Supraclavicular lymph node transplant: a focus on technique
Abstract
Physiologic surgical options, including vascularized lymph node transplant and lymphovenous bypass are becoming increasingly popular interventions for the treatment of lymphedema of both the upper and lower extremities. Many different lymph node donor sites have been described, including submental, lateral thoracic, superficial groin, supraclavicular, and various intraabdominal sites. This paper describes a step-by-step approach to the harvest of vascularized lymph nodes from the supraclavicular area, which is the preferred donor site for most patients with both upper and lower extremity lymphedema.
Keywords
INTRODUCTION
Lymphedema, characterized by the progressive buildup of protein-rich extracellular interstitial fluid due to insufficient lymphatic drainage, is a chronic condition that can affect both the upper and lower extremities. This can lead to limb swelling, inflammation, and ultimately fibrosis, causing significant morbidity with associated pain, discomfort, limb heaviness, cellulitis, and decreased quality of life. Lymphedema can be classified as either primary or secondary, depending on whether an intrinsic problem with the lymphatic system and lymph nodes exists, or if once normal lymphatic vessels and nodes have been subsequently damaged or disrupted. In the developed world, this is most often due to oncologic treatments (lymphadenectomy and/or radiation in the groin or axilla) or trauma.
Nonsurgical management of lymphedema remains the first-line treatment option for both upper and lower extremity primary and secondary lymphedema. This can include manual drainage techniques, compression garment and pneumatic pump use, skin care optimization, exercise therapy, and patient education. Complete decongestive therapy uses a combination of all the above modalities, often requiring lifelong effort and extensive daily commitment for patients to maintain results and prevent disease progression.
Surgical interventions are becoming an increasingly popular option for patients, especially those who fail or have suboptimal results from nonsurgical management. Patients may undergo ablative surgery, including liposuction and direct excision. While ablative surgeries are effective in decreasing the volume of the affected limb by removing edematous tissue, they do not correct the underlying problem: damaged or absent lymphatic channels. Nevertheless, these damaged lymphatic channels and drainage systems can be augmented through physiologic surgery. These physiologic surgical interventions include vascularized lymph node transplant (VLNT) and lymphovenous bypass (LVB), performed either separately or in combination[1,2].
Vascularized lymph node transplant involves the transfer of vascularized lymph nodes from a donor site to a site either proximally or distally on the affected extremity. Lymph node donor sites include the supraclavicular region (SC), the submental region, the superficial groin, the lateral thoracic/axillary region, and various intraabdominal sites, such as the omentum. Each of these donor sites has its own benefits and risks, which have been widely reported[3,4]. To date, there has not been any conclusive evidence about which donor site is optimal, and much of the decision-making involves surgeon and patient preference, as well as donor site availability and clinical assessment of the lymphedematous limb[5-7]. While the exact mechanism of action of VLNT remains to be elucidated, there have been several proposed theories regarding the physiology behind how these transplanted lymph nodes function to improve lymphedema by promoting local lymphangiogenesis and acting to create spontaneous lympholymphatic anastomoses at the affected site, by acting like a “pump” through the removal and redirection of excess lymphatic fluid to the venous system, or (more likely) a combination of the two[8-10].
The aim of this paper is to describe our technique for the harvest of vascularized lymph nodes from the supraclavicular area, which is our preferred donor lymph node harvest site. As our senior author has previously published[11], the successful harvest of supraclavicular lymph nodes requires a thorough understanding of the local anatomy and the critical structures near the operative field, including the carotid artery, the internal jugular vein, and the phrenic nerve. We will also briefly discuss our experience and results from the use of this donor site.
ANATOMY
The supraclavicular lymph nodes are reliably located within an anatomic triangle whose borders are comprised of the dorsal edge of the sternocleidomastoid muscle (SCM) medially, the external jugular vein (EJV) laterally and the medial part of the clavicle inferiorly. The SC lymph nodes can be harvested with or without a skin paddle, depending on soft tissue needs at the recipient site. When harvested with a skin paddle, the blood supply comes from the supraclavicular artery, which arises from the transverse cervical artery (TCA). Venous drainage is through accompanying veins, which drain either into the transverse cervical vein (TCV) or the external jugular vein. Without a skin paddle, the blood supply to the flap can be more variable. Several cadaveric studies have examined the anatomy of the SC lymph node flap in more detail. The average pedicle length of the transverse cervical artery is between 3-5 cm, with an arterial caliber of between 1.5-3 mm, depending on the site of harvest[12,13]. Additionally, Gerety et al. examined ten cadaveric specimens and found 1-8 lymph nodes within the flap (2.6 +/- 1.6 grossly and 3.0 +/- 2.2 microscopically)[13].
TECHNIQUE
The supraclavicular lymph nodes are harvested with the patient in a supine position and the head tilted approximately 45 degrees away from the side of the harvest. This positioning can often allow for simultaneous harvest of the SC lymph nodes and preparation of the recipient site. Preoperatively, the anatomical landmarks of the EJV, the SCM, and the clavicle are marked. If the lymph nodes are to be harvested without a skin paddle, a 5-7 cm longitudinal incision is designed in the patient’s native skin crease, approximately 2 cm above the superior border of the clavicle within the aforementioned triangle [Figure 1]. If a skin paddle is to be harvested, the same positioning applies; care should be taken to Doppler and mark the perforator to the skin paddle, and then design an ellipse with this point in the center.
Figure 1. The anatomical landmarks of the EJV, the SCM, and the clavicle are marked. A 5-7 cm longitudinal incision is designed in the patient’s native skin crease, approximately 2 cm above the superior border of the clavicle within the aforementioned triangle. EJV: External jugular vein; SCM: sternocleidomastoid muscle[11].
The operation begins with a skin incision, either along the longitudinal incision (no skin paddle) or along the superior border of the designed ellipse (skin paddle). The first layer encountered is the platysma, which is divided sharply. Deep into the platysma, the supraclavicular nerves may be encountered and may need to be divided to allow for deeper dissection. Dissection proceeds posteriorly. Deep into the platysma, the omohyoid muscle or tendon is seen and subsequently divided. Once divided, a soft tissue mass consisting of fat and lymph nodes can be seen posteriorly.
We first begin with the medial dissection of the supraclavicular lymph nodes by identifying a clear plane along the lateral border of the SCM. As dissection proceeds, the internal jugular vein (IJV) is encountered, and the mass of soft tissue and lymph nodes is gently dissected off this structure. Dissection proceeds posteriorly until the anterior scalene muscle is encountered. This serves as the posteriormost border of the flap dissection. We then gently retract the IJV and identify the TCA arising from the thyrocervical trunk [Figure 2]. It is important to note that there can be significant variation in terms of the size and location of the TCA - additional dissection towards its origin and ligation of other branches may be required to obtain an artery with sufficient caliber and pedicle length. There is often an accompanying vein with the TCA - a second vein can also be harvested from the EJV for additional venous drainage. In some cases, the vascular pedicle is identified laterally, and then the flap is raised off the scalene from lateral to medial towards the origin of the pedicle. Additionally, when the vein is very small, an arterial anastomosis can be done first to help identify the best choice for venous drainage.
Figure 2. Gently retract the Internal Jugular Vein, and identify the Transverse Cervical Artery arising from the thyrocervical trunk[11].
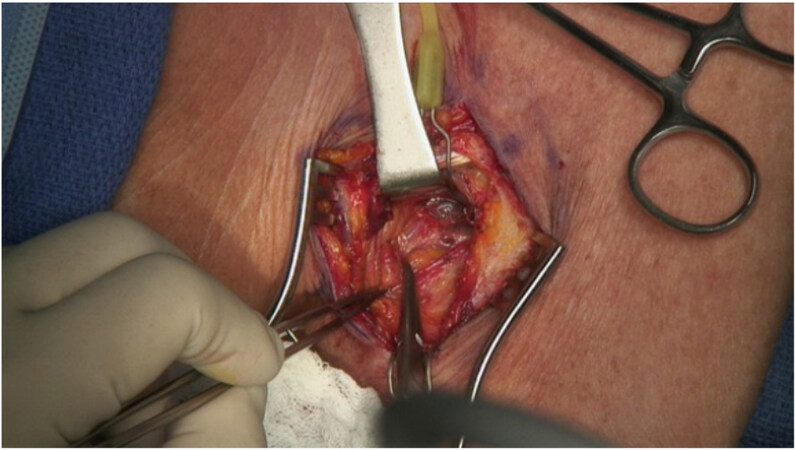
Lateral dissection begins at the previously mentioned lateral border of the triangle, the EJV. Dissection proceeds posteriorly until the anterior scalene is reached. During this portion of the dissection, the distal ends of the transverse cervical vessels are encountered and ligated. Additional length of the distal ends of the TCA and TCV can also be preserved and used for micro anastomosis if needed. During this portion of the dissection, small lymphatic vessels are often encountered. These are carefully clipped (on the patient side) to prevent any subsequent lymph leaks. The lymphatic vessels on the flap side are left unclipped [Figure 3].
Figure 3. Lymphatic vessels are carefully clipped (on the patient side) to prevent any subsequent lymph leaks. The lymphatic vessels on the flap side are left unclipped[11].
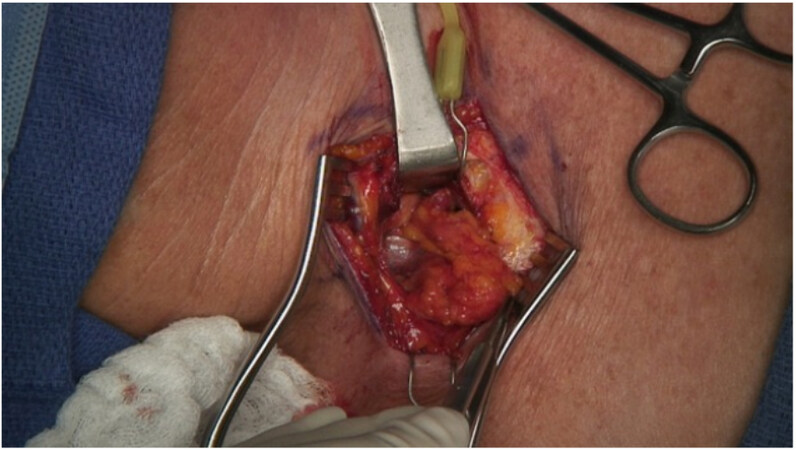
At this point, both the medial and lateral dissection of the lymph nodes has been completed, and the vascular pedicle has been identified. Posterior dissection then proceeds as the lymph node soft tissue mass is dissected off the anterior scalene muscle. During this step of the procedure, care must be taken to identify and preserve the phrenic nerve, which is often encountered in the operative field. At this point, the SC lymph node flap should be isolated on its pedicle and ready for ligation and division [Figure 4].
Figure 4. The Supraclavicular lymph node transplant should be isolated on its pedicle and ready for ligation and division[11].
Once the flap has been transferred to its recipient site location, the donor site can be closed. Adequate hemostasis is obtained, although with the above technique, the field should be relatively bloodless. A single, closed-suction drain is placed, exiting the skin laterally and ensuring that there is no suction near the IJV. The wound is closed in layers - the platysma with interrupted absorbable sutures and the skin with a running subcuticular suture. Because we routinely harvest the SC lymph nodes without a skin paddle, an implantable Doppler around the arterial anastomosis is typically used for flap monitoring for 72 h[14].
DISCUSSION
While first described by the senior author in 2013 for use in the treatment of lower extremity lymphedema[15], the supraclavicular lymph node flap has become our common choice donor site for both upper and lower extremity lymphedema in patients who have minimal soft tissue deficits at the recipient site. The benefits of this donor site are many, including no risk for facial nerve damage (as is the case with submental lymph node harvest), an easily concealed scar, and a relatively quick harvest with the use of proper technique and knowledge of anatomy. Our group has prospectively examined the aesthetic outcomes-related SC VLNT donor site scarring. The results show that the SC VLNT scar, while visible, is well-accepted by both patients and surgeons alike, with almost 77% of patients stating that they were “very satisfied” with the appearance of their scar (unpublished data).
The risks of SC VLNT harvest include bleeding, as the operative space can be small and deep, chyle leaks, and potential damage to the phrenic nerve and other important structures in the operative field. While not a downside, it is again important to reiterate that the vascular anatomy of the supraclavicular lymph nodes can be variable; therefore, it is important to pay close attention during dissection to prevent inadvertent damage to the flap’s vascularity.
A terrible complication of VLNT is the occurrence of donor site lymphedema. Although a previous case report has documented the occurrence of upper extremity lymphedema following SC VLNT harvest[16], we have not found this to be the case in our patient population. In a previous study looking at a group of 100 consecutively treated patients who underwent SC VLNT to either the upper or lower extremity by our senior author, no instances of donor site lymphedema were reported[17]. The importance of a thorough understanding of the anatomy of this region in avoiding iatrogenic lymphedema cannot be overstated.
Another potential complication of the harvest of SC lymph nodes is a resulting chyle leak from damage to surrounding lymphatics. To reduce this risk, we preferentially harvest supraclavicular lymph nodes from the right (unless the patient has had prior surgery to the right neck or has a history of right upper extremity lymphedema) to avoid damage to the thoracic duct. If a chyle leak does occur, this can often be managed expectantly with the initiation of a low-fat diet. Rarely, for high volume leaks, additional measures, including surgical intervention, need to be taken[18].
There is no current consensus on the optimal VLNT donor site when it comes to surgical outcomes in the treatment of lymphedema. However, results from our group show that patients who underwent SC VLNT had both objective and subjective improvements in their lymphedema. In a recently published study examining the impact of physiologic surgery on both upper and lower extremity secondary lymphedema, a total of 78 patients underwent supraclavicular VLNT, either alone or in combination with LVB. We did not find any significant difference in outcomes (both quantitative and qualitative measures) between these patients and those who underwent VLNT from either the lateral thoracic or groin donor sites[19].
CONCLUSION
With its favorable risk-benefit profile and relative ease of harvest, we have come to rely on the supraclavicular lymph node flap as our first-line choice for VLNT, especially in patients who do not require significant soft tissue resurfacing or who are not undergoing simultaneous autologous breast reconstruction. Given the important anatomic structures within the harvest area, it is important to have a thorough understanding of the anatomy of the region.
DECLARATIONS
Authors’ contributionsMade substantial contributions to conception and design of the study and performed data analysis, data acquisition and interpretation, as well as provided administrative, technical, and material support: Beederman M, Chang DW
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestBoth authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationWritten informed consent for publication of patient images was obtained.
Copyright© The Author(s) 2022.
REFERENCES
1. Garza R 3rd, Skoracki R, Hock K, Povoski SP. A comprehensive overview on the surgical management of secondary lymphedema of the upper and lower extremities related to prior oncologic therapies. BMC Cancer 2017;17:468.
2. Suami H, Chang DW. Overview of surgical treatments for breast cancer-related lymphedema. Plast Reconstr Surg 2010;126:1853-63.
3. Schaverien MV, Badash I, Patel KM, Selber JC, Cheng MH. Vascularized lymph node transfer for lymphedema. Semin Plast Surg 2018;32:28-35.
4. Chang EI, Chu CK, Hanson SE, Selber JC, Hanasono MM, Schaverien MV. Comprehensive overview of available donor sites for vascularized lymph node transfer. Plast Reconstr Surg Glob Open 2020;8:e2675.
5. Ciudad P, Agko M, Perez Coca JJ, et al. Comparison of long-term clinical outcomes among different vascularized lymph node transfers: 6-year experience of a single center's approach to the treatment of lymphedema. J Surg Oncol 2017;116:671-82.
6. Scaglioni MF, Arvanitakis M, Chen YC, Giovanoli P, Chia-Shen Yang J, Chang EI. Comprehensive review of vascularized lymph node transfers for lymphedema: outcomes and complications. Microsurgery 2018;38:222-9.
7. Ciudad P, Manrique OJ, Date S, et al. A head-to-head comparison among donor site morbidity after vascularized lymph node transfer: pearls and pitfalls of a 6-year single center experience. J Surg Oncol 2017;115:37-42.
8. Cheng MH, Chen SC, Henry SL, Tan BK, Chia-Yu Lin M, Huang JJ. Vascularized groin lymph node flap transfer for postmastectomy upper limb lymphedema: flap anatomy, recipient sites, and outcomes. Plast Reconstr Surg 2013;131:1286-98.
9. Cheng MH, Huang JJ, Wu CW, et al. The mechanism of vascularized lymph node transfer for lymphedema: natural lymphaticovenous drainage. Plast Reconstr Surg 2014;133:192e-8e.
10. Tourani SS, Taylor GI, Ashton MW. Vascularized lymph node transfer: a review of the current evidence. Plast Reconstr Surg 2016;137:985-93.
11. Ooi AS, Chang DW. Five-step harvest of supraclavicular lymph nodes as vascularized free tissue transfer for treatment of lymphedema. J Surg Oncol 2017;115:63-7.
12. Steinbacher J, Tinhofer IE, Meng S, et al. The surgical anatomy of the supraclavicular lymph node flap: a basis for the free vascularized lymph node transfer. J Surg Oncol 2017;115:60-2.
13. Gerety PA, Pannucci CJ, Basta MN, et al. Lymph node content of supraclavicular and thoracodorsal-based axillary flaps for vascularized lymph node transfer. J Vasc Surg Venous Lymphat Disord 2016;4:80-7.
14. Teven CM, Ooi ASH, Inbal A, Chang DW. Implantable Doppler monitoring of buried free flaps during vascularized lymph node transfer. J Surg Oncol 2017;116:371-7.
15. Althubaiti GA, Crosby MA, Chang DW. Vascularized supraclavicular lymph node transfer for lower extremity lymphedema treatment. Plast Reconstr Surg 2013;131:133e-5e.
16. Lee M, McClure E, Reinertsen E, Granzow JW. Lymphedema of the upper extremity following supraclavicular lymph node harvest. Plast Reconstr Surg 2015;135:1079e-82e.
17. Maldonado AA, Chen R, Chang DW. The use of supraclavicular free flap with vascularized lymph node transfer for treatment of lymphedema: a prospective study of 100 consecutive cases. J Surg Oncol 2017;115:68-71.
18. Teven CM, Hunter CL, Chang DW. Management of high-output chyle leak after harvesting of vascularized supraclavicular lymph nodes. Plast Reconstr Surg 2019;143:1251-6.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Beederman M, Chang DW. Supraclavicular lymph node transplant: a focus on technique. Plast Aesthet Res 2022;9:54. http://dx.doi.org/10.20517/2347-9264.2022.64
AMA Style
Beederman M, Chang DW. Supraclavicular lymph node transplant: a focus on technique. Plastic and Aesthetic Research. 2022; 9: 54. http://dx.doi.org/10.20517/2347-9264.2022.64
Chicago/Turabian Style
Beederman, Maureen, David W. Chang. 2022. "Supraclavicular lymph node transplant: a focus on technique" Plastic and Aesthetic Research. 9: 54. http://dx.doi.org/10.20517/2347-9264.2022.64
ACS Style
Beederman, M.; Chang DW. Supraclavicular lymph node transplant: a focus on technique. Plast. Aesthet. Res. 2022, 9, 54. http://dx.doi.org/10.20517/2347-9264.2022.64
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 4 clicks
Cite This Article 4 clicks













Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.