Clinical application of autologous chyle fat transplantation in the correction of sunken upper eyelid
Abstract
Aim: We investigated the clinical application of autologous chyle fat in the correction of sunken upper eyelid.
Methods: From November 2020 to October 2021, 89 cases of correction with autologous chyle fat to sunken upper eyelid were performed (with or without other cosmetic procedures related to the eyes). An appropriate amount of fat was extracted from the superficial layer of the patient’s thigh and processed to chyle fat. About 0.5-2.8 mL of fat was injected under the orbicularis oculi muscle (roof-retro orbicularis oculi fat) or in the area where the orbital septal fat exists from the outer orbital margin of the upper eyelid.
Results: In total, 59 patients were followed up for 1-11 months after surgery. No infection, necrosis, vascular embolism, upper eyelid lumpiness, fat calcification, or liquefaction occurred in all patients, while seven cases showed inadequate correction. The depression basically disappeared, the shape was relatively full, the youthfulness was greatly improved, and the satisfaction of patients was high during the follow-up period.
Conclusion: The correction with autologous chyle fat to sunken upper eyelid showed little trauma, short recovery periods, and satisfactory results, and it is worthy of being popularized and applied more widely.
Keywords
INTRODUCTION
Sunken upper eyelid refers to the sunken malformation between the lower edge of the eyebrow and the upper edge of the eyeball due to any reason[1], which is mainly caused by the protruding imbalance between the bony tissue of the eyebrow and the soft tissue of the upper eyelid. The major causes[2] include congenital structural abnormalities, aging, surgery, trauma, chronic diseases, and some drugs[3]. Park proposed the degrees of sunken upper eyelid in 2011 as follows[4]: measure the distance from the upper orbital edge to the deepest depression of the eyelid, defining it as the depression depth. Grade 1 refers to the depression depth of less than 0.5 cm, the orbital edge is not protruding, and no skin tension. The depth of Grade 2 is between 0.5 and 1.0 cm. The depth of Grade 3 is not less than 1.0 cm. Grade 4 is combined with ptosis on the basis of Grade 3. Regarding the amount of fat transplantation, according to the opinions of other scholars[4,5], Grade 1 depression generally needs to be corrected by transplanting no more than 1.5 mL fat, Grade 2 may need 1.5-2.5 mL fat, and Grades 3 and 4 need at least 2.5 mL fat transplantation to correct the depression. The maximum amount of unilateral fat transplantation should not exceed 3 mL. Some scholars also proposed a complex formula to calculate the amount of fat[6], and the verification effect was very satisfactory.
In recent years, the correction of sunken upper eyelid has attracted more and more attention, as people with sunken upper eyelid appear tired and old, and long-term sunken upper eyelid also tends to increase the incidence of periocular diseases, such as ptosis, amblyopia, corneal erosion, etc. Current treatment strategies tend to compensate for the sunken upper eyelid with a variety of fillers. The main fillers currently used in clinical treatment are: fascia fat compound tissue flap[7], free fat flap, frontal muscle fascia flap and periosteum flap, dermal fat flap, orbital fat replacement, orbicularis oculi folding, hyaluronic acid filling, autologous fat transplantation[8], etc., as well as their combination. Studies have shown that some non-surgical treatments for sunken upper eyelid also have satisfactory results, such as plasma exeresis[9]. Autologous fat transplantation is widely used due to its convenient selection and good postoperative effect. Autologous fat transplantation mainly includes block fat transplantation, chyle fat transplantation[10,11], nano fat transplantation[12], and SVF-gel (stromal vascular fraction gel) transplantation[13]. The purpose of this study was to investigate the clinical effect of chyle fat in the treatment of sunken upper eyelid and to provide a suitable treatment idea for the treatment of sunken upper eyelid.
METHODS
In total, 89 cases were collected by the authors from November 2020 to October 2021. All patients were suffering from varying degrees of upper eyelid sag, without an eye disease or history of eyelid surgery. The patients with cardiovascular disease, diabetes, or long-term use of immunosuppressive or anticoagulant drugs were excluded. Dr. Qi performed autologous chyle fat transplantation on all patients, with or without other cosmetic procedures related to the eyes at the same time. All patients signed informed consent forms for surgery, and they understood all aspects in the consent forms. Preoperative and immediate postoperative photos were taken for all patients, and 59 patients provided long-term follow-up photos.
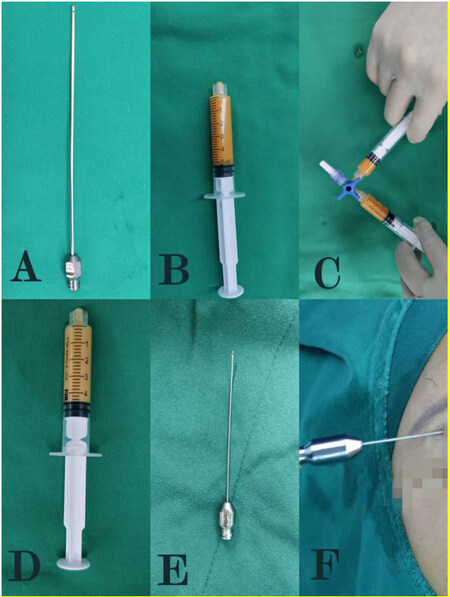
The patient was placed in a standing position and the physician measured the degree of upper eyelid depression and identified the fat donor site. Studies have shown that the content of adipogenic stem cells in the superficial fat of medial thigh and lower abdomen is high, and the fat retention rate will be relatively high after transplantation[14,15]. The specific intraoperative fat donor site should be determined by doctors and patients before the surgery. During the operation [Figure 1], a 20-mL syringe was used to inject an appropriate amount of swelling fluid (500 mL normal saline + lidocaine 300 mg + epinephrine 0.5 mg) into the subcutaneous fat layer. A blunt tip liposuction needle with a diameter of 1 mm was used under 3 mL negative pressure to aspirate the fat in the subcutaneous fat layer 15 min later, to minimize the fat damage. About 15 mL of fat was enough. Doctors used 2 mm diameter filters to remove fiber cords, and then removed impurities such as swelling of the liquid, oil, and blood after a 10 min precipitation. The syringe was connected to the ordinary fat converter and another empty syringe, 30 times back and forth rapidly (50 times/min), gradually transforming the contents into a yellowish white chyle fat. After local anesthesia
Figure 1. (A) A blunt tip liposuction needle with a diameter of 1 mm; (B) fat after settling for 20 min and removing the impurities; (C) the fat being moved back and forth; (D) chyle fat after moving back and forth rapidly 30 times (50 times/min); (E) a 0.8 mm diameter fat injection needle; and (F) fat injection.
After surgery, the fat donor area was covered with pressure dressing for three days with nothing on the fat transplant area. The wound was cleaned, and the dressing was changed on the first day after surgery. Cold compress was forbidden for fat in the transplantation area. Stitches were removed nine days after surgery on the fat donor area.
RESULTS
In total, 59 patients were followed up for 1-11 months after surgery. No infection, necrosis, vascular embolism, upper eyelid lumpiness, ptosis, retraction of upper eyelid, fat calcification, or liquefaction occurred in all patients, while seven cases showed inadequate correction. The depression basically disappeared, the shape was relatively full, the youthfulness was greatly improved, and the satisfaction of patients and doctors was high during the follow-up period. (Doctors’ satisfaction can be obtained by observing the comparison photos before and after surgery, while patients’ satisfaction can be obtained by communicating with patients.)
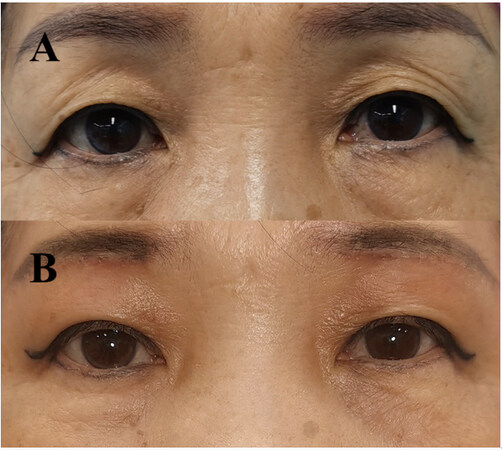
Figure 2 shows a 54-year-old female with the chief complaint of “sunken upper eyelid and sagging upper eyelid skin for more than three years”. The physical examination showed bilateral moderate upper eyelid depression, skin laxity, and multilayer double eyelid. She was operated on with upper eyelid laxity correction and autologous chyle fat transplantation, 2.0 mL on the left side and 2.0 mL on the right side. The patient’s upper eyelid was full on both sides, and the upper eyelid skin was slightly relaxed after six weeks.
Figure 2. (A) Preoperative, bilateral moderate upper eyelid depression, skin laxity, and multilayer double eyelid; and (B) six weeks after surgery, the upper eyelid was full and the upper eyelid skin was slightly relaxed.
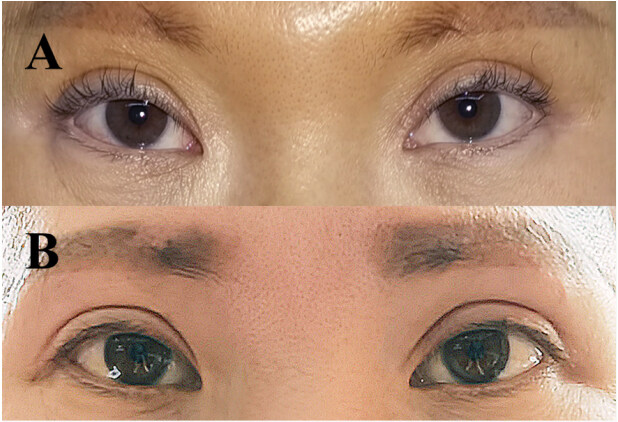
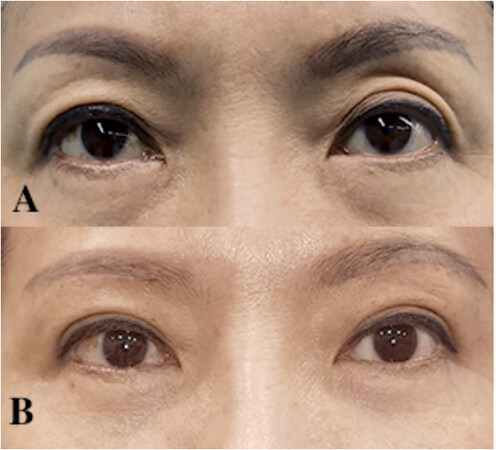
Figure 3 shows a 32-year-old female with the chief complaint of “sunken upper eyelid and sagging upper eyelid skin for more than three years”. The physical examination showed bilateral moderate upper eyelid depression. She was operated on with autologous chyle fat transplantation, 1.8 mL on the left side and
Figure 3. (A) Preoperative, bilateral moderate upper eyelid depression; and (B) three months after surgery, the upper eyelid was full, and the skin texture and elasticity of upper eyelid were significantly improved.
Figure 4 shows a 35-year-old female with the chief complaint of “sunken upper eyelid and sagging upper eyelid skin for more than three years”. The physical examination showed bilateral mild upper eyelid depression and skin laxity. She was operated on with upper eyelid laxity correction and autologous chyle fat transplantation, 1.0 mL on the left side and 1.0 mL on the right side. The patient’s upper eyelid was full on both sides, and the appearance of double eyelid was satisfactory after six months.
Figure 4. (A) Preoperative, bilateral moderate upper eyelid depression and skin laxity; and (B) six months after surgery, the upper eyelid was full and the appearance of double eyelid was satisfactory.
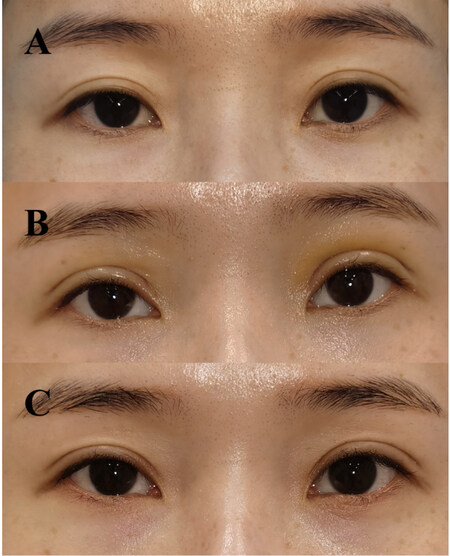
Figure 5 shows a 25-year-old female with the chief complaint of “sunken upper eyelid and multiple eyelid folds for more than four years”. The physical examination showed bilateral mild upper eyelid depression and poor shape of double eyelid. She was operated on with blepharoplasty and autologous chyle fat transplantation, 1.5 mL on the left side and 1.5 mL on the right side. The patient’s upper eyelid was full on both sides, and the double eyelid was beautiful after seven days. However, we found that the upper eyelid was still depressed after nine months. The surgeon decided to carry out a supplementary injection with autologous chyle fat. The supplemental volume was less than the previous injection because the depression had been somewhat improved.
Figure 5. (A) Preoperative, bilateral mild upper eyelid depression and poor shape of double eyelid; (B) seven days after surgery, the upper eyelid was full and double eyelid was beautiful; and (C) nine months after surgery, the upper eyelid was still depressed and needed supplementary injection.
Figure 6 shows a 58-year-old female with the chief complaint of “sunken upper eyelid and sagging upper eyelid skin for more than six years”. The physical examination showed moderate upper eyelid depression on the left side while mild on the right side, skin laxity, and poor shape of double eyelid. She was operated on with upper eyelid laxity correction and autologous chyle fat transplantation, 2.7 mL on the left side and
DISCUSSION
Currently, there are various treatment methods for sunken upper eyelid. Autologous chyle fat transplantation was used to treat sunken upper eyelid because it provides the following advantages: (1) There is no immune rejection for autologous fat transplantation; (2) Chyle fat particles are delicate and easy to be formed by self-adjustment through the eyes, avoiding problems such as unnatural shape after transplantation; (3) Chyle fat particles are small, contain more stem cell content, and have a wide contact surface with the surrounding blood donor tissue, which leads to better regeneration ability[16,17] as well as partially improves the skin texture of the upper eyelid; (4) The implanted fat can last much longer than hyaluronic acid after retention, remaining until its atrophy with age, and it is homogenous with the implanted tissue, being consistent with the physiological and anatomical characteristics of the orbital region, without affecting the function and appearance of the donor site; (5) The operation is simple, with little trauma at the fat donor site, no obvious postoperative scar, short postoperative recovery time, and short swelling period of a light degree.
Although the operation of autologous chyle fat transplantation for the treatment of sunken upper eyelid is easy to implement, the operation is performed under blind sight, requiring the operator to have a correct understanding of the upper eyelid anatomy and certain experience of filling injection. During the operation, fat entering blood vessels should be avoided as much as possible, and excessive bleeding should be avoided to reduce the postoperative effect. The surgeon injected the needle from the outer edge of the orbit of the upper eyelid, and then tilted it down to the loose space under the orbicularis oculi muscle to inject fat. The injection volume should not be too much, and the injection speed should not be too fast, so as to avoid fat entering the blood vessels as much as possible. In addition, the fat graft site should not be under the upper eyelid skin directly; otherwise, the upper eyelid might appear uneven after several weeks, with the possibility of the more serious condition of iatrogenic ptosis. Some studies have shown that fat graft should not be in the gap in front of the aponeurosis; these studies considered the orbicularis oculi and tendon membrane adhesion formation if the fat transplantation hardened or became necrotic, which may lead to artificial ptosis[18]. The surgeon mainly transplanted fat under the orbicularis oculi muscle (roof-retro orbicularis oculi fat) or in the area where the orbital septal fat exists. The most difficult part of autologous fat transplantation treatment is the postoperative fat retention. If the amount of autologous fat transplantation is too little, the correction effect is not satisfactory, while if the amount is too great, then fat nodules are easily found. Remember the principle of “too little is better than too much”. Supplementary transplantation can be performed 3-6 months later if an unsatisfactory effect is revealed[19].
In conclusion, with the continuous deepening of the understanding of the anatomy and function of the upper eyelid and the development of technology, operations to correct the depression of the upper eyelid will inevitably become more accurate and less invasive. The smallest trauma and the simplest method to achieve the best curative effect are our eternal pursuits. Autologous chyle fat transplantation correction of sunken upper eyelid has the advantages of less trauma, short recovery period, and satisfactory effect, which is worthy of wide application.
DECLARATIONS
Authors’ contributionsComplete the operation, propose design ideas, write articles and explain difficult problems: Qi L
Postoperative follow-up, photo editing, article review, literature search: Wang P
Preoperative photo shooting, data collation, article writing and literature search, concept search and interpretation: Chen X
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateThe study was conducted in accordance with the principles of the Declaration of Helsinki. This study was obtained the approval of Ethics Committee.
Consent for publicationA written informed consent for publication was obtained.
Copyright© The Author(s) 2022.
REFERENCES
1. Moon HS, Ahn B, Lee JH, Rah DK, Park TH. Rejuvenation of the deep superior sulcus in the eyelid. J Cosmet Dermatol 2016;15:458-68.
2. Liu Y, Zhao YY. Advances in pathogenesis and treatment of sunken upper eyelid. Chin J Aesthet Plast Surg 2021;32:298-300+308. (in Chinese).
3. Eftekhari K, Vagefi MR, Lee V, et al. In vivo effects of retrobulbar bimatoprost injection on orbital fat. Ophthalmic Plast Reconstr Surg 2018;34:201-4.
4. Park S, Kim B, Shin Y. Correction of superior sulcus deformity with orbital fat anatomic repositioning and fat graft applied to retro-orbicularis oculi fat for Asian eyelids. Aesthetic Plast Surg 2011;35:162-70.
5. Glasgold RA, Glasgold MJ, Lam SM. Complications following fat transfer. Oral Maxillofac Surg Clin North Am 2009;21:53-8, vi.
6. Gao L, Xu S, Li JC, et al. Clinical application of preoperative accurate grafting measurement of autogenous fat transplantation in the correction of upper eyelid depression. Chin J Aesthet Med 2020;29:6-9. (in Chinese).
7. Lee Y, Kwon S, Hwang K. Correction of sunken and/or multiply folded upper eyelid by fascia-fat graft. Plast Reconstr Surg 2001;107:15-9.
8. Shorr N, Christenbury JD, Goldberg RA. Free autogenous “pearl fat” grafts to the eyelids. Ophthalmic Plast Reconstr Surg 1988;4:37-40.
9. Sotiris TG, Nittari G, Sagaro GG, Amenta F. A descriptive study on the applications of plasma exeresis in dermatology. J Clin Aesthet Dermatol 2021;14:E58-E62.
10. Chen JN, Li ZH, Lai LY, Zhou GW, Liang LM, Chen ML. Preliminary study on biological characteristics of human chyle fat derived stem cells. Chin J Aesthet Med 2021;30:91-5. (in Chinese).
11. Xu X, Lai L, Zhang X, et al. Autologous chyle fat grafting for the treatment of hypertrophic scars and scar-related conditions. Stem Cell Res Ther 2018;9:64.
12. Tonnard P, Verpaele A, Peeters G, Hamdi M, Cornelissen M, Declercq H. Nanofat grafting: basic research and clinical applications. Plast Reconstr Surg 2013;132:1017-26.
13. Yao Y, Dong Z, Liao Y, et al. Adipose extracellular matrix/stromal vascular fraction gel: a novel adipose tissue-derived injectable for stem cell therapy. Plast Reconstr Surg 2017;139:867-79.
14. Khouri RK, Rigotti G, Cardoso E, Khouri RK Jr, Biggs TM. Megavolume autologous fat transfer: part I. Theory and principles. Plast Reconstr Surg 2014;133:550-7.
15. Xiong S, Yi C, Pu LLQ. An overview of principles and new techniques for facial fat grafting. Clin Plast Surg 2020;47:7-17.
16. Lin TM, Lin TY, Chou CK, Lai CS, Lin SD. Application of microautologous fat transplantation in the correction of sunken upper eyelid. Plast Reconstr Surg Glob Open 2014;2:e259.
17. Ramil ME. Fat grafting in hollow upper eyelids and volumetric upper blepharoplasty. Plast Reconstr Surg 2017;140:889-97.
18. Zhou X, Zeng N, Wang H. Correction of upper-eyelid depression through retro-orbicularis oculi fat (ROOF) Augmentation using periumbilical adipose graft. Aesthetic Plast Surg 2020;44:2131-6.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Qi L, Wang P, Chen X. Clinical application of autologous chyle fat transplantation in the correction of sunken upper eyelid. Plast Aesthet Res 2022;9:44. http://dx.doi.org/10.20517/2347-9264.2022.18
AMA Style
Qi L, Wang P, Chen X. Clinical application of autologous chyle fat transplantation in the correction of sunken upper eyelid. Plastic and Aesthetic Research. 2022; 9(7): 44. http://dx.doi.org/10.20517/2347-9264.2022.18
Chicago/Turabian Style
Qi, Lin, Pu Wang, Xingfan Chen. 2022. "Clinical application of autologous chyle fat transplantation in the correction of sunken upper eyelid" Plastic and Aesthetic Research. 9, no.7: 44. http://dx.doi.org/10.20517/2347-9264.2022.18
ACS Style
Qi, L.; Wang P.; Chen X. Clinical application of autologous chyle fat transplantation in the correction of sunken upper eyelid. Plast. Aesthet. Res. 2022, 9, 44. http://dx.doi.org/10.20517/2347-9264.2022.18
About This Article
Copyright
Data & Comments
Data

 Cite This Article 3 clicks
Cite This Article 3 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.