Nerve decompression in diabetics with chronic nerve compression: update 2022
Abstract
The number of people with diabetes worldwide has reached epidemic proportions. Diabetics are well-known to have chronic nerve compressions, and the prevalence of compressions exceeds 50% in those with neuropathy. The loss of sensation in the feet of people with diabetic neuropathy is the primary cause of their ulceration and amputation, as well as pain. The aim of this article is to update the reader on the current status of lower extremity nerve decompression in patients with diabetic neuropathy. A review of the history and literature related to the current approach to the patient with chronic nerve compression plus diabetic neuropathy was undertaken. The current evidence is overwhelmingly clear, in diabetics with neuropathy and a positive Tinel sign over the tibial nerve at the tarsal tunnel, that decompression, by neurolysis of lower extremity nerves, can relieve pain, restore sensation, and prevent ulceration and amputation. Furthermore, economic cost-benefit analysis by the Markov technique demonstrates that lower extremity nerve compression is not only cost-effective compared to standard medical care, but also increases the quality of life and life expectancy. The remaining barriers to acceptance and implementation of this proven surgical approach must lie in the education of physicians in training and re-education of diabetes educators, primary care providers and endocrinologists.
Keywords
INTRODUCTION
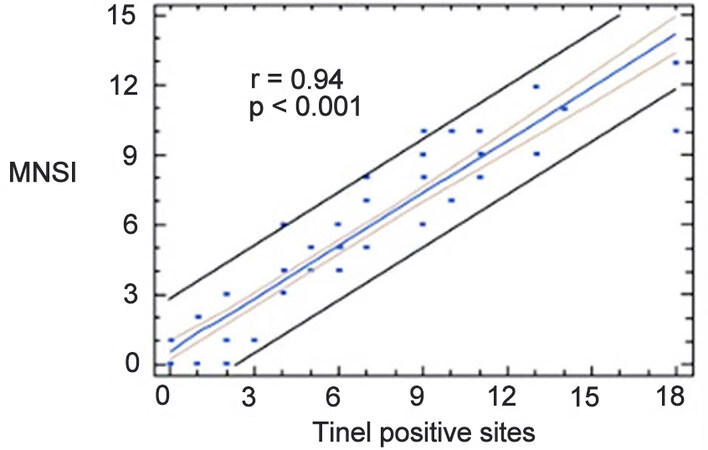
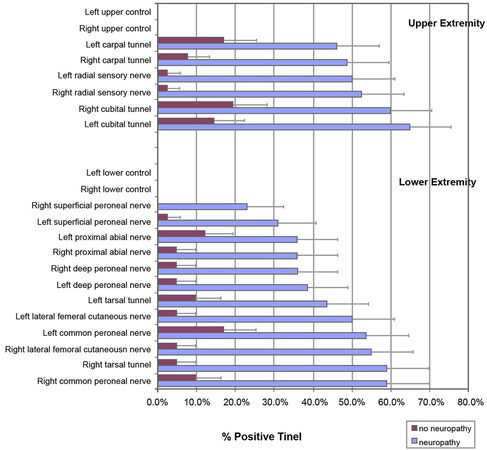
Since about 50% of people with diabetes develop neuropathy[1,2], the worldwide explosion of diabetes[3] means that there will be an explosion of patients with diabetic neuropathy. About 50% of patients with diabetic neuropathy have multiple chronic lower extremity nerve compressions [Figures 1 and 2][4,5]. In 1982, I began doing decompression of lower extremity nerves in diabetics and the results of this work were reported in 1992[6], demonstrating that 80% of patients with a positive Tinel sign of the tibial nerve in the tarsal tunnel had improved sensation, and decreased pain. Subsequent studies demonstrated that there was significantly less (P < 0.001) ulceration and amputation for a patient that had nerve decompression than the “control” that did not have that surgery[7]. In 2012, a multicenter prospective study of 38 surgeons, including 800 patients with a 3-year follow-up, demonstrated that 80% of patients had a significant (P < 0.001) relief of pain by six months after surgery, sensation recovered in the feet, 0.3% vs. the expected 15% of patients developed ulceration, 0.2% vs. the expected 15% had an amputation, and 0.6% vs. the expected 3.7% had a hospitalization for foot infection[8].
Figure 1. Relationship between severity of neuropathy, determined by the Michigan neuropathy screening instrument and the number of Tinel signs in a population of diabetics. The worse the neuropathy clinically, the more sites of compression in the given patient, with a correlation coefficient of 0.94 and a value of significance of P < 0.001[4].
Figure 2. Relationship in the upper and the lower extremity between the number of nerve compressions in diabetics with and without neuropathy for a given site of nerve entrapment[4].
There have been four independent basic science studies that demonstrate that rats with streptozotocin-induced diabetes will not develop a neuropathic walking track pattern[9,10], and will have improved lower extremity motor function[11] and improved perception of pain[12]. These studies confirm experimentally the hypothesis I proposed in 1988[13,14], that the double crush concept did apply to diabetes clinically: the underlying pathophysiology of diabetes acts as the first crush, or site of compression, making the nerve susceptible to more distal sites of compression.
Subsequently, 19 Level IV studies[6-8,15-29], two systematic reviews[30,31], and three Level I studies[32-34] have all concluded that decompression of lower extremity nerves in diabetics relieves pain, improves sensation, and prevents ulcers and amputations. There have been two economic cost-benefit analyses using the decision-tree approach that concluded that the cost of surgical decompression is less than the cost of standard medical care for the treatment of diabetic neuropathy[35,36]. The two most recent approaches, using the highest form of analysis, Markov analysis, not only confirmed that the cost of surgical decompression is less than the cost of standard medical care for the treatment of diabetic neuropathy, but also proved that surgical decompression of lower extremity nerves improves the quality of life and even prolongs life[37,38].
The results of the Markov cost-effectiveness studies are worth further comment. For example, from the study from the Johns Hopkins School of Hygiene and Public Health[37]: when compared to standard medical “prevention” (treatment), for a patient population of 10,000, surgical decompression of lower extremity nerves with the Dellon Approach prevented a total of 1447 ulcers and 409 amputations over a period of 5 years. The quality-adjusted incremental effectiveness (QALY) was 0.41. A QALY of 1.0 means a perfectly healthy life without disability for 1 year. To put this increase of 0.41 into perspective, the QALY for a person with diabetic neuropathy is 0.40, so that this surgery doubled the quality of life for the person who has undergone surgery. In relation to survival, given the difference in death rates between the two prevention strategies, medical vs. surgical, survival was 73% for those receiving medical prevention compared to 95% for those undergoing surgery. The surgery-treated group lived longer because they had fewer ulcers, fewer hospital admissions for infection, and fewer amputations.
THE DELLON APPROACH TO NERVE DECOMPRESSION IN THE DIABETIC
Making the diagnosis of neuropathy
What is the approach to the person who has any symptom of numbness, tingling, pain, or any combination of these in the feet? If the symptoms are bilateral and include the dorsum and the plantar aspect of the foot, we have little doubt that the diagnosis is neuropathy. As a Peripheral Nerve Surgeon, the person you are seeing may not have been evaluated appropriately for the presence of a medically treatable etiology of neuropathy. Before assuming the patient has diabetic neuropathy, it is critical to do a two-hour oral glucose tolerance test (OGTT). All too often, a patient will see me who has been told they have “idiopathic neuropathy”, meaning the usual tests for serum folate/B12 levels, autoimmune disease, heavy metal toxicity, hypothyroid, HbA1c and serum glucose are normal, yet they have not had this OGTT, a stress test. Up to 56% of idiopathic neuropathy patients will have an abnormal OGTT, meaning that they have impaired glucose tolerance[39]. Whether their medical doctor will or will not tell them they have diabetes, their peripheral nerves are subjected to a hyperosmolar condition related to excess serum glucose, causing the nerve to swell. This swelling, in the presence of a known site of anatomic narrowing, like the tarsal tunnel region or the fibular tunnel, is the usual cause of chronic compression.
Of course, the history is important too in making the diagnosis. For example, chemotherapy-induced neuropathy, today usually due to treatment with a “platin” or “taxol” drug that binds to tubulin in the axoplasm of the nerve, can cause neuropathy. The results of lower extremity nerve decompression for the treatment of chemotherapy-induced neuropathy, neuropathy that persists for more than six months after the cessation of chemotherapy, can be as successful as for the treatment of diabetic neuropathy. This has been proven experimentally[40] and clinically[41]. Indeed, the Dellon Approach is as successful in the treatment of idiopathic neuropathy as it is in treating diabetic neuropathy[27,42]. Furthermore, once the patient with Leprosy has received triple antibiotic therapy and is no longer infectious, but has a disability related to the immune-mediated swelling along the course of superficial peripheral nerves, like branches of the peroneal nerve at the knee (fibular tunnel), leg (superficial peroneal nerve) or foot dorsum (deep peroneal nerve), then neurolysis of these lower extremity nerves can also be successful[42,43].
Electrodiagnostic testing will most likely have been done prior to the patient ever seeing the surgeon, and is quite successful at identifying a symmetrical neuropathy, especially if there is decreased number of axons present. However, electrodiagnostic testing, even in the upper extremity, where it is most sensitive, is often unable to identify a chronic nerve compression in a person who does not have neuropathy and is very unlikely to identify a superimposed chronic nerve compression in the presence of an underlying neuropathy due to the inherent nature of the neuropathy upon the axons[44-46]. Similar reasoning applies to the lower extremity, where 50% of asymptomatic people over the age of 55 have no medial plantar response and have motor fasciculations[47-49].
MAKING THE DIAGNOSIS OF CHRONIC NERVE COMPRESSION
If the electrodiagnostic testing has demonstrated a superimposed chronic nerve compression at a known site of anatomic narrowing, then the diagnosis has been confirmed objectively. Jules Tinel, MD, a Neurologist in France, and Paul Hoffman, PhD, a Physiologist in Germany, both described, independently, in 1915, the tingling sign that results from a peripheral nerve regenerating distally[50]. Beginning with Phalen’s description of carpal tunnel syndrome in 1966, the Hoffman-Tinel sign (hereinafter referred to as the Tinel sign) has been accepted as identifying the site of a nerve compression along the course of a peripheral nerve[51]. In my experience, this sign is sufficient if the site of compression is close to the target skin territory, like the dorsum of big toe/1st web space when the deep peroneal nerve is lightly tapped at the junction of the first and second metatarsal and the cuneiform bone, or the tibial nerve in the tarsal tunnel. However, for the common peroneal nerve at the fibular neck, there is often NOT a distally radiating perception, but just tenderness of the nerve or proximal radiation of the tingling. This sign, described by Francoise Louise Isidore Valleix, MD, in 1841[52], has been proven to be valid in my clinical experience at localizing a site of nerve compression for the common peroneal nerve at the fibular neck.
The reason there has been reported so much lack of sensitivity and specificity of the Tinel sign is that the presence of a positive Tinel sign varies according to the degree of compression, that is, the underlying pathophysiology present at the time of testing. Early in nerve compression, there is just endoneurial edema, and there may be no symptoms or just paresthesias, but once demyelination begins, the Tinel sign appears, and once an advanced axonal loss occurs, the Tinel sign can disappear[53-55]. The presence of a positive Tinel sign can also vary depending upon how hard the nerve is palpated and the experience of the examiner[56].
Therefore, over the past more than 40 years, if I can elicit a Tinel sign at a known site of anatomic narrowing, I am confident that there is a chronic nerve compression present. In the lower extremity, the presence of a positive Tinel sign over the tibial nerve in the tarsal tunnel has proven to have at least an 80% positive predictive value for good to excellent results from lower extremity peripheral nerve compression from the now “classic” Dellon Triple nerve decompression (neurolysis of the common peroneal nerve at the knee, the deep peroneal nerve at the foot dorsum, the release of the tarsal tunnel with its included neurolysis of the medial, lateral and calcaneal nerves)[41,57,58].
THE IDEAL SURGICAL CANDIDATE
An ideal patient is a person with diabetes who has symptoms of numbness and tingling with or without pain. The person who has just pain, without numbness, may not be an ideal candidate as that patient might have small fiber neuropathy. Small fiber neuropathy is rare but can be identified by a skin biopsy that quantitates unmyelinated nerve fibers in the dermis of the leg and thigh in the presence of normal tests for large fiber function. The skin biopsy will likely be positive in patients with the commonest form of diabetic neuropathy (a mixed large and small fiber neuropathy), and also in patients with an advanced form of chronic nerve compression without diabetes. In chronic nerve compression, both large, myelinated fibers and small, unmyelinated fibers can undergo degeneration[59]. What must be present in the ideal candidate for surgery are large fiber symptoms, such as tingling and numbness, and some measurement of large fiber function that is abnormal, such as vibratory perception threshold (quantitative vibrometry), or touch perception threshold (Pressure-Specified Sensory Devicetm or Semmes-Weinstein monofilaments), or abnormal static or moving two-point discrimination[60-63]. An abnormal electrodiagnostic test that shows nerve compression is also a form of large fiber evaluation.
The ideal candidate for decompression should have had an extensive medical trial of neuropathic pain medications, such as Neurontin, Gabapentin, Duloxetine, Elavil, or a combination of these drugs, and found that they had too many side effects or else were ineffective.
The ideal candidate for decompression, in addition to having the correct diagnosis, must have good circulation in the lower extremities. This can be determined by palpating the pulse, and if this examination is not clearly in favor of good arterial inflow, then Doppler flow studies, ankle/brachial index, and, if needed, cutaneous oxygen levels can be ascertained. The surgical incisions clearly may not heal in the absence of sufficient circulation. The same can be said for pedal edema. In the presence of cardiac or renal problems, edema is present, which is a contra-indication to surgery.
In addition to the positive Tinel sign of the tibial nerve, as discussed above, a good prognosis can be expected if the patient has had previously successful carpal tunnel surgery[64]. From a database of 300 patients who had a Dellon Approach to their lower extremity nerve compressions, 35 patients were found who had previous carpal tunnel release. The presence of a good response to median nerve decompression at the wrist gave an 88% positive predictive value to response to the decompression of the tibial and peroneal nerves.
SURGICAL DECOMPRESSION
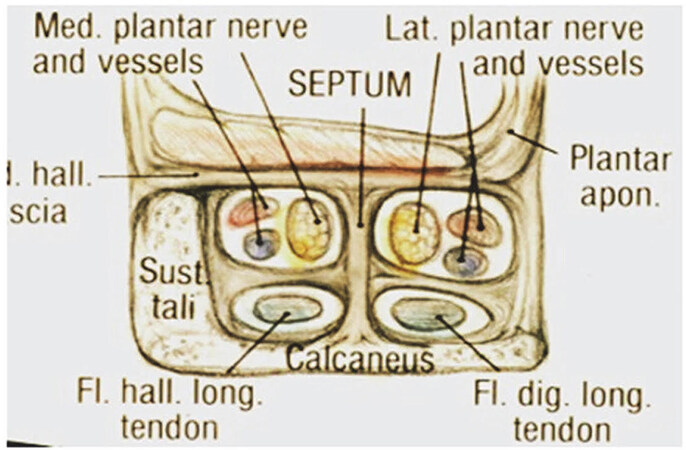
The main concept is that the stocking distribution of symptoms present in diabetic neuropathy can be understood as compression of the peroneal and tibial nerves. The original approach I took to surgical decompression required understanding that the tarsal tunnel is NOT the carpal tunnel anatomically
Figure 3. Illustration of a cross-section through the tarsal tunnels to compare to the carpal tunnel. Note that the flexor/abductor muscles in the foot correspond to the thenar muscles in hand, and cover the roof of the medial plantar nerve, homologous to the median nerve, and the lateral plantar nerve, homologous to the lateral plantar nerve. The septum between medial and lateral plantar tunnels is homologous to the hook process of the hamate carpal bone.
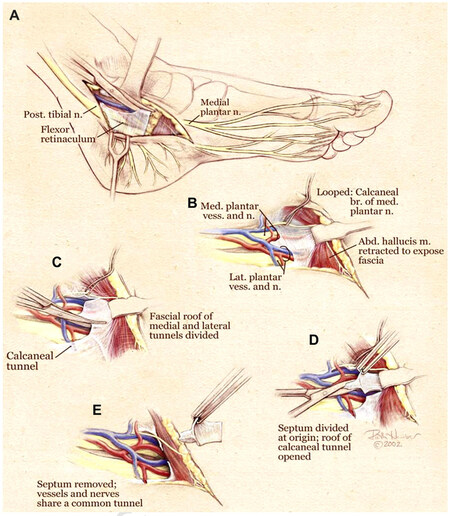
Figure 4. Illustration of decompression of the tarsal tunnels. The tarsal tunnel itself is opened to identify the anatomy leading to the more distal tunnels, and anomalous anatomy. The muscles are retracted to reveal the roof of the medial and roof of the lateral plantar tunnel. These roof structures are released distally and the septum between the tunnels removed. Finally, the calcaneal tunnel is released.
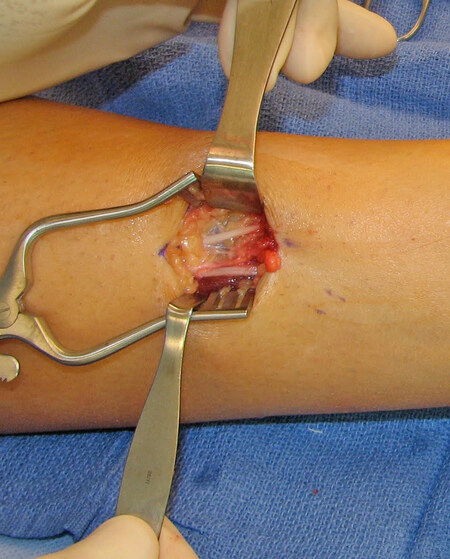
The anatomical basis of these techniques has been described for the deep peroneal over the dorsum of the foot [Figure 5][70], the common peroneal nerve at the fibular neck[71], and variations of the superficial peroneal nerve in the leg [Figure 6 ][72]. The actual surgical techniques for the four medial ankle tunnels are illustrated in Figure 4 and have been described in detail in the past[73-75]. Videos of the surgery can be viewed on YouTube.com for the tarsal tunnel decompress (https://www.youtube.com/watch?v=coBfi9NDjUM&t=36s) and the peroneal nerve decompressions (https://www.youtube.com/watch?v=Qlte57IHBzE&t=37s).
Figure 5. The deep peroneal nerve has been released over the dorsum of the foot by resecting the extensor digitorum brevis to the hallux. This tendon compresses the underlying nerve against the cuneiform bone.
Figure 6. The superficial peroneal nerve usually exits the fascia of the lateral compartment, where it becomes entrapped. In about 25% of patients, there is a high division of this nerve such that it has a branch in both the lateral and anterior compartment. Therefore, in every patient, we teach to open both compartments. An example of such a patient is shown here after decompression.
When should you consider neurolysis of the superficial peroneal nerve? The superficial peroneal nerve most always exits from the fascia of the lateral compartment about 6 to 8 cm proximal to the lateral malleolus. Sometimes there is a small bulge marking the spot. If there is a positive Tinel sign at that site, then neurolysis of this nerve should be added to the classic Dellon Triple. This can easily be added to the operation without additional post-op rehabilitation or morbidity but remember to use the bipolar cautery along the edge of the fascia before dividing the fascia to minimize post-operative bruising.
For the peroneal nerve, the multiple crush concept extends the double crush concept as follows; The first source of reduced axoplasmic flow is diabetes itself, with compression of the common peroneal nerve being the second crush, the superficial peroneal nerve being the third crush site, and the deep peroneal nerve being the fourth site. The first site cannot be changed. Theoretically, the vertebral foramen and the sciatic notch could be added, but as a matter of practicality, these sites are not easily decompressed, so they are not included. What can be approached safely are the common, superficial, and deep peroneal nerves. Although it is not clear experimentally that all need to be decompressed, if there has been a Tinel sign present, then that site is included in the surgical approach. Also, remember to open the anterior compartment, as 25% of people will have a branch of the superficial peroneal nerve located in this compartment [Figure 6][76].
For the tibial nerve, a site proximal to the tarsal tunnel had not been identified until 2009[76,77]. This clinical problem was raised not in the setting of neuropathy but in the setting of “failed tarsal tunnel decompression”. It is well documented in upper extremity surgery that a “failed” carpal tunnel release can be due to proximal compression beneath the pronator teres deep head. A similar site in the lower extremity would be the fibrous arcade of the soleal sling, which gives origin to the soleus muscle. This site is at the soleal sling [Figure 6] and is identified clinically by two physical exam findings: weakness of the flexor hallucis longus and tenderness in the calf about 8 cm below the knee joint, a site similar to that of the Homan’s sign for deep vein thrombosis. Sometimes a 3T MRI will show changes in the tibial nerve at this location, but it is unusual for the electrodiagnostic testing to be abnormal. The surgical technique has been described as well as the clinical results[78-80]. While the surgical exposure for this neurolysis is extensive and risks injury to the popliteal vessels, the post-operative course is easier than for tarsal tunnel decompression (see below). This raises the question of if a patient has both tarsal tunnel and soleal sling sites of compression, should both sites be operated upon at the same time. My current approach is to consider that tarsal tunnel release will not recover toe flexion, but will require the use of a walker for three weeks, and that it is conceivable that the proximal neurolysis will restore sensation to the plantar aspect obviating the need to do the tarsal tunnel decompressions (TTD). If the plantar sensation is not recovered, TTD can be done three months later.
REHABILITATION AFTER DELLON DECOMPRESSION
The first reported tarsal tunnel decompressions were case reports by Lam and Keck in 1962[80,81]. They recommended the use of crutches and non-weight bearing for three weeks post-operatively. We know today that if a peripheral nerve is immobilized after neurolysis, it is likely to become adherent during wound healing. Therefore, my post-op regimen requires the use of a bulky “Robert Jones” type dressing[82] and immediate walking using a walker [Figure 7]. The patient is instructed to “march”, lifting the operated foot from the knee, thereby avoiding much ankle flexion, and preventing sutures from pulling out of what is often skin with poor sensibility. Steps can be climbed sideways. The dressing is removed on post-op day #7 and betadine is applied twice a day thereafter. Sutures at the knee and leg are removed on post-op day #14, and at the ankle on post-op day #21. Water walking is begun on post-op day #22, three to four times per week, 15 to 20 minutes per time, and increased thereafter as tolerated.
Figure 7. In order to facilitate the gliding of the decompressed nerves, immediate mobilization is permitted by using a bulky Robert Jones type dressing, and a walker. In this figure, the patient I seen walking to the toilet prior to going home via wheelchair. The dressing limits ankle range of motion to less than 30 degrees, reducing the chance of the sutures tearing through the skin that has very little sensation. This dressing is used for the first week. The walker is used for three weeks until the sutures are removed at the ankle.
BARRIERS TO ACCEPTANCE & IMPLEMENTATION OF THIS SURGICAL APPROACH
Lack of awareness of the Dellon Approach to decompress peripheral nerves in diabetics with chronic nerve compression is probably the biggest obstacle to implementation today. The study by Melenhorst et al., from Zwolle in the Netherlands, best illustrates this problem[31]. In that study, they asked physicians and diabetes nurse educators the following questions:
1. “Are you aware of the theory that nerve compression injury plays a part in the pathophysiology of diabetic neuropathy?”
2. “Do you think that nerve compression injury may play a role in the development of diabetic neuropathy?”
3. “Are you aware of the potential value of nerve decompression surgery in the treatment of peripheral diabetic neuropathy?”
4. “Do you refer to other medical professionals when considering diabetic neuropathy?”
5. “Do you explain to the patient that peripheral diabetic neuropathy is an irreversible condition?”
Table 1 contains the results of their study. On average, just 35% of health care practitioners were aware of this approach and just 9% appreciated its value. Only 3% of these health care providers referred patients to a surgeon for the surgical approach. This study was done in the Netherlands, where the first randomized control study was reported using the Dellon Approach.
Includes data from the study performed by Melenhorst et al. evaluating the awareness of the general medical community of the surgical approach to peripheral neuropathy[31]
| Aware of theory | Aware of surgery value | Explains neuropathy is reversible | Refers to surgeon | |
| General practitioner | 19% | 6% | 45% | 3% |
| Internist | 32% | 11% | 46% | 0% |
| Neurologist | 35% | 22% | 57% | 9% |
| Diabetes nurse | 15% | 5% | 35% | NA |
| Overall | 23% | 9% | 35% | 3% |
The questions to be addressed today are “How can we best educate those health care professionals throughout the world to learn that (1) diabetics have an increased prevalence of chronic nerve compressions, (2) how to diagnose a chronic nerve compression, and (3) how to train surgeons interested in doing these procedures? I am hopeful that through a program aimed at providing this information to medical students early in their educational curriculum, an approach described elsewhere in an article in this issue of this journal, the future may hold optimism for those suffering from diabetic neuropathy[83].
CONCLUSION
The current evidence is overwhelmingly clear, in diabetics with neuropathy and a positive Tinel sign over the tibial nerve at the tarsal tunnel, that decompression, by neurolysis of lower extremity nerves, can relieve pain, restore sensation, and prevent ulceration and amputation. Furthermore, lower extremity nerve compression in diabetics with neuropathy and superimposed chronic nerve compression is not only cost-effective compared to standard medical care, but also increases the quality of life and life expectancy.
DECLARATIONS
Author’s contributionThe author contributed solely to the article.
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestThe Author declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2022.
REFERENCES
1. Partanen J, Niskanen L, Lehtinen J, Mervaala E, Siitonen O, Uusitupa M. Natural history of peripheral neuropathy in patients with non-insulin-dependent diabetes mellitus. N Engl J Med 1995;333:89-94.
2. Hicks CW, Selvin E. Epidemiology of peripheral neuropathy and lower extremity disease in diabetes. Curr Diab Rep 2019;19:86.
3. Available from: www.who.int/diabetes/facts/en/diabcare0504.pdf. [Last accessed on 14 Jul 2022].
4. Dellon AL. Susceptibility of nerve in diabetes to compression: implications for pain treatment. Plast Reconstr Surg 2014;134:142S-50S.
6. Dellon AL. Treatment of symptoms of diabetic neuropathy by peripheral nerve decompression. Plast Reconstr Surg 1992;89:689-97.
7. Aszmann O, Tassler PL, Dellon AL. Changing the natural history of diabetic neuropathy: incidence of ulcer/amputation in the contralateral limb of patients with a unilateral nerve decompression procedure. Ann Plast Surg 2004;53:517-22.
8. Dellon AL, Muse VL, Nickerson DS, et al. Prevention of ulceration, amputation, and reduction of hospitalization: outcomes of a prospective multicenter trial of tibial neurolysis in patients with diabetic neuropathy. J Reconstr Microsurg 2012;28:241-6.
9. Dellon ES, Dellon AL. Functional assessment of neurologic impairment: track analysis in diabetic and compression neuropathies. Plast Reconstr Surg 1991;88:686-94.
10. Sahin C, Karagoz H, Yuksel F, et al. The effect of perineurotomy on nerve regeneration in diabetic rats. Plast Reconstr Surg 2012;130:651e-61e.
11. Siemionow M, Sari A, Demir Y. Effect of early nerve release on the progression of neuropathy in diabetic rats. Ann Plast Surg 2007;59:102-8.
12. Barac S, Jiga LP, Barac B, Hoinoiu T, Dellon AL, Ionac M. Hindpaw withdrawal from a painful thermal stimulus after sciatic nerve compression and decompression in the diabetic rat. J Reconstr Microsurg 2013;29:63-6.
14. Dellon AL, Mackinnon SE, Seiler WA 4th. Susceptibility of the diabetic nerve to chronic compression. Ann Plast Surg 1988;20:117-9.
15. Wieman TJ, Patel VG. Treatment of hyperesthetic neuropathic pain in diabetics. Decompression of the tarsal tunnel. Ann Surg 1995;221:660-4; discussion 664.
16. Caffee H. Treatment of diabetic neuropathy by decompression of the posterior tibial nerve. Plast Reconstr Surg 2000;106:813-5.
17. Aszmann OC, Kress KM, Dellon AL. Results of decompression of peripheral nerves in diabetics: a prospective, blinded study. Plast Reconstr Surg 2000;106:816-22.
18. Tambwekar DS. Extended neurolysis of the posterior tibial nerve to improve sensation in diabetic neuropathic feet. Plast Reconstr Surg 2001;108:1452-3.
19. Wood WA, Wood MA. Decompression of peripheral nerves for diabetic neuropathy in the lower extremity. J Foot Ankle Surg 2003;42:268-75.
20. Biddinger KR, Amend KJ. The role of surgical decompression for diabetic neuropathy. Foot Ankle Clin 2004;9:239-54.
21. Rader AJ. Surgical decompression in lower-extremity diabetic peripheral neuropathy. J Am Podiatr Med Assoc 2005;95:446-50.
22. Yao Y, Wang RZ. Peripheral nerve decompression (Dellon procedure) and diabetic neuropathy. Chinese J Med 2005;10:1756-8.
23. Siemionow M, Alghoul M, Molski M, Agaoglu G. Clinical outcome of peripheral nerve decompression in diabetic and nondiabetic peripheral neuropathy. Ann Plast Surg 2006;57:385-90.
24. Karagoz H, Yuksel F, Ulkur E, Celikoz B. Early and late results of nerve decompression procedures in diabetic neuropathy: a series from Turkiye. J Reconstr Microsurg 2008;24:95-101.
25. Nickerson DS. Low recurrence rate of diabetic foot ulcer after nerve decompression. J Am Podiatr Med Assoc 2010;100:111-5.
26. Knobloch K, Gohritz G, Vogt PM. Surgical decompression of the lower leg in painful diabetic polyneuropathy. Oper Orthop Traumatol 2012;24:74-9.
27. Valdivia JM, Weinand M, Maloney CT Jr, Blount AL, Dellon AL. Surgical treatment of superimposed, lower extremity, peripheral nerve entrapments with diabetic and idiopathic neuropathy. Ann Plast Surg 2013;70:675-9.
28. Zhang W, Zhong W, Yang M, Shi J, Guowei L, Ma Q. Evaluation of the clinical efficacy of multiple lower-extremity nerve decompression in diabetic peripheral neuropathy. Br J Neurosurg 2013;27:795-9.
29. Yang W, Guo Z, Yu Y, Xu J, Zhang L. Pain relief and health-related quality-of-life improvement after microsurgical decompression of entrapped peripheral nerves in patients with painful diabetic peripheral neuropathy. J Foot Ankle Surg 2016;55:1185-9.
30. Baltodano PA, Basdag B, Bailey CR, et al. The positive effect of neurolysis on diabetic patients with compressed nerves of the lower extremities: a systematic review and meta-analysis. Plast Reconstr Surg Glob Open 2013;1:e24.
31. Melenhorst WB, Overgoor ML, Gonera EG, Tellier MA, Houpt P. Nerve decompression surgery as treatment for peripheral diabetic neuropathy: literature overview and awareness among medical professionals. Ann Plast Surg 2009;63:217-21.
32. Maurik JFMM, van Hal M, van Eijk RPA, Kon M, Peters EJG. Value of surgical decompression of compressed nerves in the lower extremity in patients with painful diabetic neuropathy: a randomized controlled trial. Plast Reconstr Surg 2014;134:325-32.
33. Best TJ, Best CA, Best AA, Fera LA. Surgical peripheral nerve decompression for the treatment of painful diabetic neuropathy of the foot - a level 1 pragmatic randomized controlled trial. Diabetes Res Clin Pract 2019;147:149-56.
34. Rozen S, Wolfe G, Raskin P, et al. .
35. Garrod K. Prevention of ulceration and amputation, by neurolysis of peripheral nerves in diabetics with neuropathy and nerve compression: decisiontree utility analysis. J Diabetes Metab 2014;5:5.
36. Rankin TM, Miller JD, Gruessner AC, Nickerson DS. Illustration of cost saving implications of lower extremity nerve decompression to prevent recurrence of diabetic foot ulceration. J Diabetes Sci Technol 2015;9:873-80.
37. Sarmiento S, Pierre JA Jr, Dellon AL, Frick KD. Tibial nerve decompression for the prevention of the diabetic foot: a cost-utility analysis using markov model simulations. BMJ Open 2019;9:e024816.
38. Rinkel WD, Franks B, Birnie E, Castro Cabezas M, Coert JH. Cost-effectiveness of lower extremity nerve decompression surgery in the prevention of ulcers and amputations: a markov analysis. Plast Reconstr Surg 2021;148:1135-45.
39. Tassler P, Dellon AL, Lesser GJ, Grossman S. Utility of decompressive surgery in the prophylaxis and treatment of cisplatin neuropathy in adult rats. J Reconstr Microsurg 2000;16:457-63.
40. Dellon AL, Swier P, Maloney CT Jr, Livengood MS, Werter S. Chemotherapy-induced neuropathy: treatment by decompression of peripheral nerves. Plast Reconstr Surg 2004;114:478-83.
41. Lee CH, Dellon AL. Prognostic ability of Tinel sign in determining outcome for decompression surgery in diabetic and nondiabetic neuropathy. Ann Plast Surg 2004;53:523-7.
42. Wan EL, Rivadeneira AF, Jouvin RM, Dellon AL. Treatment of peripheral neuropathy in leprosy: the case for nerve decompression. Plast Reconstr Surg Glob Open 2016;4:e637.
43. Wan EL, Rivadeniera AF, Serrano HA, et al. Protocol for a randomized controlled trial investigating decompression for leprous neuropathy (the DELN protocol). Lepr Rev ;2016:87:553-61.
44. Rempel D, Evanoff B, Amadio PC, et al. Consensus criteria for the classification of carpal tunnel syndrome in epidemiologic studies. Am J Public Health 1998;88:1447-51.
45. Szabo RM, Slater RR Jr, Farver TB, Stanton DB, Sharman WK. The value of diagnostic testing in carpal tunnel syndrome. J Hand Surg Am 1999;24:704-14.
46. Perkins BA, Olaleye D, Bril V. Carpal tunnel syndrome in patients with diabetic polyneuropathy. Diabetes Care 2002;25:565-9.
47. Fealey RD, Litchy WJ, Daube JR. Plantar nerve-stimulation in evaluation of peripheral nerves. Neurology 1980;30:412.
48. Falck B, Alaranta H. Fibrillation potentials, positive sharp waves and fasciculation in the intrinsic muscles of the foot in healthy subjects. J Neurol Neurosurg Psychiatry 1983;46:681-3.
49. Patel AT, Gaines K, Malamut R, Park TA, Toro DR, Holland N. American Association of Neuromuscular and Electrodiagnostic Medicine. Usefulness of electrodiagnostic techniques in the evaluation of suspected tarsal tunnel syndrome: an evidence-based review. Muscle Nerve 2005;32:236-40.
50. Sansone JM, Gatzke AM, Aslinia F, Rolak LA, Yale SH. Jules Tinel (1879-1952) and Paul Hoffman (1884-1962). Clin Med Res 2006;4:85-9.
52. Valleix FLI. Traité des névralgies: ou, Affections douloureuses des nerfs - Treatise on neuralgia; painful disorders of the nerves, 1841. Available from: https://books.google.com.hk/books?hl=zh-CN&lr=&id=9lj9A518SaMC&oi=fnd&pg=PA6&dq=+Valleix,+FLI+++Traite%CC%81+des+ne%CC%81vralgies,+ou,+Affections+douloureuses+des+nerfs,+%E2%80%93+Treatise+on+neuralgia%3B+painful+disorders+of+the+nerves,+1841.&ots=cTgncEtSfH&sig=Zcu0W_cyXbEquJEaBrfveqvyB-4&redir_esc=y#v=onepage&q&f=false [Last accessed on 14 Jul 2022].
54. Mackinnon SE, Dellon AL, Hudson AR, Hunter DA. Chronic nerve compression - an experimental model in the rat. Ann Plast Surg 1984;13:112-20.
55. Mackinnon SE, Dellon AL, Hudson AR, Hunter DA. A primate model for chronic nerve compression. J Reconstr Microsurg 1985;1:185-95.
56. Lifchez SD, Means KR Jr, Dunn RE, Williams EH, Dellon AL. Intra- and inter-examiner variability in performing Tinel’s test. J Hand Surg Am 2010;35:212-6.
57. Rinkel WD, Castro Cabezas M, van Neck JW, Birnie E, Hovius SER, Coert JH. Validity of the Tinel sign and prevalence of tibial nerve entrapment at the tarsal tunnel in both diabetic and nondiabetic subjects: a cross-sectional study. Plast Reconstr Surg 2018;142:1258-66.
58. Dellon AL, Muse VL, Scott ND, et al. A positive Tinel sign as predictor of pain relief or sensory recovery after decompression of chronic tibial nerve compression in patients with diabetic neuropathy. J Reconstr Microsurg 2012;28:235-40.
59. Dellon AL. Abnormal skin biopsy for intraepidermal nerve fibers: when “Decreased small nerve fibers” is not “Small fiber neuropathy”. Microsurgery 2015;35:505-6.
60. Tassler PL, Dellon AL. Correlation of measurements of pressure perception using the pressure-specified sensory device with electrodiagnostic testing. J Occup Environ Med 1995;37:862-6.
61. Tassler PL, Dellon AL, Scheffler NM. Computer-assisted measurement in diabetic patients with and without foot ulceration. J Am Podiatr Med Assoc 1995;85:679-84.
62. Radoiu H, Rosson GD, Andonian E, Senatore J, Dellon AL. Comparison of measures of large-fiber nerve function in patients with chronic nerve compression and neuropathy. J Am Podiatr Med Assoc 2005;95:438-45.
63. Rinkel WD, Castro Cabezas M, Coert JH. A new application of the Rotterdam Diabetic Foot Study Test Battery: grading pedal sensory loss to predict the risk of foot ulceration. Diabetes Res Clin Pract 2021;175:108836.
64. Maloney CT Jr, Dellon AL, Heller C Jr, Olson JR. Prognostic ability of a good outcome to carpal tunnel release for decompression surgery in the lower extremity. Clin Podiatr Med Surg 2006;23:559-67.
65. Mackinnon SE. Homologies between the tarsal and carpal tunnels: implications for surgical treatment in the tarsal tunnel syndrome. Contemp Orthop 1987;14:75-8.
66. Dellon AL, Kim J, Spaulding CM. Variations in the origin of the medial calcaneal nerve. J Am Podiatr Med Assoc 2002;92:97-101.
67. Dellon AL. The four medial ankle tunnels: a critical review of perceptions of tarsal tunnel syndrome and neuropathy. Neurosurg Clin N Am 2008;19:629-48, vii.
68. Barker AR, Rosson GD, Dellon AL. Pressure changes in the medial and lateral plantar and tarsal tunnels related to ankle position: a cadaver study. Foot Ankle Int 2007;28:250-4.
69. Rosson GD, Larson AR, Williams EH, Dellon AL. Tibial nerve decompression in patients with tarsal tunnel syndrome: pressures in the tarsal, medial plantar, and lateral plantar tunnels. Plast Reconstr Surg 2009;124:1202-10.
71. Dellon AL, Ebmer J, Swier P. Anatomic variations related to decompression of the common peroneal nerve at the fibular head. Ann Plast Surg 2002;48:30-4.
72. Rosson GD, Dellon AL. Superficial peroneal nerve anatomic variability changes surgical technique. Clin Orthop Relat Res 2005;438:248-52.
73. Dellon AL. Diabetic neuropathy: review of a surgical approach to restore sensation, relieve pain, and prevent ulceration and amputation. Foot Ankle Int 2004;25:749-55.
74. Dellon AL. Diabetic neuropathy: medical and surgical approaches. Clin Podiatr Med Surg 2007;24:425-48, viii.
75. Dellon AL. The Dellon approach to neurolysis in the neuropathy patient with chronic nerve compression. Handchir Mikrochir Plast Chir 2008;40:351-60.
76. Ducic I, Dellon AL, Graw KS. The clinical importance of variations in the surgical anatomy of the superficial peroneal nerve in the mid-third of the lateral leg. Ann Plast Surg 2006;56:635-8.
77. Williams EH, Williams CG, Rosson GD, Dellon LA. Anatomic site for proximal tibial nerve compression: a cadaver study. Ann Plast Surg 2009;62:322-5.
78. Williams EH, Williams CG, Rosson GD, Dellon AL. Combined peroneal and proximal tibial nerve palsies. Microsurgery 2009;29:259-64.
79. Williams EH, Rosson GD, Hagan RR, Hashemi SS, Dellon AL. Soleal sling syndrome (proximal tibial nerve compression): results of surgical decompression. Plast Reconstr Surg 2012;129:454-62.
82. Girdlestone GR. The robert jones tradition. J Bone Joint Surg 1948;30B:187-95. Available from: https://online.boneandjoint.org.uk/doi/pdf/10.1302/0301-620x.30b1.187 [Last accessed on 14 Jul 2022]
83. Lee EB, Podsednik BS, Khoo K, et al. The virtual peripheral nerve academy: training for the identification and treatment of peripheral nerve disorders. Plast & Aesth Research. Forthcoming 2022.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Dellon AL. Nerve decompression in diabetics with chronic nerve compression: update 2022. Plast Aesthet Res 2022;9:45. http://dx.doi.org/10.20517/2347-9264.2022.13
AMA Style
Dellon AL. Nerve decompression in diabetics with chronic nerve compression: update 2022. Plastic and Aesthetic Research. 2022; 9(7): 45. http://dx.doi.org/10.20517/2347-9264.2022.13
Chicago/Turabian Style
Dellon, Arnold Lee. 2022. "Nerve decompression in diabetics with chronic nerve compression: update 2022" Plastic and Aesthetic Research. 9, no.7: 45. http://dx.doi.org/10.20517/2347-9264.2022.13
ACS Style
Dellon, AL. Nerve decompression in diabetics with chronic nerve compression: update 2022. Plast. Aesthet. Res. 2022, 9, 45. http://dx.doi.org/10.20517/2347-9264.2022.13
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 19 clicks
Cite This Article 19 clicks













Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.