Workhorse flaps for thumb reconstruction
Abstract
Posttraumatic thumb defects result in significant functional impairment. Multiple reconstructive procedures have been described for the management and improvement of function. Compared with no treatment, all reconstructive methods are beneficial. Each of the available procedures may be more applicable under certain conditions, can offer great benefits, and have its own downsides as well. With a thorough assessment and meticulous technique, the results of thumb reconstruction can be excellent. We present a review of the current reconstructive procedures for traumatic thumb amputation.
Keywords
INTRODUCTION
The thumb is the “master digit” of the hand and is involved in 40% of hand function. The thumb is special due to its ability of opposition, which enables in carrying out most routine daily activities[1].
Fingertip amputations that result in a wound up to 1 cm2 can be managed conservatively. Non-surgical management of such wounds using semi-occlusive dressing represents an effective management strategy in terms of providing satisfactory functional and aesthetic results, good pulp thickness, adequate nail growth, and restoration of sensation as well. Reconstruction of the thumb defects due to posttraumatic causes needs a proper assessment of the defect, and the type of reconstruction will vary depending on the size and geometry of the defect (Dorsal oblique, Volar, Transverse). Factors like age, sex, hand dominance and nature of work will influence the reconstructive plan. Patient-oriented reconstructive plans are always essential, which fit the need of the patient with proper clinical guidance. The patient should be informed about the information regarding the nature of surgery and outcomes of the procedure before planning. An informed and motivated patient is vital and valuable in the successful outcome of the reconstruction[2].
The goals of thumb reconstruction are length restoration, maintenance of joint stabilization, and range of motion, as well as restoration of sensation. These above attributes, along with a stable soft tissue cover, are the essential parameters of thumb reconstruction.
THE RECONSTRUCTIVE OPTIONS
The reconstruction of the posttraumatic thumb defect depends on many patient and injury variables. Patient variables include age, occupation, hand dominance, comorbidities and associated injuries. Injury variables include nature and timing of injury, presence of web space contracture, status of CMC joint, and most importantly, level of injury. According to Waljee J, the level of thumb injury can be classified into four levels: distal thumb (interphalangeal joint to tip), distal midthumb (middle proximal phalanx to interphalangeal joint), proximal midthumb (distal metacarpal to the middle of proximal phalanx), and proximal thumb (proximal metacarpal)[3]. Many patients can still function well when the amputation is distal to the interphalangeal joint (IPJ); however, more proximal amputations require soft tissue reconstruction to preserve length and function[4,5].
Thumb reconstruction can be performed by various methods, depending on the previously mentioned variables, such as local flaps, regional flaps and distant or free flaps. Options are described below with some clinical cases.
LOCAL FLAPS
Homodigital
Atasoy flap
This V-Y advancement flap was first described by Tranquilli-Leali, and later by Atasoy for fingertip injuries[2,6]. It is a viable option for small thumb tip defects up to 0.8 cm with exposed bone, since it provides a sensate flap with good contour and colour match. The flap is started by marking “V” shaped incision lines, keeping the tip of the “V” at the distal Inter phalangeal crease and the base of the “V” is made by the injured area of the volar thumb, and it should not be wider than the nail bed. The incision should go through the entire thickness of skin, and the fibrous septa should be gradually dissected and cut until the subcutaneous fats pop out, down to the FPL insertion distally. Next, the flap is mobilized to the defect. If the mobilization is insufficient, residual fibrous septa at the apex of the flap can be divided. The flap is first sutured at the distal edge to the nail bed, then the proximal part of the “V” is mostly closed in V to Y fashion. An inadequate release can result in a V-V flap rather than a V to Y flap. The fibrous septa could be distinguished from the small vessels by the spreading action of tenotomy scissors; the fine vessels are elastic and relatively robust on stretching. The donor site can be allowed to heal with the secondary intention to avoid unnecessary tension that could result in flap ischaemia[7].
Eponychial flap
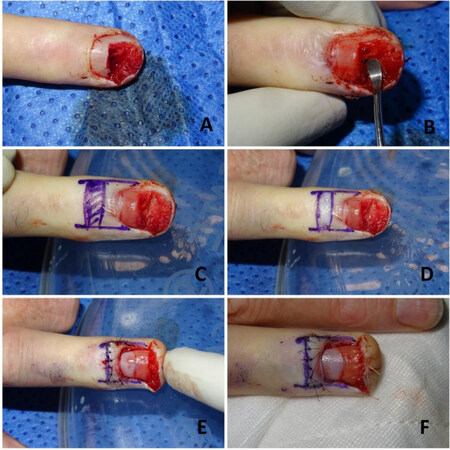
This flap was described by Bakhach[8] for improvement of nail bed appearance following fingertip injury by lengthening of the nail bed complex. The vascular supply for the flap comes from distal branches of the dorsal distal arcade. Eponychial flap is done in combination with other flaps for fingertip reconstruction[9,10]. First, the eponychium is lifted and freed from the nail bed; the nail fold is exposed. Then, the flap can be moved proximally by de-epithelizing a small rectangular area as in the original Bakhach method or by making 2 longitudinal incisions on the lateral border of the eponychial flap as in the modified method[9]. The proximal corners of the rectangular de-epithelialized area can be made roundish to have a better aesthetic appearance[11]. Finally, the flap is sutured in position proximally [Figures 1 and 2].
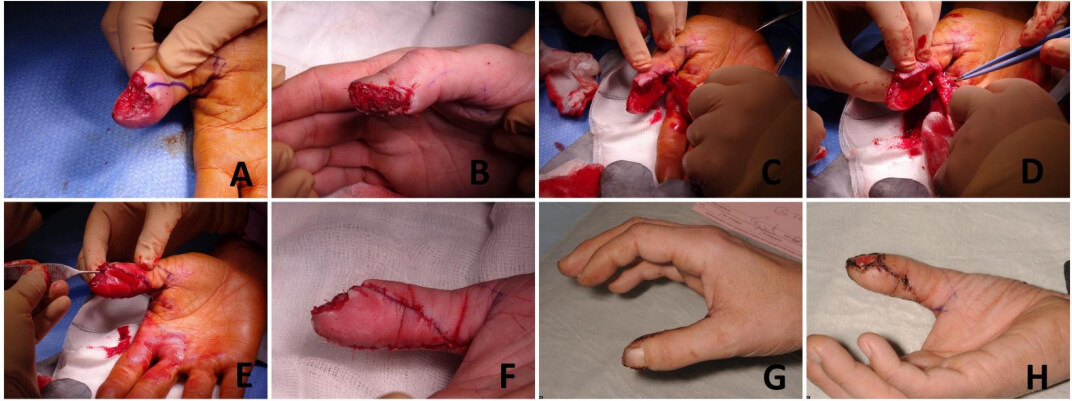
Figure 1. Eponychial flap. (A) Fingertip injury of the right thumb with loss of the distal part of the nail bed. (B) Eponychial flap created, nail bed complex lengthened and the flap sutured proximally using 5/0 vicryl rapide.
Figure 2. This figure shows a step-by-step approach to the reconstruction of a nail bed defect using eponychial flap. The defect was in the nail bed of the patient’s ring finger, not the thumb, but we included it here for illustrative purposes. (A) The nail bed defect. (B) The nail plate was removed, and the eponychium was lifted and freed from the nail bed. (C) A small rectangular area was marked to be de-epithelized. (D) The proximal rectangular area was de-epithelized. (E) The flap was sutured in position proximally. (F) The final result.
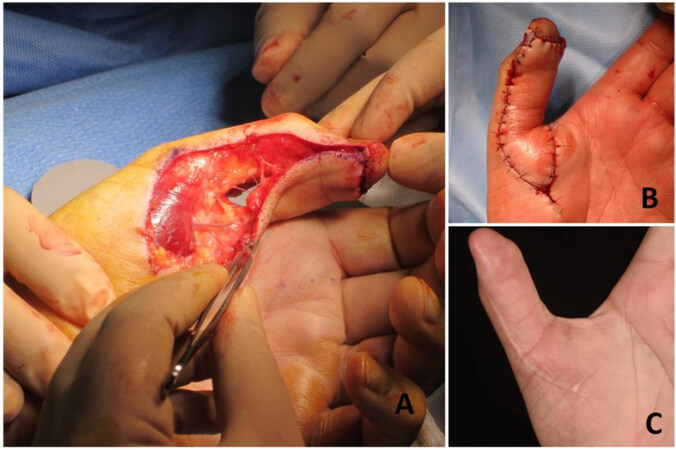
Palmar advancement/Moberg flap
This flap was first described in 1964 by Moberg for soft tissue reconstruction of the volar thumb injuries with exposed bone and tendon[12]. Moberg flap is a good choice providing sensate glabrous tissue for volar oblique defects measuring up to 2 cm over the distal third of the thumb. The vascular basis for the flap is radial and ulnar digital arteries of the thumb, present on the volar side. The shortcoming of Moberg flap is the development of a stiff thumb (IPJ contracture), as reported in the literature. To overcome this problem, the original Moberg flap was later modified with the addition of a V-Y advancement to extend the range of the flap and provide for a tension-free closure of the defect[13]. In 1968, O’Brien made a transverse incision at the flap base and used a skin graft to cover the donor site defect, leading to coverage of a larger defect by this modification. Covering the donor site defect with a graft may lead to scar contracture, hypertrophy, and color mismatch[14]. Another modification is the extended palmer flap, which can cover up to 3 cm of the defect by proposing 2 additional rotational flaps over the radial and ulnar borders of the flap [Figure 3][15,16].
Figure 3. (A) The Moberg flap was advanced as a V-Y flap, with some perforators at the base of the flap. (B) Immediate flap inset. (C) Follow-up of the patient showing a good postoperative result.
After debridement of the defect, an incision is made over the mid-axial line of the thumb bilaterally. The flap is raised just over the sheath of flexor pollicis tendon. The neurovascular bundles are carefully included in the flap. The flap is pulled distally to check the reach of the flap and dissection is done until the reach is adequate. Slight flexion (30°-45°) of the IP joint may be necessary to complete the flap reach. To improve the reach of the flap, the base of the flap can be designed in a V-Y fashion and recruit tissue from the thenar eminence, as described by David Elliott.
Brunelli flap (dorso ulnar flap) & Moschella flap (dorso radial flap)
Brunelli flap is a fasciocutaneous islanded flap demonstrated by Brunelli in 1993. It is a versatile flap for the reconstruction of small to moderate-size defects of the volar and dorsal aspects of the thumb[17]. Moschella flap is also known as the reverse first dorsal radial metacarpal flap[18].
The vascular basis for Brunelli flap is the retrograde flow through the dorsal arch of the proximal nail bed and the palmar anastomosis with the palmar digital artery to the ulnar dorsal digital artery[19]. Moschella flap is based on the recurrent radial branch of the princeps pollicis artery[20]. Both flaps can be used as fasciocutaneous with adipo-fascial extension, as well as osteocutaneous flaps[21].
In the preoperative planning of both flaps, the artery is localized by a handheld doppler along its course. The flap is designed to keep the artery in the centre. Dissection starts from proximal to distal. During elevation, the pedicle is kept surrounded by some loose adipofascial tissue. The skin between the defect and pivot point should be cut open and undermined instead of tunnelling to prevent venous congestion and help the easy transfer of the flap[22].
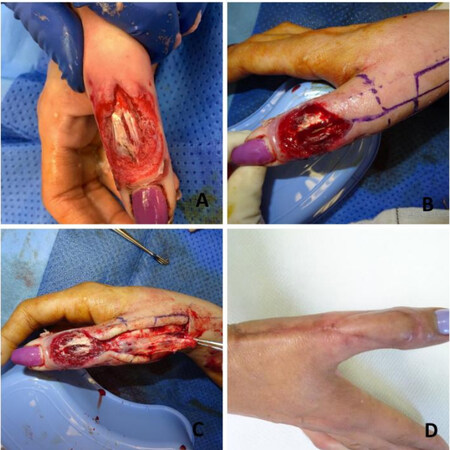
In Brunelli flap, the marking starts with drawing 2 horizontal lines, the position of the dorsal arch is 0.7 cm from the nail fold and the palmar anastomosis is 2.3 cm from the nail fold, and 2 vertical lines, the longitudinal axis of thumb and a parallel line 1 cm ulnar to this line signifying the course of the dorsal ulnar artery (DUA) of the thumb. The flap is centered over the DUA, the proximal extent is just above the head of the metacarpal, and the pedicle should be kept around 1 cm in width. The most distal extension of dissection is the interphalangeal joint; the flap is rotated and then inset. The raw area over the pedicle is closed or can be skin grafted [Figure 4 and 5][23]. Moschella flap is different from Brunelli flap in flap location and pivot point. The dorsal radial artery of the thumb arises from the radial artery in the anatomical snuffbox palmar to the EPL tendon. It courses straight distally, communicating with the palmar circulation at the level of the middle third of the proximal phalanx. This point is the pivot point for Moschella flap
Figure 4. (A) The preoperative dorsal thumb defect with the extensor pollicis tendon exposed. (B) The defect was debrided and washed out properly, and the Brunelli flap and pedicle were designed and marked. (C) The flap was raised, taking into account that the most distal extension of dissection should be proximal to the interphalangeal joint. (D) Flap was inset with a good postoperative result.
Figure 6. (A) The defect and flap design. (B) The flap harvest with the pivot point at the level of the middle third of the proximal phalanx of the thumb. (C) The flap inset.
Modification in both flaps includes adipofascial extension to decrease donor site morbidity and provide a larger flap. Shortcomings are providing an insensate flap, with some degree of joint flexion deformity that might occur. However, the incidence is much less in Moschella flap and early mobilization of the thumb can be done to avoid joint stiffness[25].
Oblique triangular flap (venkatswami flap)
Oblique triangular flap, also called the oblique triangular flap (OTF), is a type of V-Y advancement flap described by Venkatswami in 1980[26]. This flap is best suited for radial or ulnar oblique amputations. The vascular basis of the flap is the digital artery. The variant of this flap is Segmüller flap, described by Segmüller in 1976[27]. The differences between the Segmüller and Venkatswami flaps are that the distal edge of Segmüller flap is innervated while in Venkatswami flap it is not, Segmüller flap can be raised bilaterally, and the size of the flap; the proximal apex of the originally described Segmüller flap does not cross the interphalangeal joint crease.
The flap marking starts with drawing the mid-axial line on the injured side of the thumb. The base of the flap is kept equal to the width of the defect. The apex of the flap is marked between the middle of the proximal phalanx and the metacarpophalangeal joint in such a way that the length of the flap is around 2 to 2.5 times its base. An oblique line is marked on the volar side of the thumb from the apex to the base at the defect margin. The incisions are made over the 2 lines cutting the skin down to the underlying fat. The skin incision can be designed as a step ladder rather than a straight line to avoid scar contracture[28]. The flap is carefully elevated from the underlying flexor sheath, including the neurovascular pedicle in it. The flap is then advanced and sutured to the defect [Figure 7][29,30].
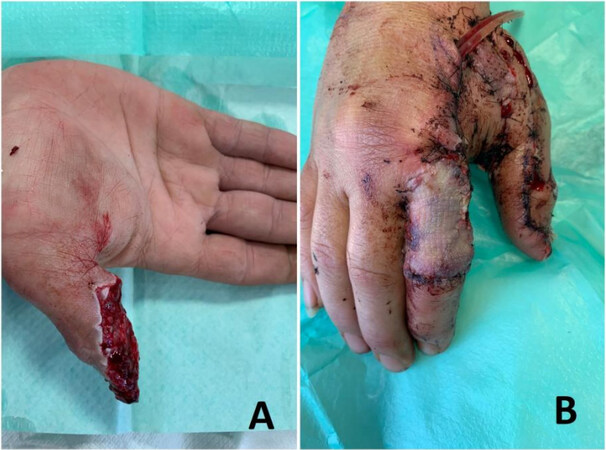
Figure 7. (A) Radial oblique amputation of the distal phalanx of the thumb. (B) Few tacking sutures were taken to reduce the size of the defect. (C) The Venkatswami flap was raised with the apex of the flap situated between the middle of the proximal phalanx and the metacarpophalangeal joint. (D) Make sure that the neurovascular pedicle was included in the flap. (E) The flap was advanced in a V-Y pattern. (F) The flap was inset and well perfused. (G and H) Good postoperative result.
Heterodigital flaps
Cross finger flap
Cross finger flap was first described by Cronin in 1945[31] and later popularized by Gurding and Pangman[32]. It is a simple, easy-to-perform, useful flap for posttraumatic volar and dorsal thumb defect coverage. This is a random pattern flap based on the subdermal plexus from branches of the digital artery. The flap marking is done over the dorsum of the proximal phalanx of the index finger as per the defect size. Markings of the flap should not cross beyond the proximal interphalangeal or the metacarpophalangeal joints. The base of the flap is kept on the radial side of the index finger; the direction of the flap can be changed according to the nature of the defect, which means that the flap can be obliquely oriented to help in better inset. The flap is raised in the plane overlying the extensor tendon paratenon from ulnar to radial. A full-thickness skin graft is placed over the donor area with a tie over the dressing. The thumb is placed in the most comfortable position and the flap is sutured into the defect. Flap division and final inset can be done after 2-3 weeks[33].
This flap is simple to perform and reliable, with good sensory recovery in young patients. Reported complications of this flap are donor site scar, stiffness of the fingers and first webspace contracture. Few modifications have been described, such as: (1) using the ring finger as a donor site[34]; (2) distally based cross finger flap[35]; and (3) jumping cross finger flap in cases of multi-digit injuries, in which soft tissue flaps from non-adjacent injured fingers may be used for coverage of small defects over the digits and thumbs instead of debridement[36].
Cross finger flap can also be raised innervated either by a dorsal sensory branch of the radial nerve only or dual innervation by cutting the dorsal branch of the index radial digital nerve and anastomosing it to the thumb ulnar digital nerve[37-40].
First dorsal metacarpal artery flap/Foucher flap
The vascular basis of FDMA flap family is the first dorsal metacarpal artery (FDMA), which is a branch of the radial artery originating in the first metacarpal web space between the head of the first dorsal interosseus muscle and extensor pollicis longus. The FDMA may present in various vascular branching patterns; however, the most common pattern is the single trunk arising from the radial artery and then dividing into branches-radial (FDMAr), intermediate (FDMAi), and ulnar (FDMAu). The FDMAr supplies the ulnar side of the thumb, FDMAi supplies the first webspace and FDMAr supplies the dorsal surface of the index finger. Venous drainage occurs by the accompanying veins.
The FDMA flap was initially described by Hilgenfelt as a pedicled fasciocutaneous flap and later modified by Holevich in 1963 as an islanded flap with a tail, an extension of skin cover over the pedicle[41]. Foucher and Braun, in 1979, reported an islanded sensate skin flap from the dorsum of the index finger based on the FDMA[42]. They have included a branch of the superficial radial nerve in the flap. Combined volar and dorsal defect reconstruction was reported by El-Khatib extended FDMA[43]. Couceiro described the bilobed racquet flap or extended seagull flap for thumb defects[44].
The radial artery and FDMA are localized on the dorsum of hand by a handheld doppler. The flap is then marked as per the required defect along with the path of the artery. The design of the flap can be different, and we will describe the 2 most commonly used methods, Holevich and Foucher. In Holevich method, the tapering skin strip is marked on both sides of the artery until the pivot point near the metacarpal shaft. Incisions are made as per the markings; the flap is elevated from ulnar to radial. The fascial attachments were dissected from the underlying muscular plane. The extensor sagittal band may be included in the flap for ease of dissection. The skin bridge is opened and undermined laterally. The flap is transferred to the defect. A full-thickness skin is used to cover the donor site. In the Foucher method, the flap is elevated similarly from the ulnar to the radial side along with the radial extensor sagittal band, and the vascular pedicle is dissected without any skin covering. The pedicle should contain aponeurosis and perivascular fat along with the artery and superficial veins. The superficial branch of radial nerve is also included in the flap. The skin bridge is undermined, and the flap is transferred to the defect. Only the flap donor site is skin grafted and the rest of the area is closed primarily[41,42,45]. Zhang et al. reported improved static 2-point discrimination of the flap by performing neurorrhaphy between the radial nerve branch of the second dorsal digital nerve which was included in the flap and the proper digital nerve of the thumb
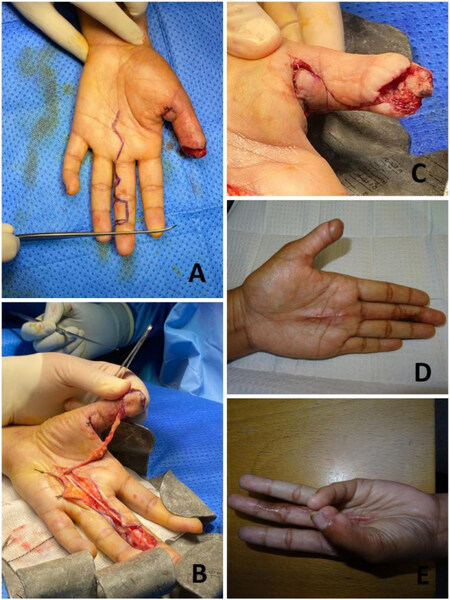
Figure 8. (A) Thumb laceration injury, dorsal defect, and bone and tendon exposure. (B) Foucher flap raised and transferred to reconstruct the dorsum of the thumb. The donor site was covered with a skin graft and a tie-over dressing.
Figure 9. (A) Volar thumb defect. (B) Reconstruction using a Foucher flap and a skin graft to the donor site.
Neurovascular island flap (Littler’s)
Littler’s neurovascular islanded flap is a heterodigital, single-stage, sensate flap[47,48]. Either a Doppler or Allen test is needed before proceeding with the flap to test the patency of both digital vessels of the finger. The flap is harvested from the ulnar aspect of the middle finger or radial aspect of the ring finger. The flap is marked, keeping the midlateral line as the axis of the flap. The most distal margin of the flap is the tip of the finger. A zigzag incision is made over the lateral aspect of the finger proximal to the flap to expose the neurovascular pedicle. The flap is elevated from distal to proximal. The Grayson and Cleland ligaments are divided during dissection. The flap is elevated below the plane of neurovascular bundle. When the dissection is reached at the bifurcation of the common digital vessels and nerve, the artery to the adjacent finger is ligated and divided, further dissection is then continued till the beginning of the common digital artery from the superficial palmer arch. The common digital nerve to the adjacent digit is dissected using intraneural dissection and then separated. Once the flap is freed and all dissection is completed, transfer of the flap to the defect is performed. This can be done by either opening the skin bridge or by tunneling the skin bridge to the defect. Hemostasis should be checked before the transfer of the flap. The flap is transferred to the defect and inset is done; the donor site is covered with a full-thickness skin graft
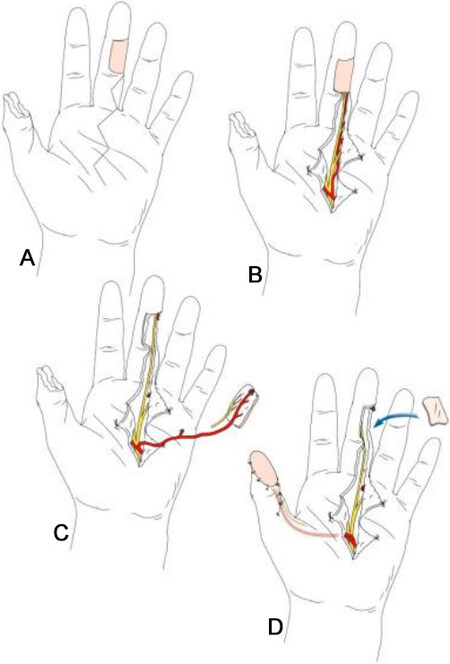
Figure 11. A diagram showing Littler’s flap harvest. (A) The thumb defect and the flap design on the ulnar aspect of the middle finger. (B) A zigzag incision is made and the neurovascular pedicle is exposed. (C) The flap is raised. (D) The flap reaches the defect under a skin tunnel, and the donor site is covered with a full-thickness skin graft.
PEDICLED AND FREE FLAPS
Pedicled groin flap
Pedicled flaps such as groin and abdominal flaps are still the mainstay of reconstruction in posttraumatic upper extremity defects at many centres.
The groin flap is an axial pattern flap described by McGregor and Jackson in 1972[51]. The vascular basis of this flap is the superficial circumflex iliac (SCI) artery. The flap marking is started with a line joining the ASIS with the pubic tubercle. The SCI artery courses 2 cm parallel to and below the inguinal ligament and divides at the medial border of sartorius muscle into a superficial and a deep branch. Beyond the ASIS, the flap becomes a random pattern flap[52].
This is a straightforward flap with reliable vascular anatomy and thin and pliable skin for hand and thumb reconstruction. Flap dimensions can reach up to 20 × 15 cm, and the donor site can be closed primarily with a flap width of 10 cm. The donor site morbidity is minimal compared to other flaps. A disadvantage of the flap is the uncomfortable period of attachment[52].
Inset of the flap in thumb reconstruction can be designed either as a tubed groin flap for circumferential defects or, in larger defects, and the flap can be inset by wrapping the end of the flap as per the defect. The flap delay is done in the second week and followed by division inset at around 21 days. In multi-finger defects, the groin flap can be fashioned as multiple small flaps called ‘daughter flaps’ instead of a single flap during flap raising to prevent syndactylisation[53]. Groin flap can also be safely raised in a suprafascial plane. These super thin flaps are better for resurfacing defects and help to avoid secondary debulking surgery[54]. In 1977, Joshi reported the use of the lateral cutaneous branches of the 12th thoracic nerve as a potential donor for neurotization of the groin flap[55].
Methods of closure of the donor site are critical in directing the flap towards the defect and reducing the strain and uncomfortable hand position[56]. Moreover, 3 parallel lines can be drawn just proximal to the wrist and monitored to ensure the correct hand positioning and prevent kinking of the flap[57].
Free venous flaps
Arterialized venous flaps (AVFs) can be an excellent option for the reconstruction of thumb defects. The main advantages of these flaps are the avoidance of scarification of a major artery of the donor site, the flap can be harvested easily without deep dissection, and can provide thin pliable tissue readily available to cover multiple skin defects if needed[58]. Recently, multiple techniques have been described to improve the AVFs outcome. Two techniques showed very successful results: (1) the retrograde pattern in which valves act as shunt restrictors, thus enhancing the flap perfusion and reducing the rate of flap failure[59]; and (2) the antegrade shunt restriction technique in which ligating clips are used to act as “simulated valves” maintaining secured separation between the venous and arterial circulations[60]. Lombardo et al. discussed how to improve the viability of AVFs by combining both techniques[61], the retrograde flow and shunt restriction, achieving more reliable isolation between the venous and arterial systems.
Free temporoparietal fascial flap
This flap can provide soft tissue reconstruction of the thumb, especially following traumatic ring avulsion injuries. It is a highly vascular flap, allowing overlying skin grafts to adhere well, thus minimizing donor site morbidity. The fact that it is a thin and pliable fascial tissue makes it advantageous in the provision of glide for an adequate range of motion as well. Excellent aesthetic and functional outcomes make it a good reconstructive option for ring avulsion injuries[62].
Great toe transfer
The transfer of a toe to replace an amputated thumb represents one of the first applications of microsurgical techniques[63]. The first great toe-to-hand transfer in a human was performed in Queen Victoria Hospital in UK by John Cobbett in 1968[64].
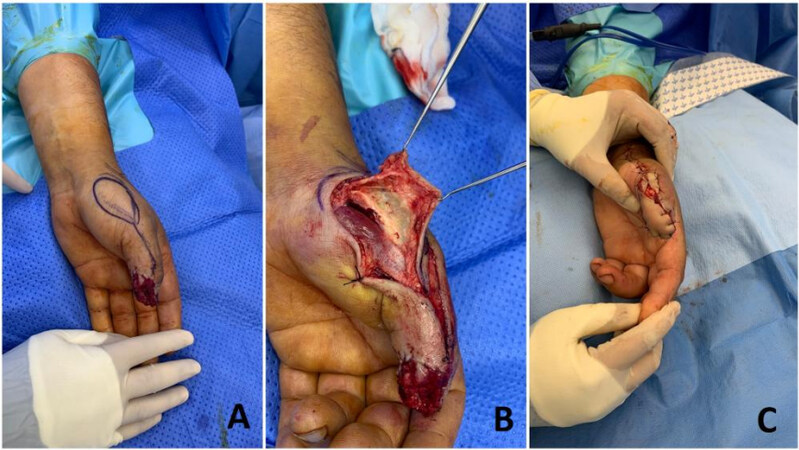
Performing a toe transfer acutely or subacutely during the initial hospital stay is safe and sometimes desirable, owing to the shortened convalescence and that the procedure itself may be technically easier due to lack of fibrosis. Large series from experienced surgeons show no difference in outcomes or complications between immediate and delayed transfers[65,66]. However, in many cases, an immediate transfer is not practical or feasible, and the initial management is only preparatory[67]. The surgical procedure, as described by Del Piñal et al., starts with an assessment of the thumb defect, debridement and bony stabilization[5]. The ipsilateral hallux is used as a donor site to permit the dominant artery and nerve to be oriented along the donor side. Dissection starts by isolating the veins. A tourniquet is used without applying an Esmarch bandage to keep some blood in the veins, which facilitates the dissection. The donor artery could be the dorsalis pedis artery, the intermetatarsal artery, or the lateral digital artery, and it is anastomosed to the ulnar digital artery at the thumb. Care should be taken to identify, dissect and ligate a constant branch proximal to the neck of the proximal phalanx. A segment of the lateral digital nerve is included with or without part of the medial digital nerve depending on the size of the toe pulp harvested. The pulp is then reflected off the distal phalanx and the bone is trimmed. Osteosynthesis is performed using 2-3 K-wires. Vascular anastomoses are carried out end-to-end using 10/0 nylon; a single artery and a vein are usually needed. The donor site is closed using a V-Y advancement flap from the medial side[5,68-70].
In 70% of cases, the dorsal metatarsal artery is dominant, and dissection is usually easier dorsally and can be continued all the way to the dorsalis pedis if necessary[71]. Plantar dissection is more difficult and, if carried beyond the mid-metatarsal level, would cause increased morbidity, and a bridging vein graft may be needed[72]. The senior author often performs the anastomosis to the radial artery at the snuff box and uses a second team to prepare the recipient vessels [Figure 13].
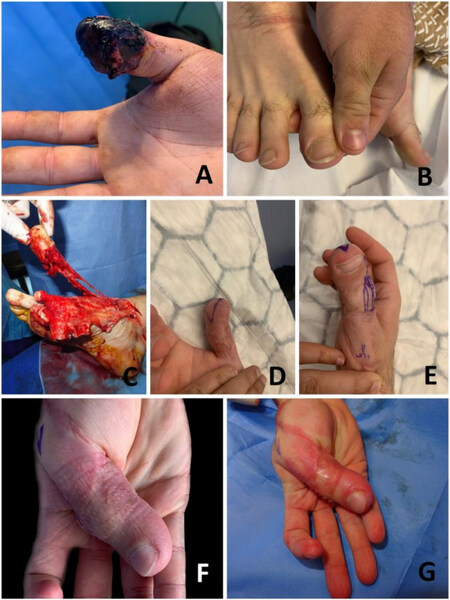
Figure 13. (A) Posttraumatic necrosis of the distal phalanx of the right thumb. (B) The ipsilateral great toe was used as an immediate great toe to hand transfer in order to salvage the thumb interphalangeal joint (IPJ) of this patient’s dominant hand. (C) Flap raise. This patient had a dorsal dominant circulation. The pedicle was harvested long enough to enable vascular anastomosis to the radial artery and venae comitantes. (D-F) A pulp plasty and a debulking procedure were performed later on in order to improve the functional and aesthetic results. (G) Immediately after the pulp plasty and debulking procedure. This patient regained IPJ movement and static 2-point discrimination S2PD of 10 mm, and returned to work.
If the great toe is significantly larger than the thumb, it can be reduced to the appropriate size in one of 2 methods. The first method is the “wrap-around” flap, in which the soft tissue of the toe is elevated off the bone and wrapped at the thumb around a conventional bone graft[73]. The other method is the timed great toe, in which only part of the skin, subcutaneous tissue and bone are harvested from the side of the toe[74].
ANCILLARY PROCEDURES
Distraction osteogenesis
Apart from reconstructive procedures, few ancillary procedures such as distraction osteogenesis can also be performed for thumb reconstruction. Patients with at least 3 cm residual stump of the first metacarpal are candidates for distraction lengthening of thumb by the use of external mini fixators. A dorsal midline approach is usually prefered because of its simplicity and visibility. A mini fixator with four self-tapping Schanz pins (1.5-2.5 mm) is a good choice for distraction. A transverse osteotomy is made in between the distal and proximal pins. Distraction is checked, and a gap of 0.5 mm is kept before closure. After a latent period of 1 week postoperatively, distraction can be started gradually at a rate of 0.5 mm/day. Consolidation of the distraction is confirmed with X-ray. An average distraction that can be achieved with this technique is 25-37 mm[75]. While this is a safe procedure with the added advantage of sensate and simultaneous soft tissue lengthening, the major disadvantages of this method include long time, pin tract infection, non-union, and need for bone grafting[76].
Web space deepening
Web space deepening is another procedure that can be an option for cases with limitations of thumb abduction after traumatic injuries. This surgery creates an apparent gain in length and increases the span of hand. Z-plasty, skin grafting, and local flaps can be used along with postoperative splinting for optimal outcomes[77].
Pollicisation
Pollicization in posttraumatic cases is useful when the level of amputation is at the carpometacarpal joint or proximal to it. In literature, the index finger is the most commonly used for pollicisation in posttraumatic thumb defects. However, pollicisation using the middle and ring fingers was also reported. Although pollicisation can be done in the acute posttraumatic period, we prefer it as an elective procedure to optimize the outcome. Our preferred approach is the dorsal “v” shaped incision for the index finger and the curvilinear incision for the other fingers. Careful neurovascular dissection is required to get the adequate gain in length needed for transfer. Extensor and flexor tendons are carefully preserved. The donor site stump is prepared, then the transferred digit is placed in such a way that its pulp faces towards the little finger. Two oblique k wires can be used for the bony fixation. Pollicisation in posttraumatic cases provides a safe and effective way of thumb reconstruction, especially when microvascular facilities are not available[78].
CONCLUSION
There are different ways to reconstruct a deficient thumb, so patients must be informed about the various options in order to be able to make an informed decision about the best reconstructive procedure personally and professionally. Additionally, the patient must be a good candidate medically, socially and psychologically and commit to the reconstructive process.
Multiple factors should be considered when deciding on the reconstructive procedure. Patient factors include age, hand dominance, comorbidities, occupation, smoking status, culture, and compliance to participate in postoperative rehabilitation. Cultural differences, on some occasions, can affect the reconstructive plan. For example, Japanese patients generally focus on the length and salvage of the nail plate. Indian patients usually have difficulty wearing traditional shoes and may be reluctant to accept a great toe transfer.
The main goals in thumb reconstruction are the restoration of functional length, stability, mobility, sensation and aesthetic appearance. If the reconstructive surgeon can achieve all these goals, the functional outcome and patient satisfaction will be great. However, if all can not be achieved, then at least a stable thumb with adequate length will be restored, allowing for some grip and pinch activities.
DECLARATIONS
AcknowledgmentsThe authors would like to thank Julia Ruston, specialty registrar of plastic surgery Royal Free Hospital, for the nice illustration in Figure 10.
Authors’ contributionsMade substantial contributions to conception and design of the study: Yassin AM, Nikkhah D
Performed data acquisition, as well as provided administrative, technical, and material support: Yassin AM, Dash S, Nikkhah D
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Authors 2022.
REFERENCES
1. Dewey WS, Richard RL, Hedman TL, et al. Opposition splint for partial thumb amputation: a case study measuring disability before and after splint use. J Hand Ther 2009;22:79-86; quiz 87.
2. Atasoy E, Ioakimidis E, Kasdan ML, Kutz JE, Kleinert HE. Reconstruction of the amputated finger tip with a triangular volar flap. A new surgical procedure. J Bone Joint Surg Am 1970;52:921-6.
3. Waljee J. Thumb reconstruction. In: Brown DL, Borschel GH, editors. Michigan Manual of Plastic Surgery. Philadelphia: Lippincott Williams & Wilkins; 2014. Available from: https://books.google.com.hk/books?hl=zh-CN&lr=&id=PyuZASnw2xoC&oi=fnd&pg=PR11&dq=Waljee+J.+Thumb+reconstruction.+In:+David+L.+Brown+GHB,+Benjamin+Levi,+ed.+Michigan+Manual+of+Plastic+Surgery.+Philadelphia,+PA+19103+USA+LIPPINCOTT+WILLIAMS+%26+WILKINS%3B+2014.&ots=rnp7lXySIk&sig=tK_k3wfb5zeEIF4Bzpeaxfh0bkg&redir_esc=y#v=onepage&q&f=false [Last accessed on 13 Sep 2022].
4. Lister G. The choice of procedure following thumb amputation. Clin Orthop Relat Res 1985;195:45-51.
5. Piñal F, Moraleda E, de Piero GH, Ruas JS, Galindo C. Onycho-osteo-cutaneous defects of the thumb reconstructed by partial hallux transfer. J Hand Surg Am 2014;39:29-36.
6. Gharb BB, Rampazzo A, Armijo BS, et al. Tranquilli-Leali or Atasoy flap: an anatomical cadaveric study. J Plast Reconstr Aesthet Surg 2010;63:681-5.
7. Nikkhah D, Singh M, Teo TC. Avoiding the V-V flap when performing an atasoy V-Y flap. J Hand Surg Am 2014;39:2122-3.
9. Bakhach J, Demiri E, Guimberteau JC. Use of the eponychial flap to restore the length of a short nail: a review of 30 cases. Plast Reconstr Surg 2005;116:478-83.
10. Chen HY, Hsu CC, Lin YT, Yeh JT, Lin CH, Lin CH. Functional and aesthetic outcomes of the fingertips after nail lengthening using the eponychial flap. J Plast Reconstr Aesthet Surg 2015;68:1438-46.
11. Merlino G, Carlucci S. A simple modification of the Bakhach’s eponychial flap for nail lengthening after fingertip amputation. J Plast Reconstr Aesthet Surg 2011;64:e265-6.
12. Moberg E. Aspects of sensation in reconstructive surgery of the upper extremity. J Bone Joint Surg Am 1964;46:817-25.
13. Elliot D, Wilson Y. V-Y advancement of the entire volar soft tissue of the thumb in distal reconstruction. J Hand Surg 1993;18:399-402.
14. O’brien B. Neurovascular island pedicle flaps for terminal amputations and digital scars. Br J Plast Surg 1968;21:258-61.
16. Foucher G, Delaere O, Citron N, Molderez A. Long-term outcome of neurovascular palmar advancement flaps for distal thumb injuries. Br J Plast Surg 1999;52:64-8.
18. Moschella F, Cordova A, Pirrello R, Brunelli F. Anatomic basis for the dorsal radial flap of the thumb: clinical applications. Surg Radiol Anat 1996;18:179-81.
19. Brunelli F, Vigasio A, Valenti P, Brunelli GR. Arterial anatomy and clinical application of the dorsoulnar flap of the thumb. J Hand Surg Am 1999;24:803-11.
20. Yang D, Morris SF. Vascular basis of dorsal digital and metacarpal skin flaps. J Hand Surg Am 2001;26:142-6.
22. Hrabowski M, Kloeters O, Germann G. Reverse homodigital dorsoradial flap for thumb soft tissue reconstruction: surgical technique. J Hand Surg Am 2010;35:659-62.
23. Terán P, Carnero S, Miranda R, Trillo E, Estefanía M. Refinements in dorsoulnar flap of the thumb: 15 cases. J Hand Surg Am 2010;35:1356-9.
24. Moschella F, Cordova A. Reverse homodigital dorsal radial flap of the thumb. Plast Reconstr Surg 2006;117:920-6.
25. Bao QY, Xiao CW, Peng F, Han D, Wang T, Gu YD. Restoration of thumb sensibility with innervated reverse homodigital dorsoradial flap. J Reconstr Microsurg 2014;30:15-20.
26. Venkataswami R, Subramanian N. Oblique triangular flap: a new method of repair for oblique amputations of the fingertip and thumb. Plast Reconstr Surg 1980;66:296-300.
28. Evans D, Martin D. Step-advancement island flap for fingertip reconstruction. Br J Plast Surg 1988;41:105-11.
29. Elliot D, Yii NW. Homodigital reconstruction of the digits - the perspective of one unit. Handchir Mikrochir Plast Chir 2001;33:7-19.
30. Usami S, Kawahara S, Yamaguchi Y, Hirase T. Homodigital artery flap reconstruction for fingertip amputation: a comparative study of the oblique triangular neurovascular advancement flap and the reverse digital artery island flap. J Hand Surg Eur Vol 2015;40:291-7.
32. Gurdin M, Pangman WJ. The repair of surface defects of fingers by trans - digital flaps. Plast Reconstr Surg (1946) 1950;5:368-71.
33. Woon CY, Lee JY, Teoh LC. Resurfacing hemipulp losses of the thumb: the cross finger flap revisited: indications, technical refinements, outcomes, and long-term neurosensory recovery. Ann Plast Surg 2008;61:385-91.
34. Chitta M, Malathi L, Joseph A. Cross-finger flap to the thumb: quest for an alternate donor. Indian J Plast Surg 2020;53:287-92.
35. Patil RK, Chavre S. Distally based cross-finger flaps for amputation stumps in avulsion amputations. Indian J Plast Surg 2012;45:504-11.
36. Sabapathy SR, Mohan D, Bharathi RR. “Jumping” cross finger flaps: a useful technique for salvaging parts in mutilating hand injuries. Br J Plast Surg 2000;53:488-90.
37. Miura T. Thumb reconstruction using radial-innervated cross-finger pedicle graft. J Bone Joint Surg Am 1973;55:563-569.
38. Gaul JS Jr. Radial-innervated cross-finger flap from index to provide sensory pulp to injured thumb. J Bone Joint Surg Am 1969;51:1257-63.
39. Walker MA, Hurley CB, May JW. Radial nerve cross-finger flap differential nerve contribution in thumb reconstruction. J Hand Surg 1986;11:881-7.
40. Cohen BE, Cronin ED. An innervated cross-finger flap for fingertip reconstruction. Plast Reconstr Surg 1983;72:688-97.
41. Holevich J. A new method of restoring sensibility to the thumb. J Bone Joint Surg Br 1963;45:496-502.
42. Foucher G, Braun JB. A new island flap transfer from the dorsum of the index to the thumb. Plast Reconstr Surg 1979;63:344-9.
43. El-khatib HA. Clinical experiences with the extended first dorsal metacarpal artery island flap for thumb reconstruction. J Hand Surg 1998;23:647-52.
44. Couceiro J, De la Red-Gallego M, Yeste L, et al. The bilobed racquet flap or extended seagull flap for thumb reconstruction: a case report. J Hand Surg Asian Pac Vol 2018;23:128-31.
45. Couceiro J, Sanmartín M. The Holevich flap revisited: a comparison with the Foucher flap, case series. Hand Surg 2014;19:469-74.
46. Zhang X, Shao X, Ren C, Zhang Z, Wen S, Sun J. Reconstruction of thumb pulp defects using a modified kite flap. J Hand Surg Am 2011;36:1597-603.
47. LITTLER JW. The neurovascular pedicle method of digital transposition for reconstruction of the thumb. Plast Reconstr Surg (1946) 1953;12:303-19.
49. Paterson P, Titley O, Nancarrow J. Donor finger morbidity in cross-finger flaps. Injury 2000;31:215-8.
50. Rose EH. Local arterialized island flap coverage of difficult hand defects preserving donor digit sensibility. Plast Reconstr Surg 1983;72:848-58.
52. Daniel RK, Taylor GI. Distant transfer of an island flap by microvascular anastomoses. A clinical technique. Plast Reconstr Surg 1973;52:111-7.
53. Rasheed T, Hill C, Riaz M. Innovations in flap design: modified groin flap for closure of multiple finger defects. Burns 2000;26:186-9.
54. Abdelrahman M, Zelken J, Huang RW, et al. Suprafascial dissection of the pedicled groin flap: a safe and practical approach to flap harvest. Microsurgery 2018;38:458-65.
56. Bajantri B, Latheef L, Sabapathy SR. Tips to orient pedicled groin flap for hand defects. Tech Hand Up Extrem Surg 2013;17:68-71.
57. Venkatramani H, Sabapathy SR. A useful technique to maintain the position of the hand following abdominal flap cover. Indian J Plast Surg 2008;41:98-9.
58. Takeuchi M, Sakurai H, Sasaki K, Nozaki M. Treatment of finger avulsion injuries with innervated arterialized venous flaps. Plast Reconstr Surg 2000;106:881-5.
59. Moshammer HE, Schwarzl FX, Haas FM, et al. Retrograde arterialized venous flap: an experimental study. Microsurgery 2003;23:130-4.
60. Lam WL, Lin WN, Bell D, Higgins JP, Lin YT, Wei FC. The physiology, microcirculation and clinical application of the shunt-restricted arterialized venous flaps for the reconstruction of digital defects. J Hand Surg Eur Vol 2013;38:352-65.
61. Lombardo GAG, Tamburino S, Tarico MS, Perrotta RE. Reverse flow shunt restricted arterialized venous free flap. J Hand Surg Am 2018;43:492.e1-5.
62. Cullen S, Joyce K, Theopold C. Temporoparietal fascial flap for primary reconstruction of complex ring avulsion injury: a case report. JPRAS Open 2022;33:47-51.
63. Buncke HJ, Buncke CM, Schulz WP. Immediate Nicoladoni procedure in the rhesus monkey, or hallux-to-hand transplantation, utilising microminiature vascular anastomoses. Br J Plast Surg 1966;19:332-7.
64. Cobbett JR. Free digital transfer. Report of a case of transfer of a great toe to replace an amputated thumb. J Bone Joint Surg Br 1969;51:677-9.
65. Yim KK, Wei FC, Lin CH. A comparison between primary and secondary toe-to-hand transplantation. Plast Reconstr Surg 2004;114:107-12.
66. Woo SH, Kim JS, Seul JH. Immediate toe-to-hand transfer in acute hand injuries: overall results, compared with results for elective cases. Plast Reconstr Surg 2004;113:882-92.
68. Piñal F. The indications for toe transfer after “minor” finger injuries. J Hand Surg Br 2004;29:120-9.
70. Piñal F, Pennazzato D, Urrutia E. Primary thumb reconstruction in a mutilated hand. Hand Clin 2016;32:519-31.
71. Spanio S, Wei FC, Coskunfirat OK, Lin CH, Lin YT. Symmetry of vascular pedicle anatomy in the first web space of the foot related to toe harvest: clinical observations in 85 simultaneous bilateral second-toe transfer patients. Plast Reconstr Surg 2005;115:1325-7.
72. Wei FC, Silverman RT, Hsu WM. Retrograde dissection of the vascular pedicle in toe harvest. Plast Reconstr Surg 1995;96:1211-4.
73. Morrison WA, O'brien BM, Macleod AM. Thumb reconstruction with a free neurovascular wrap-around flap from the big toe. J Hand Surg 1980;5:575-83.
74. Wei FC, Chen HC, Chuang DC, Jeng SF, Lin CH. Aesthetic refinements in toe-to-hand transfer surgery. Plast Reconstr Surg 1996;98:485-90.
75. Kömürcü M, Kürklü M, Demiralp B, Atesalp AS, Alsancak S, Basbozkurt M. First ray reconstruction with distraction osteogenesis. Prosthet Orthot Int 2008;32:50-6.
76. Saleem A, Sharma RK, Kumar P. Distraction lengthening of first metacarpal in traumatic thumb amputations. Indian J Plast Surg 2019;52:309-13.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Yassin AM, Dash S, Nikkhah D. Workhorse flaps for thumb reconstruction. Plast Aesthet Res 2022;9:56. http://dx.doi.org/10.20517/2347-9264.2022.36
AMA Style
Yassin AM, Dash S, Nikkhah D. Workhorse flaps for thumb reconstruction. Plastic and Aesthetic Research. 2022; 9: 56. http://dx.doi.org/10.20517/2347-9264.2022.36
Chicago/Turabian Style
Yassin, Ahmed M., Suvashis Dash, Dariush Nikkhah. 2022. "Workhorse flaps for thumb reconstruction" Plastic and Aesthetic Research. 9: 56. http://dx.doi.org/10.20517/2347-9264.2022.36
ACS Style
Yassin, AM.; Dash S.; Nikkhah D. Workhorse flaps for thumb reconstruction. Plast. Aesthet. Res. 2022, 9, 56. http://dx.doi.org/10.20517/2347-9264.2022.36
About This Article
Copyright
Data & Comments
Data
 Cite This Article 13 clicks
Cite This Article 13 clicks















Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.