgical treatment of lymphedema. Ann Surg Oncol 2014;21:1189-94.
32. Patel KM, Lin CY, Cheng MH. A prospective evaluation of lymphedema-specific quality-of-life outcomes following vascularized lymph node transfer. Ann Surg Oncol 2015;22:2424-30.
33. Ciudad P, Manrique OJ, Bustos SS, et al. Comparisons in long-term clinical outcomes among patients with upper or lower extremity lymphedema treated with diverse vascularized lymph node transfer. Microsurgery 2020;40:130-6.
34. Ciudad P, Manrique OJ, Bustos SS, et al. Combined microvascular breast and lymphatic reconstruction with deep inferior epigastric perforator flap and gastroepiploic vascularized lymph node transfer for postmastectomy lymphedema patients. Gland Surg 2020;9:512-20.
35. Kraft CT, Eiferman D, Jordan S, Skoracki RJ. Complications after vascularized jejunal mesenteric lymph node transfer: a 3-year experience. Microsurgery 2019;39:497-501.
36. Akita S, Tokumoto H, Yamaji Y, et al. Contribution of simultaneous breast reconstruction by deep inferior epigastric artery perforator flap to the efficacy of vascularized lymph node transfer in patients with breast cancer-related lymphedema. J Reconstr Microsurg 2017;33:571-8.
37. Visconti G, Tartaglione G, Bartoletti R, Salgarello M. Compartimental harvesting of dual lymph node flap from the right supraclavicular area for the treatment of lower extremity lymphedema: a case series. J Plast Reconstr Aesthet Surg 2019;72:211-5.
38. Dionyssiou D, Demiri E, Sarafis A, Goula CO, Tsimponis A, Arsos G. Functional lymphatic reconstruction with the “Selected Lymph Node” technique guided by a SPECT-CT lymphoscintigraphy. J Surg Oncol 2019;120:911-8.
39. Vignes S, Blanchard M, Yannoutsos A, Arrault M. Complications of autologous lymph-node transplantation for limb lymphoedema. Eur J Vasc Endovasc Surg 2013;45:516-20.
40. Brorson H, Höijer P. Standardised measurements used to order compression garments can be used to calculate arm volumes to evaluate lymphoedema treatment. J Plast Surg Hand Surg 2012;46:410-5.
41. Tierney S, Aslam M, Rennie K, Grace P. Infrared optoelectronic volumetry, the ideal way to measure limb volume. Eur J Vasc Endovasc Surg 1996;12:412-7.
42. Sun F, Hall A, Tighe MP, et al. Perometry versus simulated circumferential tape measurement for the detection of breast cancer-related lymphedema. Breast Cancer Res Treat 2018;172:83-91.
43. Moffatt C, Doherty D, Morgan P, eds. Best practice for the management of lymphoedema: an international consensus. Available from: https://www.woundsinternational.com/resources/details/best-practice-for-the-management-of-lymphoedema-an-international-consensus [Last accessed on 16 Feb 2023].
44. Chang EI, Ibrahim A, Liu J, et al. Optimizing quality of life for patients with breast cancer-related lymphedema: a prospective study combining diep flap breast reconstruction and lymphedema surgery. Plast Reconstr Surg 2020;145:676e-85e.
45. Dupuy A, Benchikhi H, Roujeau JC, et al. Risk factors for erysipelas of the leg (cellulitis): case-control study. BMJ 1999;318:1591-4.
46. Park SI, Yang EJ, Kim DK, Jeong HJ, Kim GC, Sim YJ. Prevalence and epidemiological factors involved in cellulitis in korean patients with lymphedema. Ann Rehabil Med 2016;40:326-33.
47. Vignes S, Arrault M, Dupuy A. Factors associated with increased breast cancer-related lymphedema volume. Acta Oncol 2007;46:1138-42.
48. Chu CK, Schaverien MV, Chang EI, Hanson SE, Hanasono MM, Selber JC. Intra-abdominal lymph nodes: a privileged donor site for vascularized lymph node transfer. Plast Reconstr Surg Glob Open 2020;8:e2673.
49. Danforth R, Skoracki R. Intra-abdominal donors for vascularized lymph node transfer: an update and review. Plast Aesthet Res 2022;8:48.
50. Panje WR, Pitcock JK, Vargish T. Free omental flap reconstruction of complicated head and neck wounds. Otolaryngol Head Neck Surg 1989;100:588-93.
51. Nicola V. Omentum a powerful biological source in regenerative surgery. Regen Ther 2019;11:182-91.
52. Coriddi M, Wee C, Meyerson J, Eiferman D, Skoracki R. Vascularized Jejunal Mesenteric lymph node transfer: a novel surgical treatment for extremity lymphedema. J Am Coll Surg 2017;225:650-7.
53. Hormes JM, Bryan C, Lytle LA, et al. Impact of lymphedema and arm symptoms on quality of life in breast cancer survivors. Lymphology 2010;43:1-13.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Raman S, Sanka SA, Ji J, Yaeger L, Skolnick GB, Christensen JM. Vascularized lymph node transfer for the treatment of lymphedema: a systematic review and meta-analysis of clinical and patient-reported outcomes. Plast Aesthet Res 2023;10:6. http://dx.doi.org/10.20517/2347-9264.2022.62
AMA Style
Raman S, Sanka SA, Ji J, Yaeger L, Skolnick GB, Christensen JM. Vascularized lymph node transfer for the treatment of lymphedema: a systematic review and meta-analysis of clinical and patient-reported outcomes. Plastic and Aesthetic Research. 2023; 10(1): 6. http://dx.doi.org/10.20517/2347-9264.2022.62
Chicago/Turabian Style
Raman, Shreya, Sai Anusha Sanka, Jenny Ji, Lauren Yaeger, Gary B. Skolnick, Joani M. Christensen. 2023. "Vascularized lymph node transfer for the treatment of lymphedema: a systematic review and meta-analysis of clinical and patient-reported outcomes" Plastic and Aesthetic Research. 10, no.1: 6. http://dx.doi.org/10.20517/2347-9264.2022.62
ACS Style
Raman, S.; Sanka SA.; Ji J.; Yaeger L.; Skolnick GB.; Christensen JM. Vascularized lymph node transfer for the treatment of lymphedema: a systematic review and meta-analysis of clinical and patient-reported outcomes. Plast. Aesthet. Res. 2023, 10, 6. http://dx.doi.org/10.20517/2347-9264.2022.62
About This Article
Special Issue
Copyright
Data & Comments
Data

 Cite This Article 11 clicks
Cite This Article 11 clicks












Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.