Artificial intelligence in plastic surgery: current developments and future perspectives
Abstract
Driven by the rapid development of big data, the amount of clinical data, including complex information, is expanding. Traditional data analysis methods cannot meet the need for mining data information, and artificial intelligence (AI) solves this problem. AI is increasingly being incorporated into modern medical practice. Algorithms provided by AI support advanced analysis and provide individualized aid to optimize medical decision-making. In plastic surgery, AI has made many breakthroughs in diagnosis, pre-operative surgical design, treatment decisions, and patient management. Plastic surgeons must recognize AI’s potential development and limitations. This review describes the current application of AI in plastic surgery and discusses the challenges and problems that need to be solved. This study aims to foster the application of this new AI technology in clinical practice.
Keywords
INTRODUCTION
Artificial intelligence (AI) is a technology that simulates human cognition, including interpreting and analyzing complex data to solve problems. AI has been applied in face recognition, speech conversion, and search engine recommendations. The application of AI in medicine and healthcare is increasing[1]. AI was first applied to image-recognition diagnostic tasks. Image-recognition technology alerts physicians seeking small lesions that are easily overlooked[2]. AI has been widely used in diabetes management[3], dermatology[4], and thoracic surgery[5].
Physicians need to make rapid and complex decisions based on the analysis of patients and clinical elements. Diagnosis and treatment decisions may be influenced by cognitive biases, personality traits, the emotions of the physicians, and even the environment. All therapeutic decision-making processes have a certain degree of variability, uncertainty, and errors[6]. AI helps overcome the limitations of human behavior because it can support medical decision-making and reasoning. On the other hand, with the development of informatization, the data collected from each patient pre- and postoperatively has grown exponentially. Furthermore, patient-generated health data and off-the-shelf wearable sensors obtain substantial data. This stored digital information is called “big data”[7]. Faced with the need to analyze and utilize big data to solve complex clinical problems, manual independent analysis is insufficient. It is vital to use AI to manage a large amount of data.
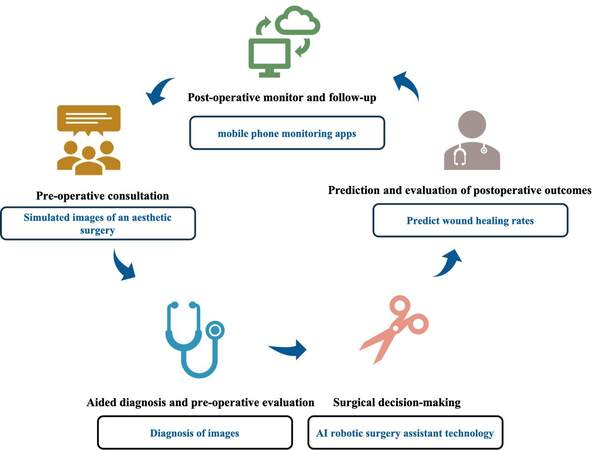
Plastic surgery is a creative discipline that treats diseases like other surgery departments and improves the appearance of the human body. Thus, AI technologies can be applied in pre-operative consultations, diagnosis, therapeutic decisions, postoperative patient evaluation, and follow-up [Figure 1]. These features will be beneficial in reducing medical errors, improving work efficiency, and decreasing resource waste.
This review summarizes the essential technical elements and concepts involved in the techniques provided by AI, describes the status of AI applications in plastic surgery and discusses the prospects and difficulties of deployment. Plastic surgeons should quickly move to the forefront of AI technology to promote the development of the discipline.
SUBFIELDS AND CONCEPTS OF AI
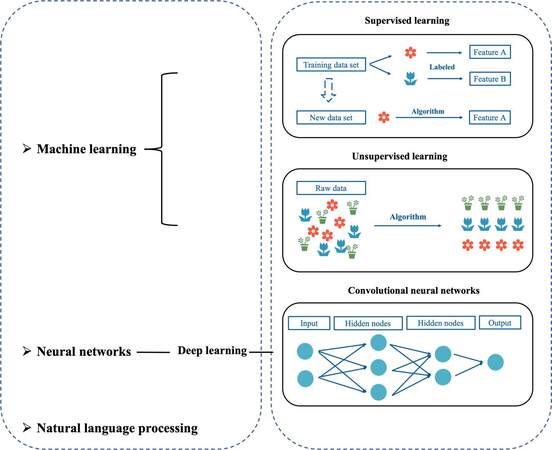
AI is a computer algorithm that analyzes data and deals with complex problems in various applications without human involvement. AI creates systems or methods for analyzing information. The most common areas of AI research in medicine are machine learning (ML), neural networks (NN), and natural language processing [Figure 2].
Machine learning
ML is a computer algorithm that autonomously learns without specific programming. For a given task, the model learns from examples and identifies patterns and trends in data using ML[8]. As the number of examples and the times of test repetition increase, the algorithm becomes more accurate and predictive. The establishment step of ML includes data preparation and selection, training the algorithm, obtaining a series of related output results, implementation of the software and analysis, and system validation. The accuracy of the system is gradually improved with algorithm adjustment and feedback.
ML is divided into supervised, unsupervised, semi-supervised, and transfer learning. Supervised learning learns from the features (input) of the data to extract the characteristics, then labels (output) and verifies the unclassified data[9]. Supervised learning is primarily used for classification. Depending on the instances in which the category is known, supervised learning is trained to observe and label new examples. Predictive ML models[10] and face recognition are supervised learning methods. Unsupervised learning uses clustering and dimensionality reduction methods to analyze unclassified data records; however, it is necessary to provide a semantic explanation by human interrogation[9]. Unsupervised learning is primarily used to explore and summarize existing data and has been applied to molecular genetic and genomic data analysis. Semi-supervised learning occurs between supervised and unsupervised learning because it can use labeled and unlabeled data to learn.
Neural networks
NNs use multiple layers of calculations to imitate humans to solve complex information and draw conclusions. NN has many “nodes”. The network can produce optimal predictive accuracy by adjusting the weight of the nodes[11].
Deep learning is a branch of NN characterized by multiple hidden node layers. It has a more extensive network scale to accurately express complex interrelationships[12]. Without external guidance, deep learning algorithms can discover the model’s essential features, make predictions on a vast amount of information, and provide an output. The commonly used NNs are “convolutional neural networks (CNNs)”, a type of deep learning architecture. The AI technology used to distinguish between malignant melanoma and benign nevi is based on the CNN system[4]. CNN is an architecture within AI medicine due that is exceptionally efficient at natural signals such as speech and image processing.
Natural language processing
NLP establishes a technique for understanding, interpreting, and manipulating human language[13]. The customer service software that automatically answers questions is NLP technology. NLP can identify and extract data from a physician’s narrative documentation in electronic medical record systems.
Computer vision
Computer vision uses data from ambient sensors to identify the contents of images or videos for medical services, for example, improving medical safety by monitoring critically ill patients in the intensive care unit[14].
CURRENT DEVELOPMENT OF AI IN PLASTIC SURGERY
Pre-operative consultation
ML has proven to be a valuable tool for analyzing and extracting information from vast amounts of data, especially social media. The comments on the website Realself.com is summarized using an ML approach to identify the most concerning pre- and postoperative problems for mentoplasty patients[15]. “Eligibility for surgery” and “options to revise surgery” are the most significant concerns pre- and postoperatively[15]. In another study, AI technology from the Cognovi Lab used emotional analysis of plastic surgery vocabulary on social media and found that patients have the highest emotional engagement with the word “liposuction”[16]. From the point of view of emotion, this study quantitatively analyzes the impact of plastic surgery terms on patient motivation and subsequent responses using much data from social media. It helps guide plastic surgeons in publicizing plastic surgery from an emotion-driven economic decision-making perspective[16]. Discovering the focus of patient attention on social media helps surgeons better predict and solve potential patient problems, communicate with accurate information, write suitable patient education materials, and improve patient satisfaction.
During the stage of online patient consultation, artificial intelligent virtual assistants (AIVA) using NLP technology understands the intent of human speech and provide answers in the form of dialogue. A study used AIVA to chat with patients on common plastic surgery topics[17]. The overall answer accuracy of the plastic surgery AIVA was 92.3%, and 83.3% of the participants thought the answers were correct[17]. The popularization and application of this technology will help free plastic surgeons from primary medical consultation.
Most plastic surgery treatment plans are highly personalized and relevant to the aesthetic view of the patient and the surgeon. Patients usually express their aesthetic views and desirable appearance before surgery. AI technology can be used to design simulated images to provide references for surgery and improve the procedure plan. BreastGAN is a portable AI-equipped tool that uses breast images of patients with bilateral augmentation to train a NN algorithm[18]. BreastGAN using pre-operative breast photos automatically simulates breast augmentation outcomes[18]. In rhinoplasty, an AI model can produce simulated images of aesthetic rhinoplasty that meet the surgeon’s aesthetic criteria[19]. The consistency of the simulated images and rhinoplasty outcomes is 92%[19]. These technologies provide patients with AI-driven predictions to help them make more informed decisions that help reduce reoperation rates and improve postoperative satisfaction.
AI can objectively evaluate facial beauty. Various human referees grade a collection of female facial images, and supervised classification is used to automatically extract facial features[20]. Then, supervised learning uses proportion analysis via image-based assessments of facial beauty[20]. Exaggerated or unnatural plastic surgery outcomes can be avoided by objectively evaluating facial beauty using this technology. However, the application of this technology may destroy the diversity of aesthetics simultaneously, resulting in similar facial appearances after surgery in different patients.
In contrast, we must recognize that some AI technologies negatively impact medical propaganda. For example, the wide use of photo-editing technology has made video presentations more credible in a medical advertisement. However, advanced AI deep learning and computational modeling (collectively known as “deepfakes”) can alter people’s faces, facial expressions, and body movements in videos. When deepfakes were used to alter a patient’s postoperative video outcome[21], they exaggerated the effects of plastic surgery.
Aided diagnosis and pre-operative evaluation
AI was first applied to image diagnosis. The most used computer-aided diagnostic system in plastic surgery is the classification of skin lesions by CNNs, such as distinguishing between keratinocyte carcinomas and benign seborrheic keratoses, malignant melanomas, and benign nevi[4]. The study showed that the CNN algorithm trained by open-source images had better sensitivity and specificity in recognizing dermoscopic images than doctors from junior to chief physicians[4]. Another multi-center prospective study demonstrated that the AI has a similar sensitivity and specificity to experts for identifying melanoma images taken with smartphones and digital single-lens reflex cameras[22].
AI has been used in the computational analysis of craniosynostosis from computed tomography (CT) images[23]. This ML technology uses cranial suture fusion indices and deformation and curvature discrepancy averages across five cranial bones and six suture regions as features to diagnose craniosynostosis. It has a 92.7% sensitivity, a 98.9% specificity, and a 95.7% probability of correct classification, comparable to experienced radiologists[23]. Another software named ShapeWorks analyzes the skull shape using ML to predict the severity of distal craniosynostosis based on CT images[24].
For diagnosing rare diseases, facial analysis software already uses unsupervised ML to recognize dysmorphic craniofacial features on two-dimensional photographs to diagnose correctly[25]. These technologies assist physicians in making quick diagnoses and reducing errors. Furthermore, the application of AI technologies in smartphone applications makes it more convenient for patients to screen for diseases.
Surgical decision-making and performance
AI provides reference information during surgery to assist in decision-making. Early identification of free-flap ischemia and congestion is essential in the microsurgical reconstruction of free flaps. A smartphone application called SilpaRamanitor was created to assess tissue perfusion based on skin color for postoperative tissue perfusion monitoring[26]. The algorithm recognizes skin color as a feature to simulate blood perfusion conditions. The accuracy rate of blood perfusion recognition was up to 95%. This application enables early detection of surgical risks and helps salvage tissue quickly.
The AI robotic surgery system is a navigation aid for surgeons during robot-assisted surgeries. Supervised autonomous procedures can recognize anatomical structures and conduct surgical navigation to aid intraoperative decision-making[27]. Robotic surgery assistant technology is used in cleft lip and palate repair surgery[28]. It is based on deep learning to help lower the technical threshold and improve surgical outcomes[28]. In the future, an autonomous robotic surgical system using AI technology will be developed to provide precise surgical treatment, improve surgical efficiency, reduce complications, and shorten the length of hospital stays.
Head-mounted cameras and wearable technology have increased the use of surgical video data. AI analyzes videos to identify and extract high-quality surgical data. Surgical video analysis improves surgical techniques[29] and enhances surgeons’ surgical abilities[30]. The robust data retrieval and processing capabilities of AI substantially reduce the time for plastic surgeons to gain experience and knowledge. Autonomous surgical systems guided by AI could improve surgical outcomes in underdeveloped areas.
Prediction and evaluation of postoperative outcomes
Complex models built by AI use clinical data, imaging, and histopathological information to select the optimal treatment plan and assess outcomes. These models are superior to traditional regression models. The predictive outcome model was first applied to wound healing in plastic surgery. The RReliefF algorithm was used to predict wound healing rates based on the wound area, the patient’s age, and the time from wound appearance to the beginning of treatment[31]. For burn treatment and triage, the burn healing time was predicted by the artificial neural network (ANN) analysis of the burn spectra taken on the third day after the burn using the reflectance spectrometer[32]. The overall accuracy of this method is 86%, which is significantly better than the accuracy of direct visual examination. The system is sufficient as an effective tool for physicians unfamiliar with burn systems to assess burn severity. The ANN was also used to predict the survival of burn patients and is based on the observations of the burn patient’s total body surface area, rescue time, admission time, surgery, and inhalation injury[33]. In the training phase, ANN has reached a 90% accuracy[33]. ANN effectively predicts surgical site infection in patients who underwent free-flap reconstruction after surgery for head and neck cancer[34]. This prediction efficiency is significantly higher than conventional logistic regression[34]. These predictions help formulate reasonable patient management strategies. Medical resources lean toward patients with poor prognoses to achieve the optimal allocation of medical resources.
The effect of aesthetic evaluation after surgery is usually highly subjective for facial aesthetic surgery. AI provides an objective evaluation standard for the effect of aesthetic surgery. AI uses deep learning methods to extract facial features and uses CNN to evaluate apparent age[35] and facial attractiveness[36]. ML is also used to assess facial beauty based on facial proportions according to features like the golden ratio, texture, shape, and color[37]. These techniques provide an objective assessment of patient aesthetic improvement after surgery. In orthognathic treatment, the algorithm found that most patients (66.7%) were younger in apparent age and improved in attractiveness after surgery[36]. After rhinoplasty, the facial attractiveness of patients is increased[38], and perceived age relative to the patient’s actual age is decreased[39], meaning that rhinoplasty reverses signs of facial aging. Using CNN to evaluate the facial attractiveness of treated cleft patients, the AI evaluation of cleft patients was comparable to human ratings[40].
Expression of emotions can be analyzed by AI using facial images that analyze the effects of surgery from the perspective of emotional aesthetics. Noldus FaceReader uses ML to measure the relative proportions of emotion in facial expressions obtained from video data[41]. One study considered fifteen facial palsy patients who underwent cross-facial nerve grafting and free gracilis muscle transfer; the study evaluated happiness expressed in smiles[41]. The patients’ postoperative smiling videos showed an increase in happy expressions compared to pre-operative smiling videos[41]. In another study, AI emotion detection software found that people with facial paralysis showed less joy and more negative emotion in their smiles than ordinary people[42]. These techniques provide a way to quantify changes in facial emotion before and after surgery objectively.
AI can identify gender through facial recognition. Using facial recognition NN, facial recognition features are used to evaluate gender-typing of male-to-female transgender patients before and after surgery[43]; the study revealed that gender-typing changes and confidence in femininity are significantly improved after facial feminization surgery[43].
Postoperative monitoring and follow-up
The widespread application of wearable technology and mobile health technologies has made remote technologies for patient monitoring and communication more convenient[44]. Surgeons monitor the postoperative outcomes using patient-generated selfies or other mobile phone monitoring apps. These technologies save time for follow-up. They also give surgeons timely follow-up information that can be digitized to facilitate analysis and integration.
LIMITATIONS AND CHALLENGES
Despite AI achieving encouraging results in medicine, privacy protection and ethical issues related to its application still need to be discussed.
ML algorithms require training with big data to achieve satisfactory performance. However, medical-related health data is highly sensitive, and it is crucial to protect the privacy and ownership of the data. First, better-regulated and restrictive laws are needed to protect personal information. Second, the data requires adequate supervision by regulators to avoid personal information leakage. Finally, data protection technology advances and industry personnel's ethical discipline are critical. Big data needs de-identification and data sharing. Building a multi-center data platform to collect high-quality and standardized big data is the foundation for the development of AI. There must be strict requirements for informed consent, data protection, and cybersecurity[45]. Programmers, policymakers, physicians, and patients should participate in real-world algorithmic decision-making processes to maximize fairness and respect privacy[46].
Another challenge is that most medical data is heterogeneous. Collecting, constructing, and standardizing the data to meet analytic needs is critical. For example, providing high-quality standardized pre- and postoperative photographs is critical for information collection in plastic surgery.
Supervised learning needs experienced physicians to label features (input). Physicians’ capacity variance or error in labeling results in biased datasets. Systematic bias leads to unrepresentative conclusions. For algorithms, it is challenging for physicians to assess the weights of various parameters. The complex architecture becomes a black box; the lack of an explanation for a particular output becomes the “black box dilemma”. When physicians’ understanding and interpretation of AI diagnostic or predictive models are insufficient, they will be reluctant to use AI models. The interpretability of AI algorithms is crucial. Full cooperation and communication with computer scientists are needed for the surgeons’ success.
Algorithmic procedures of AI need to ensure correct medical ethical values. The programmer should take measures to monitor technological development to avoid medical harm[47]. If the algorithm is set up with an inherent ethical error, it will eventually result in an error output. Before AI is applied to clinical practice, it is essential to generate fair laws to regulate the behavior of AI algorithms. However, legislation that is too strict should be avoided to limit the development of AI.
AI helps to free medical practitioners from repetitive and time-consuming simple tasks. However, AI’s limitations should be recognized. First, AI cannot wholly replace physicians in diagnosis and decision-making. In many cases, AI is currently used with conditional restrictions, and the algorithm’s output is only an association[48]. It is necessary to evaluate whether the output results can be applied to specific clinical patients and scenarios by physicians. Second, AI exacerbates pre-existing problems such as overdiagnosis, overdetection, and overtreatment[49]. Surgeons need to fully understand AI's pros and cons to promote the application and development of AI in medicine.
CONCLUSION
AI has been increasingly applied in healthcare settings, promoting the development of pre-operative evaluation, prognosis prediction, patient management, and postoperative monitoring. Many complex AI algorithms can learn from data and refine algorithms through learning. Physicians are also needed to optimize algorithms.
Although the application of AI in plastic surgery is still in its infancy, and most studies have not entered clinical practice, the development and prospects of AI remain full of expectations. It is necessary for plastic surgeons to fully understand and apply these technologies to solve various clinical and research problems. AI can provide patients with safer and more efficient medical services in the future.
DECLARATIONS
AcknowledgmentsThe authors thank AiMi Academic Services (www.aimieditor.com) for English language editing and review services.
Authors’ contributionsDesigned the study, searched the literature, and wrote the manuscript: Qin F
Made substantial contributions to conception and revised the manuscript: Gu J
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Autor(s) 2023.
REFERENCES
1. Buch VH, Ahmed I, Maruthappu M. Artificial intelligence in medicine: current trends and future possibilities. Br J Gen Pract 2018;68:143-4.
2. Saba L, Biswas M, Kuppili V, et al. The present and future of deep learning in radiology. Eur J Radiol 2019;114:14-24.
3. Contreras I, Vehi J. Artificial intelligence for diabetes management and decision support: literature review. J Med Internet Res 2018;20:e10775.
4. Esteva A, Kuprel B, Novoa RA, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature 2017;542:115-8.
5. Chen Z, Zhang Y, Yan Z, et al. Artificial intelligence assisted display in thoracic surgery: development and possibilities. J Thorac Dis 2021;13:6994-7005.
6. Saposnik G, Redelmeier D, Ruff CC, Tobler PN. Cognitive biases associated with medical decisions: a systematic review. BMC Med Inform Decis Mak 2016;16:138.
7. Kurmis AP, Ianunzio JR. Artificial intelligence in orthopedic surgery: evolution, current state and future directions. Arthroplasty 2022;4:9.
9. Handelman GS, Kok HK, Chandra RV, Razavi AH, Lee MJ, Asadi H. eDoctor: machine learning and the future of medicine. J Intern Med 2018;284:603-19.
10. Kanevsky J, Corban J, Gaster R, Kanevsky A, Lin S, Gilardino M. Big data and machine learning in plastic surgery: a new frontier in surgical innovation. Plast Reconstr Surg 2016;137:890e-7e.
11. Schwarzer G, Vach W, Schumacher M. On the misuses of artificial neural networks for prognostic and diagnostic classification in oncology. Statist Med 2000;19:541-61.
12. Lee JG, Jun S, Cho YW, et al. Deep learning in medical imaging: general overview. Korean J Radiol 2017;18:570-84.
13. Nadkarni PM, Ohno-Machado L, Chapman WW. Natural language processing: an introduction. J Am Med Inform Assoc 2011;18:544-51.
14. Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med 2019;25:44-56.
15. Patel R, Tseng CC, Choudhry HS, Lemdani MS, Talmor G, Paskhover B. Applying machine learning to determine popular patient questions about mentoplasty on social media. Aesthetic Plast Surg 2022;46:2273-9.
16. Levites HA, Thomas AB, Levites JB, Zenn MR. The use of emotional artificial intelligence in plastic surgery. Plast Reconstr Surg 2019;144:499-504.
17. Boczar D, Sisti A, Oliver JD, et al. Artificial intelligent virtual assistant for plastic surgery patient’s frequently asked questions: a pilot study. Ann Plast Surg 2020;84:e16-21.
18. Chartier C, Watt A, Lin O, Chandawarkar A, Lee J, Hall-Findlay E. BreastGAN: artificial intelligence-enabled breast augmentation simulation. Aesthet Surg J Open Forum 2022;4:ojab052.
19. Chinski H, Lerch R, Tournour D, Chinski L, Caruso D. An artificial intelligence tool for image simulation in rhinoplasty. Facial Plast Surg 2022;38:201-6.
20. Gunes H, Piccardi M. Assessing facial beauty through proportion analysis by image processing and supervised learning. Int J Hum Comput Stud 2006;64:1184-99.
21. Crystal DT, Cuccolo NG, Ibrahim AMS, Furnas H, Lin SJ. Photographic and video deepfakes have arrived: how machine learning may influence plastic surgery. Plast Reconstr Surg 2020;145:1079-86.
22. Phillips M, Marsden H, Jaffe W, et al. Assessment of accuracy of an artificial intelligence algorithm to detect melanoma in images of skin lesions. JAMA Netw Open 2019;2:e1913436.
23. Mendoza CS, Safdar N, Okada K, Myers E, Rogers GF, Linguraru MG. Personalized assessment of craniosynostosis via statistical shape modeling. Med Image Anal 2014;18:635-46.
24. Bhalodia R, Dvoracek LA, Ayyash AM, Kavan L, Whitaker R, Goldstein JA. Quantifying the severity of metopic craniosynostosis: a pilot study application of machine learning in craniofacial surgery. J Craniofac Surg 2020;31:697-701.
25. Ferry Q, Steinberg J, Webber C, et al. Diagnostically relevant facial gestalt information from ordinary photos. Elife 2014;3:e02020.
26. Kiranantawat K, Sitpahul N, Taeprasartsit P, et al. The first smartphone application for microsurgery monitoring: silpaRamanitor. Plast Reconstr Surg 2014;134:130-9.
27. Shademan A, Decker RS, Opfermann JD, Leonard S, Krieger A, Kim PC. Supervised autonomous robotic soft tissue surgery. Sci Transl Med 2016;8:337ra64.
28. Li Y, Cheng J, Mei H, Ma H, Chen Z, Li Y. CLPNet: cleft lip and palate surgery support with deep learning. Annu Int Conf IEEE Eng Med Biol Soc 2019;2019:3666-72.
29. Turner AE, Abu-Ghname A, Davis MJ, Ali K, Winocour S. Role of simulation and artificial intelligence in plastic surgery training. Plast Reconstr Surg 2020;146:390e-1e.
30. Grenda TR, Pradarelli JC, Dimick JB. Using surgical video to improve technique and skill. Ann Surg 2016;264:32-3.
31. Robnik-šikonja M, Cukjati D, Kononenko I. Comprehensible evaluation of prognostic factors and prediction of wound healing. Artif Intell Med 2003;29:25-38.
32. Yeong EK, Hsiao TC, Chiang HK, Lin CW. Prediction of burn healing time using artificial neural networks and reflectance spectrometer. Burns 2005;31:415-20.
33. Estahbanati HK, Bouduhi N. Role of artificial neural networks in prediction of survival of burn patients-a new approach. Burns 2002;28:579-86.
34. Kuo PJ, Wu SC, Chien PC, et al. Artificial neural network approach to predict surgical site infection after free-flap reconstruction in patients receiving surgery for head and neck cancer. Oncotarget 2018;9:13768-82.
35. Liao H, Yan Y, Dai W, Fan P. Age estimation of face images based on CNN and divide-and-rule strategy. Math Model Eng Probl 2018;2018:1-8.
36. Patcas R, Bernini DAJ, Volokitin A, Agustsson E, Rothe R, Timofte R. Applying artificial intelligence to assess the impact of orthognathic treatment on facial attractiveness and estimated age. Int J Oral Maxillofac Surg 2019;48:77-83.
37. Iyer TKR, Nersisson R, Zhuang Z, Joseph Raj AN, Refayee I. Machine learning-based facial beauty prediction and analysis of frontal facial images using facial landmarks and traditional image descriptors. Comput Intell Neurosci 2021;2021:4423407.
38. Khetpal S, Peck C, Parsaei Y, et al. Perceived age and attractiveness using facial recognition software in rhinoplasty patients: a proof-of-concept study. J Craniofac Surg 2022;33:1540-4.
39. Dorfman R, Chang I, Saadat S, Roostaeian J. Making the subjective objective: machine learning and rhinoplasty. Aesthet Surg J 2020;40:493-8.
40. Patcas R, Timofte R, Volokitin A, et al. Facial attractiveness of cleft patients: a direct comparison between artificial-intelligence-based scoring and conventional rater groups. Eur J Orthod 2019;41:428-33.
41. Boonipat T, Asaad M, Lin J, Glass GE, Mardini S, Stotland M. Using artificial intelligence to measure facial expression following facial reanimation surgery. Plast Reconstr Surg 2020;146:1147-50.
42. Dusseldorp JR, Guarin DL, van Veen MM, Jowett N, Hadlock TA. In the eye of the beholder: changes in perceived emotion expression after smile reanimation. Plast Reconstr Surg 2019;144:457-71.
43. Chen K, Lu SM, Cheng R, et al. Facial recognition neural networks confirm success of facial feminization surgery. Plast Reconstr Surg 2020;145:203-9.
44. Piwek L, Ellis DA, Andrews S, Joinson A. The rise of consumer health wearables: promises and barriers. PLoS Med 2016;13:e1001953.
46. Lepri B, Oliver N, Pentland A. Ethical machines: the human-centric use of artificial intelligence. iScience 2021;24:102249.
47. Keskinbora KH. Medical ethics considerations on artificial intelligence. J Clin Neurosci 2019;64:277-82.
48. Maddox TM, Rumsfeld JS, Payne PRO. Questions for artificial intelligence in health care. JAMA 2019;321:31-2.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Qin F, Gu J. Artificial intelligence in plastic surgery: current developments and future perspectives. Plast Aesthet Res 2023;10:3. http://dx.doi.org/10.20517/2347-9264.2022.72
AMA Style
Qin F, Gu J. Artificial intelligence in plastic surgery: current developments and future perspectives. Plastic and Aesthetic Research. 2023; 10(1): 3. http://dx.doi.org/10.20517/2347-9264.2022.72
Chicago/Turabian Style
Qin, Feng, Jianying Gu. 2023. "Artificial intelligence in plastic surgery: current developments and future perspectives" Plastic and Aesthetic Research. 10, no.1: 3. http://dx.doi.org/10.20517/2347-9264.2022.72
ACS Style
Qin, F.; Gu J. Artificial intelligence in plastic surgery: current developments and future perspectives. Plast. Aesthet. Res. 2023, 10, 3. http://dx.doi.org/10.20517/2347-9264.2022.72
About This Article
Copyright
Data & Comments
Data
 Cite This Article 24 clicks
Cite This Article 24 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.