Combined grafts and flaps in urethral stricture repair
Abstract
Although urethral strictures have been known since antiquity, the surgical management of urethral strictures has undergone a great (re)evolution over the last six decades, both in the perception of the disease and in the surgical repair techniques, always presenting itself as a challenge for the surgeon and patient. Reconstruction of urethral stricture disease involving a combination of grafts and flaps consists of a group of complex procedures with specific clinical indications. The knowledge of these procedures by reconstructive urologists is both necessary and relevant. A thorough understanding of the anatomy, including blood supply, is a crucial proviso for the correct evaluation and successful management of urethral stricture disease. We discuss the main techniques and indications in combined graft and flap urethroplasties.
Keywords
INTRODUCTION
Urethral reconstruction is complex with a significant learning curve if the best outcomes are desired[1]. Several “principles” have been implemented and accepted to best cope with distinct surgical possibilities. The obliterative pattern of a urethral segment involves the full circumference of the corpus spongiosum, thereby only preserving a limited urethral plate and a hostile ground for a comfortable and straightforward urethroplasty.
The vast majority of urethral strictures can be managed with a single surgical procedure using grafts, flaps, or excision and primary anastomosis[2]. In the presence of an extensive and fully circumferential injury of the urethral plate segment, these resources may be insufficient, and a standard staged urethroplasty is the option of choice. A staged urethroplasty creates a hypospadic meatus for a least six months and will require at least one additional intervention to complete the urethral reconstruction. Staged urethroplasty is usually performed with skin flaps or buccal mucosa graft to correct complex hypospadias.
The combination of graft and a flap is an alternative way to reconstruct these complex obliterative urethral lesions. This option is less commonly used, but it must be part of the reconstructive urologist’s armamentarium. The literature is lacking in regards to the combined use of grafts and flaps. Of those published, all are related to hypospadias cripple or some form of obliterative penile pathology[3]. We present a review of this complex reconstruction with indications and techniques.
PRINCIPLES OF TISSUE TRANSFER TECHNIQUES
When performing a graft, flap, or combination technique, important principles must be kept in mind for the selection of the surgical procedure. The tissue must be hairless, have the ability to adapt to a new environment, and preferentially present a good aesthetic result[4-5].
Vascular anatomy of the penis and urethra
A thorough understanding of the anatomy and vascularization of the penis and urethra is essential to choose the best surgical procedure with a decrease in complications or unwanted results. Additionally, penile cutaneous flaps utilized in urethroplasty are “axial” (based on a specific feeding vessel) and “island” (completely separated from the skin from which it is lifted); they are only attached by and dependent on the pedicle, which carries the blood supply to the skin island.
The urethra has two principal sources of arterial blood supply, allowing for extensive dissection, mobilization, and division without generating ischemic injury. Arterial blood supply to the urethra and corpus spongiosum follows both antegrade and retrograde patterns. It originates from the bulbar and dorsal arteries, which derive from the common penile arteries. The common penile arteries, in turn, arise from the internal pudendal artery. The common penile artery then divides into the bulbar, urethral, and dorsal arteries. Together, the bulbar arteries supply antegrade flow to the urethra and corpus spongiosum, while the dorsal arteries vascularize the glans.
A venous plexus exists in the glans, the most distal segment of the corpus spongiosum. This plexus merges with three main venous branches. The periurethral vein courses within the corpus spongiosum and arborizes with the deep dorsal vein through numerous circumflex veins that circle both corpora cavernosa. As these veins progress further proximally, they merge at Santorini’s plexus just proximal to the symphysis pubis, alongside the prostate on each side[6].
Graft and flap materials and their characteristics
Types of grafts and graft techniques
Many grafts have been used in urethral reconstruction, including oral mucosa, lingual mucosa, penile skin, tunica vaginalis, bladder mucosa, colonic mucosa, and acellular grafts including porcine small intestinal submucosa and tissue-engineered material[7,8]. An oral mucosal graft (OMG) urethroplasty is currently the gold standard for substitution urethroplasty[9,10]. Several factors were responsible for the acceptance of OMGs as the best urethral substitute, including ready availability and easy manipulation, resistance to infection, affinity for a humid environment, a thick epithelium and a thin lamina propria, quick inosculation, and superior medium-term outcomes, which are equivalent to full-thickness cutaneous grafts[10].
Several techniques have been described, each with its own peculiarities. However, there are few comparative studies. There are three different approaches to the onlay augmentation technique: ventral, dorsal, and dorsolateral. The ventral route has the theoretical advantage of being faster and without the need for urethral dissection[11]. However, it needs to be located proximally to the anterior urethra, in the bulbar urethra. The dorsal route has the advantage of leaving the graft well fixed to the corpus cavernosum, eventually allowing better graft take[6]. The dorsolateral approach is an attempt to provide an alternative to the other two approaches.
Types of flaps and flap techniques
The ideal flap should be: (1) hairless; (2) accustomed to a wet environment; (3) versatile; (4) cosmetically appealing; and (5) produce minimal donor site morbidity[12]. These characteristics provide a good adaptation of the flap when it is incorporated into the urethra, ensuring good caliber and fluidity for urine transport.
Historically, several flaps were commonly utilized in penile urethroplasty. Until the widespread utilization of penile cutaneous flaps and OMGs as techniques of choice, scrotal flaps were popular options. Despite the historical importance of these scrotal flaps, the incorporation of hair-bearing skin into the urethra led to unacceptable long-term outcomes due to stones and infections[12]. Other flaps which were non-hair-bearing, including thigh skin, had shorter pedicles and, therefore, were not appropriate for penile urethroplasty[12]. However, for urethral fistula closure and reconstruction with interpositions layers in combination with grafting, the use of non-cutaneous pedicled rotational flaps (i.e., gracilis muscle) continues to be actively used and investigated[13].
PATIENT SELECTION AND SELECTION OF THE RIGHT TECHNIQUE
The preoperative evaluation of the patient is essential before deciding on the smallest procedure to be performed. For this purpose, the patient must be considered as a whole, including age and comorbidities, as they can interfere with both intraoperative and postoperative periods. These comorbidities, such as smoking, the patient’s ability to be in lithotomy, previous surgeries, and diabetes mellitus, among others, may impact on peripheral blood supply and compromise effective healing and surgical success[10]. Another fundamental aspect when selecting the surgical incision site is the evaluation of the skin and tissues, always taking into consideration the care that the patient should have postoperatively[14,15].
Physical examination to assess the integrity of the penile/genital skin and concomitant wounds, fistulas, or abscesses is also important in selecting the proper locations for flaps and grafts. The use of skin affected by lichen sclerosus (LS) should not be advised for urethral reconstruction. Currently, there is a high tendency to use oral mucosa graft, causing flaps to lose popularity as a conventional reconstructive option[3,6,8,9,14,15].
COMBINED TISSUE TRANSFER
The combined tissue transfer is an option for severe urethral stricture or congenital penile anomalies. The concepts mainly consist in a graft dorsally fixed on the penis covered by a pedicled penile skin flap.
To the glans and fossa navicularis
The management of strictures affecting the distal penile urethra, including external meatus and fossa navicularis (FN), has long constituted a difficult task for both general and reconstructive urologists. The therapeutic goal for surgical reconstruction of these strictures is two-fold: (1) to create a patent distal urethra; and, simultaneously; (2) to yield an aesthetically pleasing outcome. The implementation of a standard reconstructive procedure for strictures of the distal penile urethra is usually compromised by three important obstacles: (1) these strictures are difficult to evaluate by imaging studies; (2) they are difficult to diagnose; and (3) they are difficult to treat. As with most urologic reconstructive procedures, the evaluation of both operative and patient-reported outcomes by randomized trials is mostly inexistant. Therefore, data favoring one technique over another are, to a certain extent, based on and obtained from prospectively gathered, but retrospectively delineated, observational series. In this review, the evolution and treatment of distal penile urethral strictures are discussed with a special focus on tissue transfer, in either isolated or combined fashion.
The selection of the most appropriate technique to reconstruct distal urethral strictures depends significantly on stricture etiology. In turn, the most frequent causes of these strictures have altered dramatically in the last 30 years. In the past, infectious urethritis, such as sexually transmitted diseases, was predominant. However, contemporary series in the industrialized world report iatrogenic etiologies, such as traumatic urethral catheterizations or transurethral procedures, and LS[16-18]. Distal and FN strictures correspond to 18% of all strictures of the anterior urethra[17].
Several therapeutic options may be useful to create urethral patency and simultaneously preserve satisfactory penile cosmesis. Due to the challenges imposed by these two functional issues, an algorithmic approach has been recommended. In short strictures that are limited to the external meatus only, a simple meatotomy, or urethral dilatation, may be the procedure of choice. However, these options require repeated intervention in the short term and are often considered palliative. Therefore, because they are considered palliative, they should be attempted only once. Endoscopic urethrotomy using a cold knife or laser has not produced efficacious results in a consistent fashion[19-20]. However, most distal strictures tend to extend proximally. Endoscopic urethrotomy for distal urethral strictures was associated with notably lower efficacy compared to bulbar urethra (16% vs. 42%)[19]. Although very popular due to their simplicity and minimally invasiveness, both urethral dilatation and endoscopic urethrotomy are linked to high failure rates, thereby leading to recurrent interventions, and therefore should not be recommended in complex distal urethral strictures.
Traditionally, open distal urethroplasty has been reserved for the longest strictures that involve the external meatus and FN, or for recurrent or obliterative cases. Reconstructive approaches have included grafts, flaps, or combined use of both, including several variations in technique. A single-stage penile skin flap procedure can often be utilized for these strictures if not due to LS. If previous penile flap surgery has been attempted or in the presence of LS, a staged reconstruction with oral mucosa grafting (as dorsal onlay or inlay) is more advisable, as using skin in these cases is associated with high recurrence rates[21-22]. Multiple flap procedures have been reported for the surgical reconstruction of distal strictures of the penile urethra.
Flaps
Flap urethroplasty for distal penile strictures was first described more than 50 years ago. Originally, tubularized or advancement flaps were the local penile flaps described, and these were tormented by severe problems, such as flap necrosis, flap contraction, penile ventral curvature, penile rotation, or deformities of the external meatus. In 1987, Jordan introduced the ventral transverse fasciocutaneous island flap[23]. This cutaneous island flap is based and lifted on a broad pedicle of dartos fascia and is designed transversally on the ventral skin of the penis. In this technique, a well-vascularized fasciocutaneous distal transverse ventral skin flap is prepared and sutured to the ventral urethra [Figure 1]. Glans wings are raised and reapproximated over the flap. Only minimal advancement of the flap is needed, making the final cosmetic appearance highly gratifying. Long-term stricture free rates after this technique were 83% with a mean follow-up of 10.3 years[22]. In 1998, Armenakas and McAninch reported a modification of the previous technique to mitigate potential complications of glans dehiscence that utilized a similar ventral transverse skin flap but with preservation of the glans and elevation of the glans off the urethra [Figure 2][24]. The authors reported a stricture-free rate of 94% at a mean follow-up of 43 months. Globally, patients were very pleased with the cosmetic outcome. McAninch and Morey[25] also adapted this concept to complex, long urethral strictures extending from the FN to the proximal penile urethra. Based on a modification of the original technique, they utilized a circumferential penile fasciocutaneous flap for long anterior urethral strictures spanning up to 15 cm. They initially reported 79% successful results. Asserting that the total length of FN stricture disease is a predictor for restricture, Virasoro et al.[22] stratified FN strictures into two groups, those < 2.5 cm and those > 2.5 cm, finding a statistical difference in terms of restricture in the longer stricture cohort The use of local genital cutaneous flaps was strongly discouraged in the presence of LS, which was associated with a 50% higher risk of restricture at the flap location in their series.
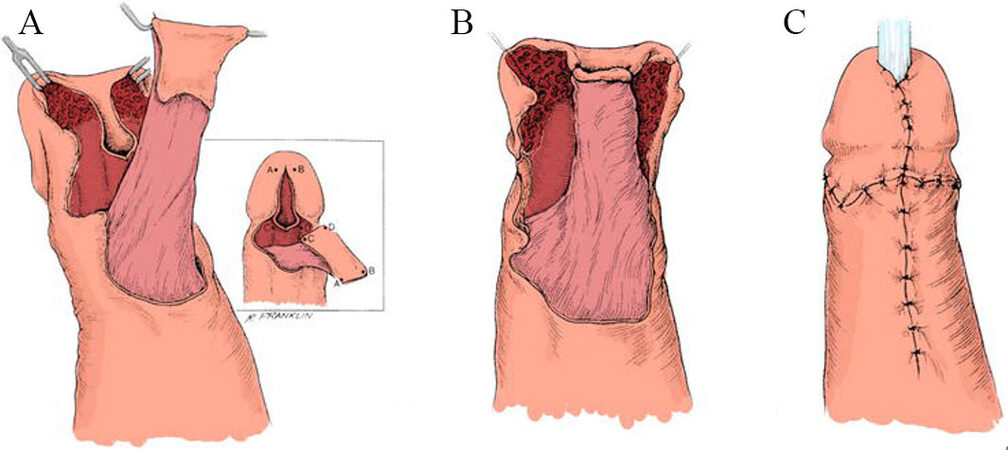
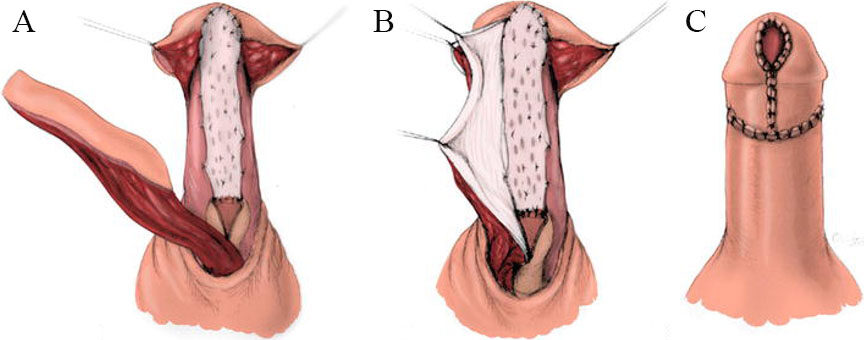
Figure 1. Schematic illustration of Jordan’s ventral transverse skin island flap procedure. (A-C) After urethrotomy is made until normal urethra, a ventral skin island flap is elevated above Buck’s fascia, and the lateral glans wings are exposed. The skin island is rotated, transposed, and inverted into the urethrotomy defect. The glans wings are sutured ventrally. The inset shows details of the rotation, transposition, and inversion of the flap (from Jordan GH[23]).
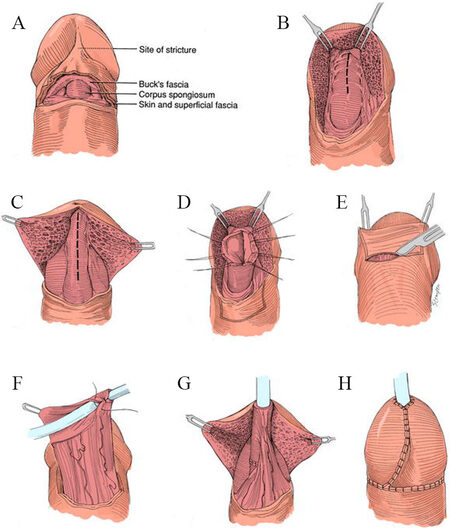
Figure 2. Fasciocutaneous distal penile flap urethroplasty as described by McAninch. (A-H) Urethral exposure followed by ventral longitudinal urethrotomy. The fossa navicularis is exposed with either a glans-cap or a glans-wings technique. A fasciocutaneous distal, transverse, ventral penile flap is developed. The urethral stricture can be corrected by either a ventral onlay or a neourethral tube. The glans wings or cap is sutured to cover the flap reconstruction (from Armenakas and McAninch[24]).
Grafts
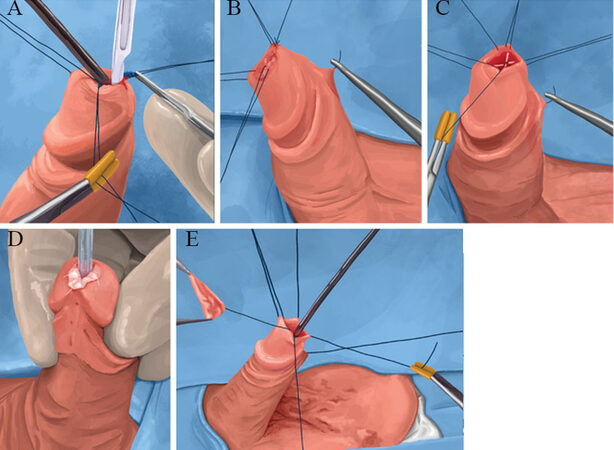
Grafting procedures for distal penile strictures are deemed more flexible than flap procedures. Grafts can be employed in inflammatory strictures, especially LS that discourages the use of penoscrotal cutaneous flaps. Venn and Mundy[26] compared the results between a single-stage penile skin flap urethroplasty and a traditional staged graft (posterior auricular skin or oral mucosa) urethroplasty in patients with LS. Patients treated with skin flap urethroplasty had a 100% recurrence rate at a mean follow-up of five years compared to 8.3% recurrence of those who had a graft. These findings led them to infer that genital skin that is affected by LS must be avoided in urethral reconstruction. Depasquale et al.[21] also published a 90% long-term restricture rate in LS patients who underwent staged urethral reconstruction with genital skin grafting as opposed to 0% recurrence in those who received an OMG. In 1998, Naudé[27] initiated the concept of endoscopic graft urethroplasty. A few modifications were published later[28-29]. Unfortunately, these procedures did not gain popularity due to intrinsic technical complexity and problems with surgical reconstruction of distal penile strictures. The main advantage of this concept of intraurethral urethroplasty over open procedures is to avoid skin incisions and glans elevation with spatulation. Open procedures are intrinsically associated with cosmetic and functional complications, including infection, dehiscence, and fistula. In 2008, Seth et al.[29] reported a hybrid technique of intraurethral approach to distal urethral stricture combining a transurethral graft placement with a ventral subcoronal incision to promote better scar removal and proximal graft anastomosis. At a mean follow-up of 38 months, an 84% success rate was reported. In 2016, Nikolavsky et al.[30] published a new transurethral surgical technique for the reconstruction of distal penile strictures employing OMG with promising outcomes [Figures 3 and 4]. They developed this innovative and elegant reconstructive concept to avoid the drawbacks, technical complexities, and weaknesses of the previous procedures used in this urethral segment. Other advantages include avoidance of an external skin incision, preservation of the glans penis, and use of oral mucosa for grafting, thus providing both very good functional and cosmetic outcomes. This surgical technique is mainly advised for men with distal strictures due to LS, where only OMGs are recommended. At an initial follow-up of 12 months, a 93% stricture free rate was reported.
Figure 3. Transurethral ventral buccal mucosa graft inlay urethroplasty for the reconstruction of fossa navicularis and distal urethral meatus, as described by Nikolavsky.[30] (A-E) Transurethral ventral shallow resection of scar tissue. Placement of double-armed suture through buccal graft and through the apex of urethrotomy (inside out). External apical suture tying, meatal BMG edge fixation, and additional inside-out quilting of the graft with double-armed sutures (reproduced with permission from Springer Science and Business Media Dordrecht[30]).
Combined graft and flap urethroplasty
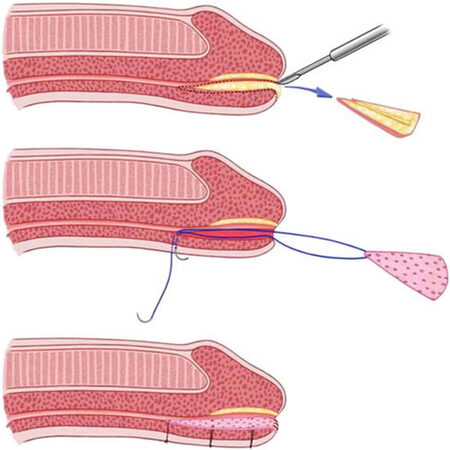
In 2011, Gelman and Sohn published a surgical technique characterized by the combined use of a dorsal onlay graft with a ventral onlay flap for a subgroup of patients with obliterated distal strictures due to ischemia, who had already failed reconstructive attempts, or with a history of hypospadias in childhood[31]. The technique was considered a combination of fasciocutaneous flap designed by Jordan with OMG. This surgical procedure is very useful in men with highly compromised urethral plates due to ischemia and dense scar formation caused by earlier surgical attempts and when a staged procedure is not favored [Figure 5]. The authors achieved a 100% success rate in a cohort of 12 patients at a 39-month follow-up. The authors concluded that this is a better approach to handling these complex strictures. A success rate of 92% was confirmed by urethroscopy four months after reconstruction with a subsequent mean follow-up of 39 months. Based on previous experiences, Djordjevic et al.[32] also used a technique that combined a dorsal longitudinal island skin flap and OMG to form a neourethra in patients with severe hypospadias. The main goal was to correct all defects in a single-stage reconstruction. They recommended this combined reconstructive approach as a good and highly successful option for neourethral reconstruction with satisfactory results in the most severe forms of hypospadias. In 2001, Morey[33] published his first experience with a similar procedure.
Figure 5. Schematic illustration of single-stage, combined flap graft technique as described by Gelman. (A-C) Oral mucosal graft is placed and quilted dorsally followed by the closure of the urethrotomy defect by a penile skin flap (from Gelman and Sohn[31]).
Staged techniques
The best application of these techniques is in men who have failed hypospadias surgical attempts, with a deficient or densely fibrotic urethral plate, or in the presence of LS. These techniques are usually regarded as more adaptable compared to flap procedures and are especially favored in the presence of LS. In 1995, Bracka initiated a modern era of staged urethral reconstruction by describing a versatile approach to difficult anterior urethral reconstructions[34]. In his procedure, the diseased urethra is completely removed, and the urethral plate is covered by an onlay graft of oral mucosa.
To the penile urethra and bulbar urethra
Dorsal graft with ventral penile skin flap
In 2001, Morey introduced the principle of augmentation urethroplasty combining OMG and penile cutaneous flap. He reported salvage of the urethral plate using a dorsal OMG combined with a flap of ventral penile skin in men with complex strictures involving the penile urethra[33]. In the initial use of this new procedure (with mean follow-up to 2.1 years), all four patients voided well and needed no further intervention. Similarly, Erickson et al.[35] described a single-stage procedure in 14 men with anterior urethral strictures using this combination of dorsal onlay OMG with a ventral fasciocutaneous flap.
The average length of the urethral strictures in his patient population was 9.75 cm with 12 (12/14; 85%) strictures found in the penobulbar segment. At a median follow-up of 2.5 years, the authors published an overall urethral patency rate of 78% (11/14 patients), although two of these patients (14%) needed an additional intraluminal maneuver to attain a fairly good urethral caliber. Individuals with longer strictures seemed to have a higher risk of restricture (12.8 cm vs. 8.7 cm). A similar experience was reported by Gelman and Sohn when applying this combination of dorsal oral graft with a ventral penile fasciocutaneous flap in distal obliterative strictures[31]. Although stricture length was not specified by the authors, various sizes of OMGs were employed (range, 2-6.5 cm) with all strictures detected in the penile urethra. All 12 patients had good urethral patency on three-month postoperative follow-up cystoscopy and all voided well at a mean 39-month follow-up.
Dorsal graft with ventral penile skin flap in proximal hypospadias surgery
Surgical reconstruction of proximal hypospadias implies rectifying different basic elements of the hypospadias complex to optimize long-term success, both functionally and cosmetically. These elements include ventral penile chordee, proximal implantation of the urethral meatus, ventral skin shortage, atypical glans morphological appearance, abnormal division of the corpus spongiosum, penile rotation, and penoscrotal transposition [Figure 6]. In some cases, there is not enough foreskin or penile skin tissue for surgery, so the choice of the technique will depend on the surgeon’s preference. Staged repairs aim at the initial rectification of ventral chordee with the fashioning of a new urethral plate using preputial/penile skin flap or OMG and followed by urethral reconstruction in the next stage[34-36]. A recently described technique by Djordjevic et al.[32] used the combination of a longitudinal dorsal island skin flap and OMG [Figure 7]. They employed this surgical procedure in children with hypospadias. Seventeen patients, aged less than two years old, received this single-stage operation for severe hypospadias (13 penoscrotal and 4 scrotal). This technique involved a combination of a dorsal OMG with a ventrally applied dorsal island penile cutaneous flap. Functional and cosmetic success was achieved in 14 patients (82%) at a mean follow-up of 25 months. Complications occurred in the remaining three patients, specifically urethral fistulation and distal urethral stricture (18%)[32].
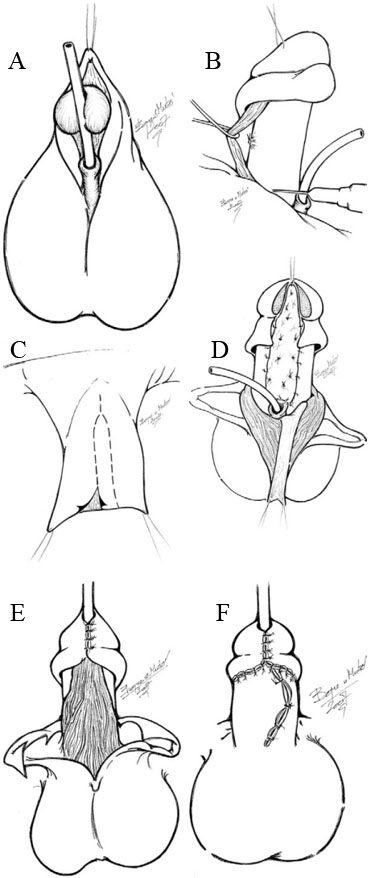
Figure 6. Diagrammatic illustration of the combined buccal mucosa graft and dorsal penile skin flap technique for pediatric hypospadias (from Djordjevic et al.[32]). A: Severe hypospadias with chordee. B: The short urethral plate is divided. Tunica albuginea is plicated dorsally to straighten the penis. C: A longitudinal skin flap is harvested from dorsal penile skin. Two lateral skin flaps will be used for penile body covering. D: The flap is buttonholed and transposed ventrally. Buccal mucosa is grafted and quilted to the tunica albuginea starting from urethral meatus up to the tip of the glans. Previously, glans was incised in the midline and its two wings were extensively mobilized. E: The flap was anastomosed with buccal mucosa graft to create neourethra. All suture lines are covered with well-vascularized subcutaneous tissue of the flap. Glans is closed without tension. F: Penile skin reconstruction is done using available penile skin.
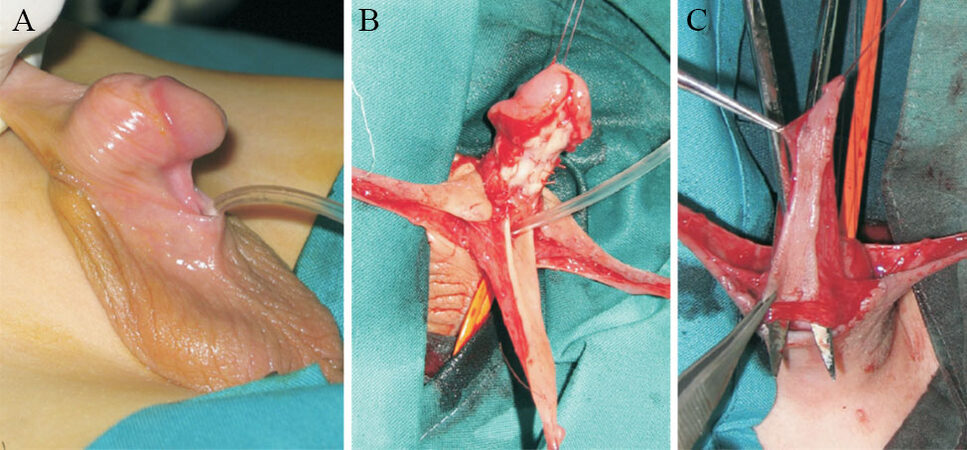
Figure 7. Scrotal hypospadias. (A) The short and undeveloped urethral plate is visible. (B) The flap is transposed ventrally. Buccal mucosa graft is fixed starting from the native urethral meatus to the tips of corporal bodies. (C) A well-vascularized island skin flap is created from the dorsal penile skin. A hole is made at the base of the flap (from Djordjevic et al.[32]).
Double graft
A double-faced dorsal plus ventral onlay urethroplasty described by Palminteri et al.[37] was applied in nearly obliterative strictures where an isolated graft would be clearly insufficient to achieve adequate lumen caliber without urethral transection. The strictured segment was opened on the ventral aspect, followed by a midline incision of the exposed dorsal urethral plate and then followed by dorsal and ventral augmentation using two OMGs[38]. In cases where a severe penile curvature was present, Djordjevic et al.[39,40] started to repair the chordee by ventral tunica albuginea incision and grafting. In patients with a penile length less than 2.5 cm, preoperative topical hormonal therapy was instituted for a period of three weeks.
CONCLUSION
The combined use of a graft, usually oral mucosa, and a genital skin flap is a safe, predictable, and long-lasting approach to single-stage reconstruction of lengthy and complex urethral stricture disease. With a proper patient selection, this combined modality proved to be a more efficient method to handle these complex stricture scenarios. This combination consists of a dorsal OMG to augment or replace the insufficient urethral plate, followed by a ventral onlay penile skin flap procedure.
Therefore, grafts and flaps have been paramount in the surgical reconstruction of urethral strictures and should continue as an essential instrument in the resources of the reconstructive surgeon. However, comparing the success rates of this combined technique with other reconstructive procedures is challenging at the present time. Nonetheless, the graft and flap combination appears to be very rewarding for well-selected patients as long as a variety of factors are considered.
Further randomized studies will be mandatory to support one technique over another. Until then, it is vital for the reconstructive surgeon to feel confident with a wide array of techniques to address the best treatment approach for each individual patient.
DECLARATIONS
Authors’ contributionsMade substantial contributions to conception and design of the study and performed data analysis and interpretation: Dávila F, Rosito T
Provided administrative, technical, and material support: Stojanovic B
Drafted the work and substantively revised it, made substantial contribution to conception and design of the study: Martins FE
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declare that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2022.
REFERENCES
1. Fossati N, Barbagli G, Larcher A, et al. The surgical learning curve for one-stage anterior urethroplasty: a prospective single-surgeon study. Eur Urol 2016;69:686-90.
2. Giudice CR, Becher E, Olivares AM, Tobía I, Favre GA. Dorsal oral mucosa graft in combination with ventral penile flap as an alternative to repair obliterative stenosis of the anterior urethra in a single surgical time. Int Braz J Urol 2020;46:83-9.
3. Ding J, Li Q, Li S, et al. Ten years’ experience for hypospadias repair: combined buccal mucosa graft and local flap for urethral reconstruction. Urol Int 2014;93:454-9.
4. Breyer BN, McAninch JW, Whitson JM, et al. Multivariate analysis of risk factors for long-term urethroplasty outcome. J Urol 2010;183:613-7.
5. Elliott SP, Mcaninch JW. Penile skin flaps for urethral reconstruction. In: Brandes SB, editor. Urethral Reconstructive Surgery. Totowa: Humana Press; 2008. pp. 153-64.
6. Brandes SB. Vascular anatomy of genital skin and the urethra: implications for urethral reconstruction. In: Brandes SB, editor. Urethral Reconstructive Surgery. Totowa: Humana Press; 2008. pp. 9-18.
7. Mangera A, Patterson JM, Chapple CR. A systematic review of graft augmentation urethroplasty techniques for the treatment of anterior urethral strictures. Eur Urol 2011;59:797-814.
8. Atala A, Danilevskiy M, Lyundup A, et al. The potential role of tissue-engineered urethral substitution: clinical and preclinical studies. J Tissue Eng Regen Med 2017;11:3-19.
9. Barbagli G, Lazzeri M. Surgical treatment of anterior urethral stricture diseases: brief overview. Int Braz J Urol 2007;33:461-9.
10. Bhargava S, Chapple CR. Buccal mucosal urethroplasty: is it the new gold standard? BJU Int 2004;93:1191-3.
11. Palminteri E, Berdondini E, Di Pierro GB. The advantages of the ventral approach to bulbar urethroplasty. Arab J Urol 2013;11:350-4.
13. Zinman L. Muscular, myocutaneous, and fasciocutaneous flaps in complex urethral reconstruction. Urol Clin North Am 2002;29:443-66.
14. Dubey D, Vijjan V, Kapoor R, et al. Dorsal onlay buccal mucosa versus penile skin flap urethroplasty for anterior urethral strictures: results from a randomized prospective trial. J Urol 2007;178:2466-9.
15. Tung TA, Nichols CM. Techniques in tissue transfer: plastic surgery for the urologist. In: Brandes SB, editor. Urethral Reconstructive Surgery. Totowa: Humana Press; 2008. pp. 43-52.
16. Belsante MJ, Selph JP, Peterson AC. The contemporary management of urethral strictures in men resulting from lichen sclerosus. Transl Androl Urol 2015;4:22-8.
17. Fenton AS, Morey AF, Aviles R, Garcia CR. Anterior urethral strictures: etiology and characteristics. Urology 2005;65:1055-8.
18. Lumen N, Hoebeke P, Willemsen P, De Troyer B, Pieters R, Oosterlinck W. Etiology of urethral stricture disease in the 21st century. J Urol 2009;182:983-7.
19. Pansadoro V, Emiliozzi P. Internal urethrotomy in the management of anterior urethral strictures: long-term followup. J Urol 1996;156:73-5.
20. Heyns C, Steenkamp J, De Kock M, Whitaker P. Treatment of male urethral strictures: is repeated dilation or internal urethrotomy useful? J Urol 1998;160:356-8.
21. Depasquale I, Park AJ, Bracka A. The treatment of balanitis xerotica obliterans. BJU Int 2000;86:459-65.
22. Virasoro R, Eltahawy EA, Jordan GH. Long-term follow-up for reconstruction of strictures of the fossa navicularis with a single technique. BJU Int 2007;100:1143-5.
24. Armenakas NA, Mcaninch JW. Management of fossa navicularis strictures. Urol Clin North Am 2002;29:477-84.
25. Mcaninch JW, Morey AF. Penile circular fasciocutaneous skin flap in 1-stage reconstruction of complex anterior urethral strictures. Journal of Urology 1998;159:1209-13.
28. Kuyumcuoglu U, Eryildirim B, Tarhan F, Faydaci G, Ozgül A, Erbay E. Antegrade endourethroplasty with free skin graft for recurrent vesicourethral anastomotic strictures after radical prostatectomy. J Endourol 2010;24:63-7.
29. Seth A, Saini AK, Dogra PN. Hybrid minimally invasive urethroplasty for pan-anterior urethral strictures: initial results. Urol Int 2012;89:116-9.
30. Nikolavsky D, Abouelleil M, Daneshvar M. Transurethral ventral buccal mucosa graft inlay urethroplasty for reconstruction of fossa navicularis and distal urethral strictures: surgical technique and preliminary results. Int Urol Nephrol 2016;48:1823-9.
31. Gelman J, Sohn W. 1-stage repair of obliterative distal urethral strictures with buccal graft urethral plate reconstruction and simultaneous onlay penile skin flap. J Urol 2011;186:935-8.
32. Djordjevic ML, Majstorovic M, Stanojevic D, et al. Combined buccal mucosa graft and dorsal penile skin flap for repair of severe hypospadias. Urology 2008;71:821-5.
33. Morey AF. Urethral plate salvage with dorsal graft promotes successful penile flap onlay reconstruction of severe pendulous strictures. J Urol 2001;166:1376-8.
35. Erickson BA, Breyer BN, McAninch JW. Single-stage segmental urethral replacement using combined ventral onlay fasciocutaneous flap with dorsal onlay buccal grafting for long segment strictures. BJU Int 2012;109:1392-6.
36. Tijani KH, Idiodi-Thomas HO, Elebute OA, Alakaloko FM, Ojewola RW, Ademuyiwa AO. Two-stage flap repair of severe hypospadias: usefulness of the tubularized incised plate urethroplasty. J Pediatr Urol 2017;13:483.e1-5.
37. Palminteri E, Manzoni G, Berdondini E, et al. Combined dorsal plus ventral double buccal mucosa graft in bulbar urethral reconstruction. Eur Urol 2008;53:81-9.
38. Palminteri E, Lumen N, Berdondini E, et al. Two-sided dorsal plus ventral oral graft bulbar urethroplasty: long-term results and predictive factors. Urology 2015;85:942-7.
39. Perovic SV, Djordjevic ML. The penile disassembly technique in the surgical treatment of Peyronie’s disease. BJU Int 2001;88:731-8.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Dávila F, Rosito T, Stojanovic B, Martins FE. Combined grafts and flaps in urethral stricture repair. Plast Aesthet Res 2022;9:31. http://dx.doi.org/10.20517/2347-9264.2021.133
AMA Style
Dávila F, Rosito T, Stojanovic B, Martins FE. Combined grafts and flaps in urethral stricture repair. Plastic and Aesthetic Research. 2022; 9: 31. http://dx.doi.org/10.20517/2347-9264.2021.133
Chicago/Turabian Style
Dávila, Francisco, Tiago Rosito, Borko Stojanovic, Francisco E. Martins. 2022. "Combined grafts and flaps in urethral stricture repair" Plastic and Aesthetic Research. 9: 31. http://dx.doi.org/10.20517/2347-9264.2021.133
ACS Style
Dávila, F.; Rosito T.; Stojanovic B.; Martins FE. Combined grafts and flaps in urethral stricture repair. Plast. Aesthet. Res. 2022, 9, 31. http://dx.doi.org/10.20517/2347-9264.2021.133
About This Article
Special Issue
Copyright
Data & Comments
Data

 Cite This Article 6 clicks
Cite This Article 6 clicks










Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.