Soleus muscle flap for reconstruction of lower extremity trauma. Workhorse or glue factory?
Abstract
Aim: Soleus muscle flaps have traditionally been a reliable tool in the plastic surgeon’s armamentarium for lower extremity reconstruction and limb salvage. In the modern era, many surgeons prefer free flaps. This study sought to evaluate trends and outcomes of soleus flap reconstruction after lower extremity injury in a large cohort at a Level 1 trauma center.
Methods: This is an Institutional Review Board -approved, retrospective chart review that was undertaken at Los Angeles County + University of Southern California Medical Center from 2007 to 2021. Patient demographics, Gustilo-Anderson fracture classification, flap characteristics, and outcomes were collected and analyzed. Outcomes of interest included failure rates, postoperative complications, and long-term ambulatory status.
Results: Of 187 local leg flaps, 68 (36.4%) were soleus flaps, with 84% of soleus flaps performed prior to 2016. The flap loss rate was 0.0%. Eighteen (26.1%) flaps demonstrated > 1 complication, including osteomyelitis/hardware infection (n = 12), flap revision (n = 6), and amputation (n = 2). Long-term follow-up demonstrated 35.3% of patients ambulating independently after an average of 7.5 ± 7.2 months, with the remainder needing a wheelchair or walking assistance device.
Conclusion: Although soleus flap loss rate was 0%, the findings demonstrate more infections than expected; this must be considered in light of pre-existing patient comorbidities possibly deterring free flap placement. Additionally, our results reveal that only 16% of soleus flaps were performed after 2015. As surgeons consider the reconstructive ladder for lower extremity trauma, a rotational soleus muscle flap should not be overlooked in the modern era of free flap tissue transfers and might be a more optimal flap choice in certain patients with multiple comorbidities.
Keywords
INTRODUCTION
Hallmarks of limb salvage include hemostasis, patent vascular flow, bony fixation, infection control, and soft tissue coverage. Accordingly, the reconstructive surgeon is presented with a complex soft tissue injury unable to be closed primarily. Previously established treatment algorithms dictate the use of local calf muscles for the upper two-thirds of the leg while using free tissue transfer for the lower-third of the leg and foot[1-3]. Better insight into local flap anatomy and physiology has led to some centers even reporting a decreased reliance on free flaps for soft tissue coverage for traumatic lower extremity reconstruction[4].
Given finite flap options coupled with considerable soft tissue damage, traumatic reconstruction continues to pose a significant challenge to the reconstructive surgeon beyond the inherent risk of limb loss associated with limb salvage[5]. Inclusion of muscle in flap design has historically been viewed as protective toward postoperative infection given a robust blood supply compared to fasciocutaneous flaps[6]. Other advantages of muscle flaps include the ability to eliminate dead space with vascularized tissue; however, muscle flaps can be associated with donor site morbidity and flap bulk.
While advances in microsurgical technique have allowed surgeons to utilize free flaps for soft tissue coverage, distal lower extremity trauma is often too small to sensibly utilize free flaps but too large to close primarily. Considerations of flap design include patient factors (medical comorbidities, surgical risk, current adjuvant therapy), local factors (injury location, injury severity, associated fractures, tissue quality, previous surgical sites), and flap factors (color, texture, surface area, volume, pedicle length, arc of rotation)[7]. Therefore, careful deliberation is vital when planning for traumatic reconstruction.
The soleus flap is known to be an optimal flap for the middle- and lower-third of the leg[8]. Its primary vascular pedicles include the popliteal artery and branches of both the posterior tibial (medial belly) and peroneal arteries (lateral belly)[5,9]. As a consequence of its dual blood supply, the soleus flap can advantageously be split longitudinally into a hemisoleus flap with an improved rotational arc[10]. However, soleus muscle harvest has been associated with decreased ankle flexion and impaired venous return[11]. Despite these risks, soleus muscle flaps have traditionally been a reliable tool in the plastic surgeon’s armamentarium for traumatic lower extremity reconstruction and should not be overlooked in the modern era of free flaps. The purpose of this study is to evaluate the trends and outcomes of soleus flap reconstruction after lower extremity injury in a large cohort at a Level 1 trauma center.
METHODS
This is an Institutional Review Board approved retrospective chart review using a prospectively maintained database at the Los Angeles County + University of Southern California (LAC + USC) Medical Center from 2007 to 2021. Inclusion criteria were as follows: (1) patients 18 years of age or older; (2) definitive soft tissue coverage by soleus muscle flap; (3) operation conducted by the Plastic and Reconstructive Surgery (PRS) service at LAC + USC; and (4) available follow-up records of postoperative outcomes of the lower extremity.
Chart review was performed by four separate reviewers (CJ, IR, JB, KK) across electronic medical records (EMR) and paper charts. Patient demographics, body mass index (BMI), medical comorbidities, mechanism of injury (MOI), wound location, Gustilo-Anderson (GA) fracture classification, and flap characteristics were reviewed and analyzed. Primary outcomes of interest included flap complications, including flap revision, flap necrosis, and flap loss. Secondary outcomes included infection rates, limb amputation, ambulatory status, and duration until final ambulation. Ambulatory status was defined as either walking unassisted, using an assistance device (i.e., walker, crutches, or cane), wheelchair, or limb amputation. Time until final ambulation was calculated as the difference between the date of flap placement and the earliest date of the highest level of ambulation, which was abstracted from any note in the medical record specifying the patient’s highest ambulation.
SPSS Statistics 28.0 was used to analyze differences in patient demographics, injury characteristics, postoperative complications, and ambulatory status. Descriptive statistical analysis for demographic data included the means and standard deviations. Student's t-test was used to compare continuous variables, and chi-square was used to analyze categorical data. P-values were reported as two-tailed and were indicated as statistically significant if the alpha (α) value was less than or equal to 0.05.
RESULTS
In our single-institution review of microsurgical reconstruction, 187 lower extremity local flaps were placed, 68 (36.4%) of which were soleus muscle flaps. Only 16% of soleus flaps (n = 11) were performed after 2015.
Demographics
The average age was 39.4 years old (SD: 16.2) and the average BMI was 27.8 kg/m2 (SD: 5.3) across 63 (92.6%) males and five (7.4%) females. The most common comorbidity was tobacco usage (n = 36; 52.9%), followed by hypertension (n = 17; 25.0%), and diabetes mellitus (n = 11; 16.2%); 44 patients (64.7%)
Patient demographics
| n (%) | ||
| Total number of patients | 68 | |
| Mean age (years) | 39.4 ± 16.2 | |
| Average BMI (kg/m2) | 27.8 ± 5.3 | |
| Obese (BMI > 30) | 18 (26.1%) | |
| Not obese (BMI < 30) | 50 (72.5%) | |
| Sex | ||
| Male | 63 (92.6%) | |
| Female | 5 (7.4%) | |
| Comorbidities | ||
| ≥ 1 comorbidity | 44 (64.7%) | |
| Tobacco | 36 (52.9%) | |
| Illicit drug use | 19 (27.9%) | |
| Hypertension | 17 (25.0%) | |
| Diabetes mellitus | 11 (16.2%) | |
| Coronary artery disease | 3 (4.4%) | |
Injury & flap characteristics
The most common MOI warranting reconstruction was auto versus pedestrian (n = 34; 49.3%), followed by motorcycle collisions (n = 7; 10.1%), gunshot wounds (n = 5; 7.2%), and falls (n =5; 7.2%). Wound severity was classified by the Gustilo-Anderson (GA) classification system for open fractures. Open fractures were diagnosed in 56 patients, with GA fracture IIIB (n = 35; 50.7%) seen in over half of these patients, GA type II occurring in 18 patients (26.1%), and GA type IIIC occurring in two patients (2.9%). Soleus flaps were predominantly placed on middle-third leg wounds (69.6%) followed by distal-third injuries (32.4%) [Table 2]; only one hemisoleus flap was placed, and no cross-leg free flaps were performed. Of note, a significantly larger percentage of patients (53.6%) with high severity injuries (i.e., GA type IIIA-C) suffered middle-third leg wounds (P = 0.009).
Injury & flap characteristics
| n (%) | |||
| Mechanism of injury | |||
| Auto versus pedestrian (AVP) | 34 (49.3%) | ||
| Motorcycle crash (MCC) | 7 (10.1%) | ||
| Other | 7 (10.1%) | ||
| Gunshot wound (GSW) | 5 (7.2%) | ||
| Falls | 5 (7.2%) | ||
| Auto versus stationary body | 4 (5.9%) | ||
| Motor vehicle collision (MVC) | 4 (5.9%) | ||
| Crush | 2 (2.9%) | ||
| Soft tissue coverage | |||
| Middle 1/3 only | 40 (58.8%) | ||
| Distal 1/3 only | 15 (22.1%) | ||
| Middle 1/3 + distal 1/3 | 5 (7.4%) | ||
| Proximal 1/3 only | 5 (7.4%) | ||
| Proximal 1/3 + middle 1/3 | 1 (1.5%) | ||
| Proximal 1/3 + distal 1/3 | 1 (1.5%) | ||
| Proximal 1/3 + middle 1/3 + distal 1/3 | 1 (1.5%) | ||
| Fractures | |||
| Fracture location | (n = 63) | ||
| Middle 1/3 of tibia | 41 (65.1%) | ||
| Middle 1/3 of fibula | 22 (34.9%) | ||
| Distal 1/3 of tibia | 19 (30.2%) | ||
| Proximal 1/3 of fibula | 15 (23.8%) | ||
| Distal 1/3 of fibula | 10 (15.9%) | ||
| Proximal 1/3 of tibia | 7 (11.0%) | ||
| Tibial plateau | 3 (4.8%) | ||
| Calcaneus | 2 (3.2%) | ||
| Gustilo-Anderson type | (n = 56) | ||
| Type IIIB | 35 (50.7%) | ||
| Type II | 18 (26.1%) | ||
| Type IIIC | 2 (2.9%) | ||
| Type I | 1 (1.4%) | ||
The most commonly fractured bone was the tibia, occurring in 62 of 63 patients (98.4%) with fractures, with middle-third fractures being the most common fracture location (66.1%). Multiple concurrent unilateral fractures were seen in the majority of patients, with the most common combinations being the middle-third tibia/fibula (n = 17) followed by fracture of the distal-third tibia/fibula (n = 9). Eighteen patients suffered multiple remote fractures, including contralateral lower extremity (n = 10), upper extremity (n = 9) and pelvis (n = 7).
In certain cases, the soleus flap was combined with the medial gastrocnemius flap (n = 3), lateral gastrocnemius flap (n = 1), vastus lateralis flap (n = 1), and anterolateral thigh flap (n = 1). Skin grafts were employed in 67 patients (98.5%). Of note, eight patients (11.8%) suffered from arterial injuries.
Complications & long-term functional outcomes
Regarding postoperative complications, twelve patients (17.6%) suffered hardware infections (n = 2) and/or osteomyelitis (n = 11) [Table 3]. Among these twelve patients, ten smoked tobacco, six endorsed illicit substance use, four had hypertension, two had diabetes mellitus, and one had obstructive sleep apnea. One patient with osteomyelitis required a below-the-knee amputation (BKA); notably, this patient suffered a GA IIIB injury. Of these 12 patients, there were four concurrent upper extremity fractures and two concurrent contralateral lower extremity fractures (n = 4). No statistical significance was found between high severity fractures (GA type IIIA-C) and postoperative infection rate. Similarly, no significance was identified between diabetes mellitus or > 1 comorbidity and infectious complications.
Postoperative outcomes & complications
| n (%) | ||
| Flap complications | ||
| Any postoperative complication | 18 (26.1%) | |
| Any infection | 12 (17.6%) | |
| Osteomyelitis | 11 (15.9%) | |
| Flap revision | 6 (8.7%) | |
| Amputation | 2 (2.9%) | |
| Hardware infection | 2 (2.9%) | |
| Partial flap loss | 2 (2.9%) | |
| Flap loss | 0 (0.0%) | |
| Ambulation status* | ||
| Fully ambulatory | 24 (35.3%) | |
| Assistance device | 24 (35.3%) | |
| Wheelchair | 20 (29.4%) | |
Six patients (8.8%) required flap revision and two (2.9%) experienced partial flap loss [Table 3]; notably, six of these patients smoked tobacco. Three of the patients who needed flap revision developed osteomyelitis, one of which also had a hardware infection. Of the eight patients who suffered arterial injuries, two required flap revisions, and one necessitated an above-the-knee amputation (AKA); of note, the latter patient suffered a GA IIIC injury. There was 100% flap survival at the most recent clinic follow-up.
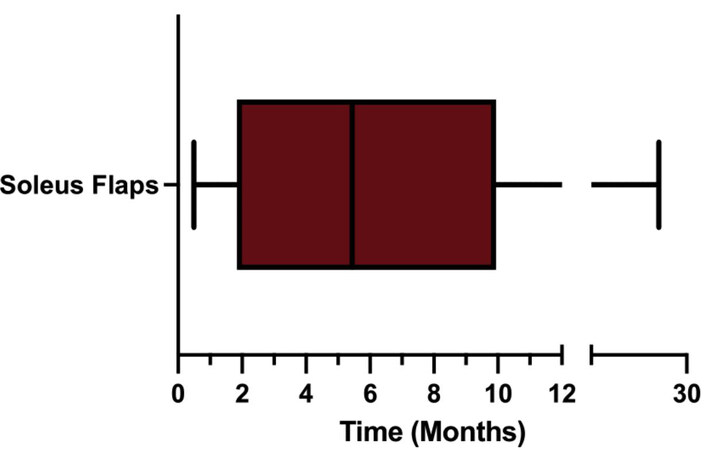
The mean follow-up time from discharge date to latest follow-up with the PRS team was 3.7 months (SD: 6.8). Of the patients with documented follow-up, 35.3% of patients (n = 24) were independently ambulatory after an average of 7.5 months (SD: 7.2) [Figure 1]. Twenty-four patients used a walking assistance device (walker or cane) at the most recent follow-up, and twenty patients were wheelchair-dependent [Table 3].
DISCUSSION
An interesting trend identified in our review was 84% of soleus flaps were placed prior to 2016, with all patients who received soleus flaps for isolated proximal-third leg injuries occurring prior to 2016. With the increased use of locally-based perforator flaps[12], there appears to be less reliance on the aforementioned workhorse flap; however, it should not be overlooked as a reliable flap option for wounds involving the middle-third leg, as demonstrated by 0% flap loss. The muscle bulk recruited during flap elevation is well contoured for tibial coverage, providing added aesthetic benefit[5] for these injuries. Additionally, the soleus flap is a relatively simple and safe alternative to more complex microsurgical reconstruction with free flap placement[12]. Per operative dictation, indications for soleus flap placement were commonly weighed against free flap placement; however, wound size, ability to approximate the defect, surrounding tissue quality, and arc of rotation of the muscle belly prompted soleus flap selection. Reflective of the literature, soleus flaps were mostly selected for wounds involving the middle- and distal-third leg.
The robust nature of the soleus flap is exemplified by 0% flap loss in our cohort, in which most patients endorsed comorbidities unfavorable to a free flap, namely tobacco use. Our cohort demonstrated a higher than expected incidence of overall infectious complications (17.6%); additionally, a significantly higher percentage of smokers developed infectious complications (83.3%, P = 0.017), which is reflective of the literature suggesting that smoking increases infectious complications in plastic surgery patients[13,14]. Furthermore, 66.7% of patients who required flap revisions smoked tobacco - a known vasoconstrictor and deterrent to wound healing[15]. Interestingly, in our study, high severity GA fracture classification was not significantly correlated with infection (P = 0.304), despite 56 patients having open lower extremity fractures and GA fracture classification being a strong predictor of deep infections[16]. However, our cohort demonstrated that significantly more patients with high-grade GA injuries suffered middle-third leg wounds (P = 0.009), prompting soleus flap allocation.
Four of the twelve (33.3%) patients who suffered infectious complications had concurrent remote fractures, likely reflective of higher impact MOI, and, subsequently, a higher likelihood of infection based on increased injury severity. GA can be used as a surrogate for injury severity[16,17]; notably, our data did not demonstrate significance between GA classification and the need for flap revision (P = 0.599), possibly reflective of a small number of revisions (8.7%); notably, four of six patients requiring revision had GA type II fractures. Studies have shown higher-grade injuries associated with a greater risk of complications; notably, GA type III injuries are often associated with higher amputation rates and delayed revascularization as they commonly result from blunt and high-velocity trauma[17,18]. Similarly, among the two patients who suffered from type IIIC injuries, both patients had arterial injuries and one patient required an amputation. In such high severity open fractures, flap coverage and bony union can improve the likelihood of achieving full ambulation by six months postoperatively[18].
Eight patients suffered arterial injuries, two of which required revisional surgery. One of these eight patients required an AKA after suffering a significant injury with a GA type IIIC open fracture, arterial and nerve injuries, two unilateral leg fractures, and two remote fractures, with a history of hypertension and use of two illicit substances. All these factors increased the likelihood of complications with limb salvage and ultimately resulted in amputation. As mentioned previously, the clinically grave picture preoperatively reflected the severity of the injury and strongly influenced the outcome. It is important to note that a preoperative angiogram may be of added benefit[5], especially in the setting of severe trauma, to confirm the patency of major perforators when considering flap design. Free tissue transfer should be considered as a final reconstructive option for larger wounds in the middle- or distal-third leg or those involving trauma to the soleus or its perforators[5].
Donor site morbidity is a considerable outcome involved in flap harvest. Although muscle flaps are reported as imparting an acceptable functional outcome in the literature, a potential unknown ambulatory morbidity is associated with this option, is variable across patients, and may be reflective of the injury itself. This notion might be reflective of the increase in pedicled perforator flaps[12] and reflective of our surgical trend in which 16% of soleus flaps were placed after 2015. However, given severe tissue disruption in traumatic injuries, pedicled fasciocutaneous perforator flaps may be of limited use in such situations, thereby supporting the versatile soleus muscle flap[12]. Following the transfer of the soleus muscle, Knopp et al.[19] used isokinetic testing three years postoperatively and found a mean reduction in muscle-strength flexion of 30%. While it has been reported that functional donor site morbidity is mild in patients who had a complete recovery from the index trauma, patients can still demonstrate deficits and compensatory motions during more challenging activities (i.e., fast/uphill walking)[20]. Further research should focus on flap type and its correlation with long-term ambulation.
This study was limited in focus to soleus flaps alone and commented explicitly on the location of soleus flap placement and outcomes. Our group has parallel publications examining flap choice based on wound location as well as local versus free flap implementation; however, the aim of this particular study was to describe the trends and outcomes of soleus flap usage at a large Level 1 trauma center. One of the limitations of this study is the variability in outpatient follow-up; fifteen patients had no long-term follow-up after discharge. While the mean follow-up time from discharge date to latest follow-up with PRS was 3.7 months (SD: 6.8), the average date of highest ambulation across the whole cohort was 5.4 ± 9.8 postoperatively. The average time to ambulation for those who achieved fully independent ambulation was 7.5 months (SD: 7.2). Additionally, the duration of time until final ambulation was reached may be higher than we report since patients are more likely to return for follow-up when experiencing postoperative complications or requiring a medical device that helps them ambulate. In contrast, fully ambulatory patients are less likely to follow up, and the exact date of final ambulation may be unknown. Future studies could implement more frequent follow-ups through phone or telehealth visits. Other limitations include patient loss to follow-up and possible errors that could have occurred during the crossover between EMR and paper charts, providing mixed difficulty across chart reviews with a certain paucity of data.
In conclusion, this study examines outcomes of over 15 years of experience with lower extremity reconstruction employing soleus flaps at a Level 1 trauma center. Although the flap loss rate in this cohort was 0%, the findings demonstrate higher than expected infectious complications. Additionally, our results reveal only 16% of soleus flaps were performed at our institution after 2015. As surgeons consider the reconstructive ladder for lower extremity trauma, a rotational soleus muscle flap should not be overlooked in the modern era of free flap tissue transfers and might be a more optimal flap choice in certain patients with multiple comorbidities. Future studies should evaluate the difference in functional and aesthetic outcomes based on flap type and evaluate the impact of patient comorbidities and demographics on wound healing and ambulation.
DECLARATIONS
Authors’ contributionsAssisted with study concept and design: Roohani I, Kondra K, Carey J
Acquired, analyzed, or interpreted the data: Roohani I, Kondra K, Jimenez C, Stanton E, Becerra J
Drafted the manuscript: Kondra K, Jimenez C, Stanton E, Roohani I
Provided critical revision of the manuscript for important intellectual content: Kondra K, Carey J
Calculated statistical analysis: Roohani I, Jimenez C, Stanton E
Provided administrative, technical, or material support: Carey J
Supervised study: Carey J
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateThis is an Institutional Review Board approved retrospective chart review using a prospectively maintained database at the Los Angeles County + University of Southern California (LAC + USC) Medical Center from 2007 to 2021 (ethical number: HS-16-00314).
Consent for publicationNot applicable.
Copyright© The Author(s) 2022.
REFERENCES
2. Yaremchuk MJ, Manson PN. Local and free flap donor sites for lower-extremity reconstruction. Lower extremity salvage and reconstruction: orthopedic and plastic surgical management. New York: Elsevier 1989:117-57. Available from: https://www.amazon.com/Lower-Extremity-Salvage-Reconstruction-Orthopaedic/dp/0444013334 [Last accessed on 1 Apr 2022].
3. Grotting JC, Vasconez LO. Regional blood supply and the selection of flaps for reconstruction. Clin Plast Surg 1986;13:581-93.
4. Parrett BM, Matros E, Pribaz JJ, Orgill DP. Lower extremity trauma: trends in the management of soft-tissue reconstruction of open tibia-fibula fractures. Plast Reconstr Surg 2006;117:1315-22; discussion 1323.
5. Song P, Pu LLQ. The Soleus Muscle Flap: An overview of its clinical applications for lower extremity reconstruction. Ann Plast Surg 2018;81:S109-16.
6. Gosain A, Chang N, Mathes S, Hunt TK, Vasconez L. A study of the relationship between blood flow and bacterial inoculation in musculocutaneous and fasciocutaneous flaps. Plast Reconstr Surg 1990;86:1152-62; discussion 1163. PMID: 2243859.
7. Janis JE. Essentials of plastic surgery. CRC Press; 2014. Available from: https://www.amazon.com/Essentials-Plastic-Surgery-Second-Jeffrey/dp/1576263851 [Last accessed on 1 Apr 2022].
8. AlMugaren FM, Pak CJ, Suh HP, Hong JP. Best local flaps for lower extremity reconstruction. Plast Reconstr Surg Glob Open 2020;8:e2774.
9. Reddy V, Stevenson TR. MOC-PS(SM) CME article: lower extremity reconstruction. plastic and reconstructive surgery 2008;121:1-7.
11. Azoury SC, Levin LS, FACS, Bauder AR, Kovach SJ. Flap reconstruction of the lower extremity. Available from: https://www.uptodate.com/contents/flap-reconstruction-of-the-lower-extremity [Last accessed on 1 Apr 2022].
12. Quaba O, Quaba A. Pedicled perforator flaps for the lower limb. Seminars in Plastic Surgery 2006;20:103-11.
13. Spear SL, Ducic I, Cuoco F, Hannan C. The effect of smoking on flap and donor-site complications in pedicled TRAM breast reconstruction. Plast Reconstr Surg 2005;116:1873-80.
14. Pluvy I, Panouillères M, Garrido I, et al. Smoking and plastic surgery, part II. Clinical implications: a systematic review with meta-analysis. Ann Chir Plast Esthet 2015;60:e15-49.
15. Sørensen LT. Wound healing and infection in surgery: the pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: a systematic review. Ann Surg 2012;255:1069-79.
16. Thakore RV, Francois EL, Nwosu SK, et al. The Gustilo-Anderson classification system as predictor of nonunion and infection in open tibia fractures. Eur J Trauma Emerg Surg 2017;43:651-6.
17. Kim PH, Leopold SS. In brief: Gustilo-Anderson classification. [corrected]. Clin Orthop Relat Res 2012;470:3270-4.
18. Kohlprath R, Assal M, Uçkay I, et al. Open fractures of the tibia in the adult: surgical treatment and complications. Rev Med Suisse 2011;7:2482, 2484-8. PMID: 22288287.
19. Knopp W, Buchholz J, Muhr G, Steinau HU. Negative effects of local tibial muscle flap repair on foot function. Unfallchirurg 1993;96:229-34.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Kondra K, Jimenez C, Stanton E, Roohani I, Becerra J, Carey J. Soleus muscle flap for reconstruction of lower extremity trauma. Workhorse or glue factory?. Plast Aesthet Res 2022;9:36. http://dx.doi.org/10.20517/2347-9264.2021.121
AMA Style
Kondra K, Jimenez C, Stanton E, Roohani I, Becerra J, Carey J. Soleus muscle flap for reconstruction of lower extremity trauma. Workhorse or glue factory?. Plastic and Aesthetic Research. 2022; 9(5): 36. http://dx.doi.org/10.20517/2347-9264.2021.121
Chicago/Turabian Style
Kondra, Katelyn, Christian Jimenez, Eloise Stanton, Idean Roohani, Jake Becerra, Joseph Carey. 2022. "Soleus muscle flap for reconstruction of lower extremity trauma. Workhorse or glue factory?" Plastic and Aesthetic Research. 9, no.5: 36. http://dx.doi.org/10.20517/2347-9264.2021.121
ACS Style
Kondra, K.; Jimenez C.; Stanton E.; Roohani I.; Becerra J.; Carey J. Soleus muscle flap for reconstruction of lower extremity trauma. Workhorse or glue factory?. Plast. Aesthet. Res. 2022, 9, 36. http://dx.doi.org/10.20517/2347-9264.2021.121
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 20 clicks
Cite This Article 20 clicks












Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.