Regenerative peripheral nerve interfaces (RPNIs): current status and future direction
Abstract
Despite significant advancements in neuroprosthetic control strategies, current peripheral nerve interfacing techniques are limited in their ability to facilitate accurate and reliable long-term control. The regenerative peripheral nerve interface (RPNI) is a biologically stable bioamplifier of efferent motor action potentials with demonstrated long-term stability. This innovative, straightforward, and reproducible surgical technique has shown enormous potential in improving prosthetic control for individuals with upper limb amputations. The RPNI consists of an autologous free muscle graft secured around the end of a transected peripheral nerve or individual fascicles within a residual limb. This construct facilitates EMG signal transduction from the residual peripheral nerve to a neuroprosthetic device using indwelling bipolar electrodes on the muscle surface. This review article focuses on the development of the RPNI and its use for intuitive and enhanced prosthetic control and sensory feedback. In addition, this article also highlights the use of RPNIs for the prevention and treatment of postamputation pain.
Keywords
INTRODUCTION
Upper limb loss has devastating functional consequences as well as a substantial impact on an individual’s self-perception and quality of life[1]. Recent innovations in robotic technology have led to the development of upper extremity prosthetic devices that are capable of emulating precise finger, hand, and wrist movements[2]. However, persons with upper extremity amputations continue to reject these advanced devices at high rates, preferring conventional (i.e., body-powered or myoelectric) prosthetic limbs that provide little functional recovery[3]. This finding is largely due to a lack of an intuitive, functional neural interface that can provide high-fidelity control signals for efferent motor control. The majority of current experimental peripheral nerve interfaces are limited by several disadvantages, including iatrogenic nerve injury from electrode insertion, insufficient signal selectivity and reproducibility, substantial signal degradation over time, and an inability to prevent neuroma formation[4,5].
To overcome the limitations of current neural interfacing strategies, our laboratory has developed the regenerative peripheral nerve interface (RPNI) to provide reliable, high-fidelity signal transduction from the residual limb for optimal prosthetic activation and volitional control[6-11]. The RPNI is composed of a transected peripheral nerve, or peripheral nerve fascicle, that is implanted into a free skeletal muscle graft[12] [Figure 1]. After the free muscle graft is secured around the terminal end of the fascicle or nerve, the graft undergoes a process of regeneration, revascularization, and reinnervation by the implanted peripheral nerve[13]. This process creates a biologically stable peripheral nerve bioamplifier that produces high-amplitude EMG signals[6-8,13]. An epimysial electrode is then implanted in the RPNI to record specific efferent motor action potentials[13], which serves as an interface that can be utilized for prosthetic control[6-8,13,14]. This surgical approach has numerous benefits, including decreased neuroma formation, improved signal-to-noise ratio (SNR) by means of neuromuscular signal amplification, as well as avoidance of iatrogenic axonal injury that occurs with direct neural interfacing approaches[14]. Furthermore, because RPNIs can be created with individual fascicles, specific and selective prosthetic device control supporting multiple degrees of freedom is possible, potentially resulting in a more intuitive and enhanced experience when compared to other neuroprosthetic control techniques[15]. In addition to neuroprosthetic control, RPNIs may have the potential for providing sensory feedback from the prosthetic to the sensory afferents in patients with upper extremity amputations[16]. Lastly, RPNI surgery is indicated for effective prevention and treatment of neuromas and postamputation pain[17]. The purpose of this article is to review the multiple applications of the RPNI.
REGENERATIVE PERIPHERAL NERVE INTERFACE DEVELOPMENT
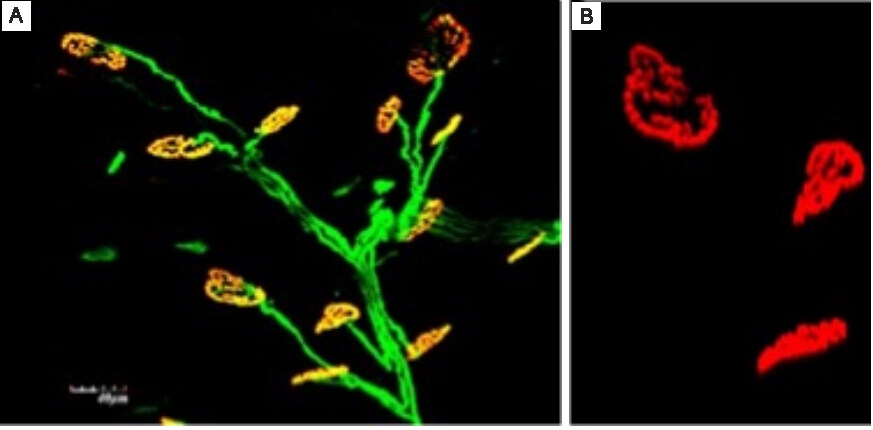
Development of the RPNI began with extensive preliminary testing of RPNIs in animal models[6-8,11,13,18]. Initial testing in rodents utilized free skeletal muscle grafts of the extensor digitorum longus (EDL) muscle neurotized by the divided common peroneal nerve for the creation of RPNIs[13]. Following the three-month regeneration, revascularization, and reinnervation process, RPNIs were shown to generate high-amplitude compound muscle action potentials (CMAPs) that could be readily recorded[13]. Further experimentation confirmed the biologic stability of the interface and provided histologic evidence of axonal regeneration and synaptogenesis within the construct[11] [Figure 2].
Figure 2. Histologic evidence of axonal regeneration and synaptogenesis within the RPNI. (A) Reinnervating axons stained green using anti-neurofilament 200. (B) Neuromuscular junctions stained red using fluorescent alpha-bungarotoxin conjugates. RPNI: Regenerative peripheral nerve interface.
Subsequent testing revealed reliable RPNI signal transduction in real-time during voluntary muscle activation[8,11]. These experiments showed that RPNI EMG activity could be selectively recorded without electrical interference and signal contamination from adjacent active muscles or RPNIs[8,11]. In addition, results from these experiments revealed that RPNIs had high SNR when compared to a control group without RPNIs[11]. Substantiated by these findings, this rodent model was used to further investigate the long-term stability of RPNIs along with their ability to transduce efferent motor action potentials into CMAPs[18]. Signals were measured up to 14 months postoperatively and demonstrated large-amplitude CMAPs without evidence of RPNI degeneration or signal degradation over time[18]. Together, these findings demonstrated that the RPNI is a reliable and stable peripheral nerve interface that facilitates signal transduction of efferent motor action potentials into large-amplitude CMAPs, with high SNRs and minimal signal contamination, over long periods of time.
Initial rodent RPNI experiments provided the foundation for studies in nonhuman primates using rhesus macaques who were trained to perform specific cued finger movements[6]. RPNIs were created in these monkeys using the median, ulnar, and radial nerves[6]. RPNI EMG signals were recorded for finger flexion, finger extension, and finger rest with an accuracy of over 96%[6]. Long-term stability was demonstrated with efferent motor action potentials transduced into large-amplitude CMAPs with high SNRs up to 20 months postoperatively in this model[6]. Building on this work, subsequent experiments on rhesus macaques were performed to control continuous and real-time finger flexion and finger extension of a prosthetic hand using indwelling bipolar electrodes[7]. Due to the positive results from these animal studies, clinical translation and subsequent testing of RPNIs were next carried out in humans.
REGENERATIVE PERIPHERAL NERVE INTERFACE FOR NEUROPROSTHETIC CONTROL
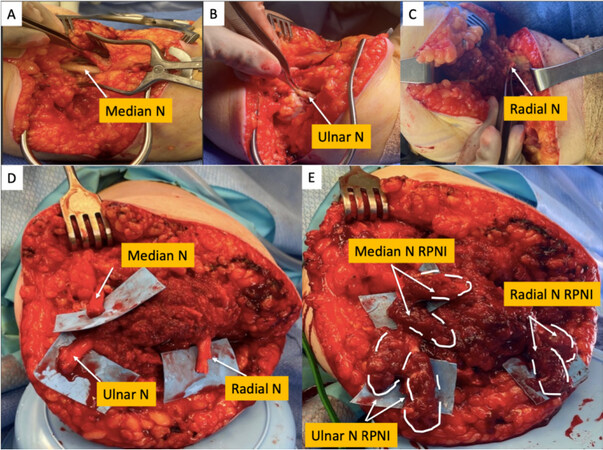
A pilot study in humans with upper extremity amputations demonstrated the successful use of RPNIs for real-time, volitional prosthetic device control[9]. The study included four participants with varying levels of amputation including transradial, wrist disarticulation, and shoulder disarticulation. RPNIs in these patients were created using transected residual nerves (including the median nerve, ulnar nerve, and radial nerve) and muscle grafts harvested from the patient’s vastus lateralis [Figure 3]. Participant 1 (P1) elected to have temporary fine wire electrodes placed in their RPNIs under ultrasound guidance. However, in this participant, RPNI EMG signals recorded immediately after electrode insertion had a mean SNR of 4.21[9]. In contrast, participants 3 (P3) and 4 (P4) elected to have indwelling bipolar electrodes surgically implanted in their RPNIs. The SNR of the recorded signals in these participants were significantly larger with a mean of 68.9 and 21.0, respectively, and were effective in providing high-fidelity control of thumb and finger flexion and extension, as well as intrinsic finger control (finger abduction and adduction)[9]. This difference is likely attributed to the bipolar electrode design and the relatively small space between electrode sites in the percutaneous fine wires (1 mm) compared to the indwelling electrodes (10 mm)[9]. Of note, the future direction of RPNIs includes electrode implantation at the time of RPNI surgery, as opposed to using percutaneous wire electrodes into existing RPNIs.
Figure 3. Intraoperative RPNI creation. This patient underwent implantation of four RPNIs, one each for the radial and median nerve and two for the ulnar nerve. RPNI: Regenerative peripheral nerve interface.
In these patients, RPNIs demonstrated effective transduction of efferent motor action potentials into large amplitude CMAPs, with high SNRs, for high-fidelity prosthetic control of both extrinsic and intrinsic hand and finger movements[9]. The patients who underwent surgical implantation of indwelling bipolar EMG electrodes into their RPNIs had substantially higher SNRs for prosthetic control, especially when compared to other methods of harnessing signals directly from peripheral nerves such as cuff and intraneural electrodes[9]. In addition, RPNIs did not cause iatrogenic nerve injury, nor were there any problems with signal stability or degradation commonly seen with electrodes that directly interface with peripheral nerves[9].
This human study also showed the functional stability of RPNIs through ultrasound imaging. For example, independent contractions of distinct RPNIs, in the same patient with multiple median nerve RPNIs, could be seen on ultrasound during thumb flexion, index finger flexion of the proximal interphalangeal (PIP) joint, and index finger flexion of the distal interphalangeal (DIP) joint. On ultrasound, subsections of the same RPNI and alternative RPNIs of the median nerve fascicles contracted based on the patient’s varying motor intent. This finding shows that an RPNI contains individual motor units that contract independently, thus allowing for the accurate recording of discrete signals. Importantly, electrodes can be spaced millimeters apart on the large surface area of the RPNI to enable selective and functional prosthetic control, as theoretically, electrodes with more recording sites within RPNIs can provide enhanced signal selectivity[9]. The use of indwelling bipolar electrodes in RPNIs overcomes a major barrier inherent to peripheral nerve interfaces that use intraneural electrodes which require micrometer spacing of numerous recording sites[9,15]. Another distinct advantage of RPNIs over other techniques is that RPNIs do not rely on recording EMG signals from residual innervated muscles because signals can be recorded directly from peripheral nerves through the RPNI[15]. In fact, even in patients with proximal amputations, fascicular RPNIs can be created and utilized to capture signals for intrinsic finger movements. For instance, distinct RPNIs that facilitated individual finger movements were identified in a patient with a shoulder-level amputation[9].
Human trials have also demonstrated that patients with RPNIs have long-term stability of RPNI signals for highly accurate, continuous control of prosthetic finger movements[9]. Experimental tasks were designed to test the accuracy of prosthetic control. These tasks were completed by patients with high accuracy on day 0 (96%-100%) up to day 300 (96%-100%)[9]. It should be noted that signal amplitudes and SNR remained unchanged over time without the need for recalibration of the original control algorithm. This is a significant advancement and major benefit due to the fact that other existing strategies of prosthetic control require frequent recalibrations for accurate, reliable control[19-23]. For example, powered prostheses controlled using surface EMG often require daily recalibrations, and even multiple recalibrations during the same day, due to changes in electrode impedance, position, and motion artifacts throughout the day. Even as the user becomes more experienced using the device, the need for frequent recalibration cannot be eliminated[19]. The outcomes from clinical trials in humans have helped establish the reliability, stability, and durability of RPNIs in signal transduction for intuitive neuroprosthetic control.
REGENERATIVE PERIPHERAL NERVE INTERFACES FOR SENSORY FEEDBACK
Despite the advancements in modern robotic technology, prosthetic users still primarily rely on visual feedback to improve the function and control of their prosthetic device[24]. Lack of sensory feedback is a major limitation to reestablishing the full functionality of the natural limb. Restoring tactile sensation and proprioception would relieve the cognitive burden of relying solely on visual cues to monitor motor commands. In addition, the restoration of the sense of touch would provide tremendous psychological benefits and give individuals a sense of prosthetic embodiment[25].
As a solution to these challenges, RPNIs have been used to provide sensory afferent signals for sensory feedback from prosthetic devices[10,16,26]. Findings from a study on participants with upper limb amputations revealed the ability of RPNIs to restore sensation[16]. In this study, patients underwent the creation of RPNIs on their median and ulnar nerves as well as implantation of indwelling bipolar electrodes in the RPNIs and intact forearm muscles. After one month, patients participated in monthly experimental stimulation sessions. Electrical stimulation of the RPNIs resulted in both meaningful and anatomically appropriate proprioceptive and cutaneous sensations in the residual limb[16]. These initial results are promising and encourage further investigation into the potential of this interface to provide sensory feedback. The addition of sensory feedback with efferent motor control would establish a robust bidirectional closed-loop prosthetic paradigm that could significantly improve the quality of life for individuals with amputations and would fully capture the potential of extremity prostheses[25,27].
PREVENTION AND TREATMENT OF NEUROMAS AND POSTAMPUTATION PAIN
Debilitating chronic pain is common after limb amputation. An estimated fifty to eighty percent of patients with limb loss suffer from residual limb pain (RLP) and phantom limb pain (PLP)[28,29]. These conditions are associated with significant functional consequences, such as prosthetic abandonment and inadequate prosthetic rehabilitation, as well as impairments in activities of daily living and decreased quality of life[29-32]. It has been well established in the literature that successful treatment of symptomatic neuromas in this patient population has the potential to alleviate both RLP and PLP[33-35].
Symptomatic terminal neuromas develop when the transected axons of an injured nerve fail to reestablish connections with their end organs, which are no longer present following amputation. Exuberant regeneration of these axons occurs, forming disorganized, hyperexcitable, painful masses of Schwann cells, axonal sprouts, blood vessels, and connective tissue[36,37]. Although multiple surgical interventions have been proposed for symptomatic neuroma treatment, such as traction neurectomy, these conventional methods have yielded unsatisfactory results including failed pain resolution and neuroma recurrence[38-40].
The RPNI has been found to be an uncomplicated and effective solution for both the treatment and prevention of symptomatic neuromas[17,33,41]. In contrast to other existing methods of neuroma treatment, the RPNI addresses the regenerating nerve’s physiologic inclination for end organ reinnervation. In this construct, the free autologous muscle graft undergoes revascularization and is reinnervated by regenerating axons, forming new neuromuscular junctions. This leads to fewer axons without functional connections, thereby decreasing the erratic axons that contribute to the formation of a painful neuroma[13,17]. Current studies investigating whether or not neuromas form within the RPNI construct using ultrasound have not shown neuroma formation within RPNIs.
Studies from our research group have shown that the utilization of RPNIs can successfully treat existing symptomatic neuromas and phantom limb pain[33,42], in addition to preventing the formation of neuromas when prophylactically performed at the time of amputation[43]. A retrospective study compared postamputation pain outcomes between patients who underwent prophylactic RPNI surgery at the time of amputation to age, gender, and level of amputation-matched control patients whose peripheral nerves were instead treated with either traction neurectomy, suture ligature, burial of peripheral nerve within the nearby muscle, or a combination of these strategies[43]. RPNI patients experienced a significantly decreased incidence of symptomatic neuromas (0% vs. 13.3%) and phantom limb pain (51.5% vs. 91.1%) after a mean follow-up time of approximately one-year[43]. Additionally, RPNI patients experienced an overall lower rate of postoperative complications compared to the control group (31.1% vs. 55.6%), demonstrating that the addition of RPNI surgery performed at the time of primary amputation does not increase surgical morbidity[43]. Further research is needed to investigate the possibility of neuroma formation within the RPNI construct.
The RPNI has demonstrated enormous potential to decrease the incidence of postamputation pain. Given the results of our study, all patients who undergo limb amputation should be considered for RPNI surgery for prophylactic prevention of postamputation neuromas. This will undoubtedly have positive implications for pain outcomes, rehabilitation, and overall quality of life for this patient population.
CONCLUSION
In summary, the RPNI is a neuroprosthetic control strategy that transduces signals from residual peripheral nerves with high accuracy and favorable SNRs for enhanced prosthetic device control and user experience. The indications for RPNIs continue to expand as this technique can be applied to any transected peripheral nerve to provide denervated target end organs for reinnervation. The RPNI is a safe, straightforward, and reproducible surgical technique. This novel interface for prosthetic motor control has also shown promise in restoring sensory feedback in persons with upper extremity amputations. Furthermore, RPNIs can be used to treat and prevent neuroma formation and postamputation pain. RPNIs have revolutionized the potential of neuroprosthetic control of the upper extremity, creating an enhanced, intuitive experience for prosthetic users.
DECLARATIONS
Authors’ contributionsPerformed writing of the manuscript: Burke KL
Assisted with manuscript preparation: Kung TA, Hooper RC, Kemp SWP, Cederna PS
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2022.
REFERENCES
1. Armstrong TW, Williamson MLC, Elliott TR, Jackson WT, Kearns NT, Ryan T. Psychological distress among persons with upper extremity limb loss. Br J Health Psychol 2019;24:746-63.
2. Trent L, Intintoli M, Prigge P, et al. A narrative review: current upper limb prosthetic options and design. Disabil Rehabil Assist Technol 2020;15:604-13.
3. Cowley J, Resnik L, Wilken J, Smurr Walters L, Gates D. Movement quality of conventional prostheses and the DEKA Arm during everyday tasks. Prosthet Orthot Int 2017;41:33-40.
4. Schultz AE, Kuiken TA. Neural interfaces for control of upper limb prostheses: the state of the art and future possibilities. PM R 2011;3:55-67.
5. Kung TA, Bueno RA, Alkhalefah GK, Langhals NB, Urbanchek MG, Cederna PS. Innovations in prosthetic interfaces for the upper extremity. Plast Reconstr Surg 2013;132:1515-23.
6. Irwin ZT, Schroeder KE, Vu PP, et al. Chronic recording of hand prosthesis control signals via a regenerative peripheral nerve interface in a rhesus macaque. J Neural Eng 2016;13:046007.
7. Vu PP, Irwin ZT, Bullard AJ, et al. Closed-loop continuous hand control via chronic recording of regenerative peripheral nerve interfaces. IEEE Trans Neural Syst Rehabil Eng 2018;26:515-26.
8. Ursu DC, Urbanchek MG, Nedic A, Cederna PS, Gillespie RB. In vivo characterization of regenerative peripheral nerve interface function. J Neural Eng 2016;13:026012.
9. Vu PP, Vaskov AK, Irwin ZT, et al. A regenerative peripheral nerve interface allows real-time control of an artificial hand in upper limb amputees. Sci Transl Med 2020;12:eaay2857.
10. Svientek SR, Ursu DC, Cederna PS, Kemp SWP. Fabrication of the composite regenerative peripheral nerve interface (C-RPNI) in the adult rat. J Vis Exp 2020; doi: 10.3791/60841.
11. Frost CM, Ursu DC, Flattery SM, et al. Regenerative peripheral nerve interfaces for real-time, proportional control of a Neuroprosthetic hand. J Neuroeng Rehabil 2018;15:108.
12. Urbanchek MG, Kung TA, Frost CM, et al. Development of a regenerative peripheral nerve interface for control of a neuroprosthetic limb. Biomed Res Int 2016;2016:5726730.
13. Kung TA, Langhals NB, Martin DC, Johnson PJ, Cederna PS, Urbanchek MG. Regenerative peripheral nerve interface viability and signal transduction with an implanted electrode. Plast Reconstr Surg 2014;133:1380-94.
14. Woo SL, Urbanchek MG, Cederna PS, Langhals NB. Revisiting nonvascularized partial muscle grafts: a novel use for prosthetic control. Plast Reconstr Surg 2014;134:344e-6e.
15. Kumar N, Kung TA, Cederna PS. Regenerative peripheral nerve interfaces for advanced control of upper extremity prosthetic devices. Hand Clin 2021;37:425-33.
16. Vu PP, Lu CW, Vaskov AK, et al. Restoration of proprioceptive and cutaneous sensation using regenerative peripheral nerve interfaces (RPNIs) in humans with upper-limb amputations. Plast Reconstr Surg 2022;149:1149e-1154e.
17. Kubiak CA, Adidharma W, Kung TA, Kemp SWP, Cederna PS, Vemuri C. “Decreasing postamputation pain with the regenerative peripheral nerve interface (RPNI)”. Ann Vasc Surg 2022;79:421-6.
18. Langhals NB, Woo SL, Moon JD, et al. Electrically stimulated signals from a long-term regenerative peripheral nerve interface. Annu Int Conf IEEE Eng Med Biol Soc 2014;2014:1989-92.
19. Scheme E, Englehart K. Electromyogram pattern recognition for control of powered upper-limb prostheses: state of the art and challenges for clinical use. J Rehabil Res Dev 2011;48:643-59.
20. Fluit R, Prinsen EC, Wang S, van der Kooij H. A comparison of control strategies in commercial and research knee prostheses. IEEE Trans Biomed Eng 2020;67:277-90.
21. Iturrate I, Chavarriaga R, Millán JDR. General principles of machine learning for brain-computer interfacing. Handb Clin Neurol 2020;168:311-28.
22. Antelis JM, Montesano L, Ramos-Murguialday A, Birbaumer N, Minguez J. On the usage of linear regression models to reconstruct limb kinematics from low frequency EEG signals. PLoS One 2013;8:e61976.
23. Chavarriaga R, Millan Jdel R. Learning from EEG error-related potentials in noninvasive brain-computer interfaces. IEEE Trans Neural Syst Rehabil Eng 2010;18:381-8.
24. Childress DS. Historical aspects of powered limb prostheses. Clinical Prosthetics & Orthotics 1985;9:2-13. Available from: http://www.oandplibrary.org/cpo/1985_01_002.asp [Last accessed on 11 Aug 2022]
25. Tan DW, Schiefer MA, Keith MW, Anderson JR, Tyler J, Tyler DJ. A neural interface provides long-term stable natural touch perception. Sci Transl Med 2014;6:257ra138.
26. Nghiem BT, Sando IC, Gillespie RB, et al. Providing a sense of touch to prosthetic hands. Plast Reconstr Surg 2015;135:1652-63.
27. Davis TS, Wark HA, Hutchinson DT, et al. Restoring motor control and sensory feedback in people with upper extremity amputations using arrays of 96 microelectrodes implanted in the median and ulnar nerves. J Neural Eng 2016;13:036001.
28. Hanley MA, Ehde DM, Jensen M, Czerniecki J, Smith DG, Robinson LR. Chronic pain associated with upper-limb loss. Am J Phys Med Rehabil 2009;88:742-51; quiz 752, 779.
29. Sinha R, van den Heuvel WJ, Arokiasamy P. Factors affecting quality of life in lower limb amputees. Prosthet Orthot Int 2011;35:90-6.
30. Kooijman CM, Dijkstra PU, Geertzen JH, Elzinga A, van der Schans CP. Phantom pain and phantom sensations in upper limb amputees: an epidemiological study. Pain 2000;87:33-41.
31. Singh RK, Prasad G. Long-term mortality after lower-limb amputation. Prosthet Orthot Int 2016;40:545-51.
32. Morgan SJ, Friedly JL, Amtmann D, Salem R, Hafner BJ. Cross-sectional assessment of factors related to pain intensity and pain interference in lower limb prosthesis users. Arch Phys Med Rehabil 2017;98:105-13.
33. Woo SL, Kung TA, Brown DL, Leonard JA, Kelly BM, Cederna PS. Regenerative peripheral nerve interfaces for the treatment of postamputation neuroma pain: a pilot study. Plast Reconstr Surg Glob Open 2016;4:e1038.
34. Prantl L, Schreml S, Heine N, Eisenmann-Klein M, Angele P. Surgical treatment of chronic phantom limb sensation and limb pain after lower limb amputation. Plast Reconstr Surg 2006;118:1562-72.
35. Economides JM, DeFazio MV, Attinger CE, Barbour JR. Prevention of painful neuroma and phantom limb pain after transfemoral amputations through concomitant nerve coaptation and collagen nerve wrapping. Neurosurgery 2016;79:508-13.
36. Cravioto H, Battista A. Clinical and ultrastructural study of painful neuroma. Neurosurgery 1981;8:181-90.
37. Ives GC, Kung TA, Nghiem BT, et al. Current state of the surgical treatment of terminal neuromas. Neurosurgery 2018;83:354-64.
38. Eberlin KR, Ducic I. Surgical algorithm for neuroma management: a changing treatment paradigm. Plast Reconstr Surg Glob Open 2018;6:e1952.
39. Mackinnon SE. Evaluation and treatment of the painful neuroma. Tech Hand Up Extrem Surg 1997;1:195-212.
40. Santosa KB, Oliver JD, Cederna PS, Kung TA. Regenerative peripheral nerve interfaces for prevention and management of neuromas. Clin Plast Surg 2020;47:311-21.
41. Kubiak CA, Kemp SWP, Cederna PS. Regenerative peripheral nerve interface for management of postamputation neuroma. JAMA Surg 2018;153:681-2.
42. Hooper RC, Cederna PS, Brown DL, et al. Regenerative peripheral nerve interfaces for the management of symptomatic hand and digital neuromas. Plast Reconstr Surg Glob Open 2020;8:e2792.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Burke KL, Kung TA, Hooper RC, Kemp SWP, Cederna PS. Regenerative peripheral nerve interfaces (RPNIs): current status and future direction. Plast Aesthet Res 2022;9:48. http://dx.doi.org/10.20517/2347-9264.2022.26
AMA Style
Burke KL, Kung TA, Hooper RC, Kemp SWP, Cederna PS. Regenerative peripheral nerve interfaces (RPNIs): current status and future direction. Plastic and Aesthetic Research. 2022; 9(8): 48. http://dx.doi.org/10.20517/2347-9264.2022.26
Chicago/Turabian Style
Burke, Katherine L., Theodore A. Kung, Rachel C. Hooper, Stephen W. P. Kemp, Paul S. Cederna. 2022. "Regenerative peripheral nerve interfaces (RPNIs): current status and future direction" Plastic and Aesthetic Research. 9, no.8: 48. http://dx.doi.org/10.20517/2347-9264.2022.26
ACS Style
Burke, KL.; Kung TA.; Hooper RC.; Kemp SWP.; Cederna PS. Regenerative peripheral nerve interfaces (RPNIs): current status and future direction. Plast. Aesthet. Res. 2022, 9, 48. http://dx.doi.org/10.20517/2347-9264.2022.26
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 11 clicks
Cite This Article 11 clicks












Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.