Advancement flaps
Abstract
Local advancement flaps are a key tool in the armamentarium of the reconstructive surgeon. They can be used to repair small and large defects on all areas of the face with excellent skin color and texture match, limited donor site morbidity, and flexibility to hide scars. In this review, we outline common categories of advancement flaps and discuss common situations for their use.
Keywords
INTRODUCTION
Local advancement flaps are a useful tool for reconstructing facial skin defects. While many forms of local tissue reconstruction incorporate an element of advancement, advancement flaps are technically characterized by sliding or stretching the flap skin along a single vector. This type of flap therefore relies on the elasticity of the skin and/or skin redundancy to facilitate closure of the defect. Care must be taken to orient the limbs of the flap parallel to relaxed skin tension lines (RSTLs) to avoid creating an aesthetically obvious scar. Most advancement flaps are random pattern flaps, relying on the unnamed cutaneous vasculature to supply the tissue. Traditionally, a length to width ratio of no more than 3:1 is recommended, though there is no clear evidence to support this. The area of greatest tension in the closure is at the distal flap edge. Advancement flaps offer a number of benefits including excellent skin color and texture match, limited donor site morbidity, and flexibility to hide scars. Reconstructing larger defects poses challenges including distortion of normal structures and strategies to overcome these challenges will be discussed[1-3].
Advancement flaps are generally named for the shape of the closed incision including the U-plasty, H-plasty, T-plasty, V-Y, Y-V, and east-west flap. Variations on advancement flaps include subcutaneous tissue advancement, island advancement, cervicofacial rotation advancement, Bernard-Burow, and Karapandzic flaps.
Considerations when planning reconstruction
The reconstructive surgeon must always take into account a few basic principles when considering approaches to address a defect. These principles include fundamental knowledge of the functional and aesthetic anatomy of the defect site and proposed donor skin, an understanding of patterns of vascular supply in the donor tissue, and a recognition of the tension vectors associated with a proposed reconstruction including primary and secondary movement[1].
When analyzing a defect, the surgeon should take into account the specialized issues associated with reconstructing the complex topography of the face. Care should be taken to avoid distorting structures that would affect nasal patency, eye closure, or oral competence. Incisions should ideally be designed to hide in RSTLs or boundaries of aesthetic units for optimal outcomes. Donor tissue should be of adequate laxity to allow for appropriate primary movement into the defect while accounting for likely secondary movement of the adjacent tissue[3,4].
Reconstructive flaps must have a reliable vascular supply to be successful. In general, flaps can either rely on a random pattern of unnamed subcutaneous and subdermal plexuses or a larger named artery. Most advancement flaps are random patterns in nature, relying primarily on anastomoses within the subdermal plexus. This makes it incumbent upon the surgeon to elevate a flap in the appropriate plane to maintain this vascular supply. Care should also be taken to consider the proposed flap length when designing a reconstruction to ensure adequate perfusion pressure at the distal end of the flap and avoid distal necrosis. Native tissue around the defect site should be of adequate health to allow for neovascularization of the transposed flap[5,6].
UNIPEDICAL FLAPS
U-plasty
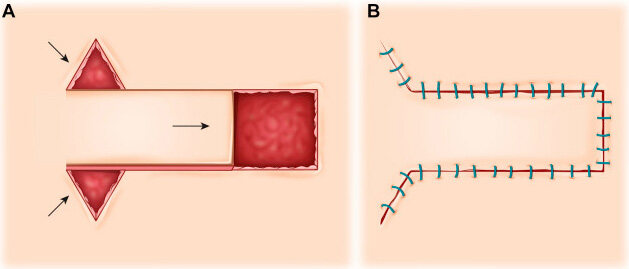
The U-plasty is a unipedicle advancement flap, meaning it has a single cutaneous pedicle. The flap is created by making parallel incisions to free up the donor skin and allow it to slide along the flap’s long axis to fill the defect. This will result in bilateral standing cone deformities at the base of the flap that may necessitate excising Burow triangles. Halving sutures could also be used to redistribute redundancy. Care should be taken to match the shape of the flap’s distal end and the donor site’s distal end. Squaring off flap edges can limit the risk of a trapdoor deformity. The flap must be completely undermined to allow for free movement. Likewise, the surrounding skin and soft tissue should be undermined to limit tension and distortion at the base of the flap [Figure 1].
Figure 1. U-plasty. (A) Two parallel incisions are made to allow for movement in a linear vector. Burow triangles may need to be excised to correct standing cone deformities. (B) Closure following advancement. This figure is used from senior authors’ previous work,
These flaps are often most useful in areas such as the forehead, where the flap incisions can be designed to lie in RSTLs or along the brow or hairline. They can also be used in the cheek, where there is abundant redundancy with care taken to design the axis of movement in a lateral-to-medial vector that minimizes the risk of tension on the lower lid or nasofacial sulcus[3]. This type of advancement flap can also be used on the nose by taking advantage of the redundancy of adjacent tissues. The Rintala flap represents a specialized form of U-plasty in which skin from the glabella is advanced inferiorly to repair defects of the nasal dorsum. Burow triangles are excised from the base of the flap to avoid distortion of the medial brow[7]. The lateral nasal advancement flap advances skin from the medial cheek onto the nasal sidewall or dorsum. Burow triangles can be well hidden within the nasofacial sulcus and alar groove[8].
H-plasty
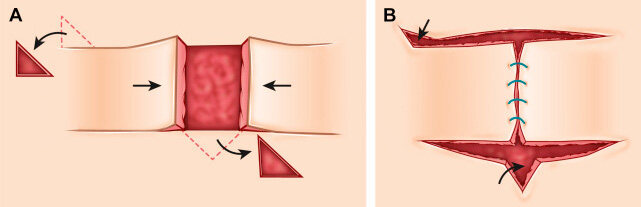
The H-Plasty is a bilateral modification of the unipedicle flap, which can be useful in closing larger defects where there is insufficient tissue or laxity unilaterally to fully close the defect. The limbs need not be the same length and can be customized to fit the character of the adjacent tissue. It is recommended to raise only one flap at a time as often more advancement than anticipated can be generated from a single flap. Like the U-plasty, standing cone deformities may be generated that can be dealt with by excising Burow triangles at the bases of the pedicles or at the defect to effectively shrink the defect. The H-plasty is useful for the forehead for the same reasons as the U-plasty and can also be helpful for reconstructing defects of the central lip and chin[2,9] [Figure 2].
Figure 2. H-plasty. (A) Bilateral linear advancement flaps raised and advanced towards central defect. Burow triangles are excised to avoid standing cone deformities. (B) Closure following advancement. This figure is used from senior authors’ previous work,
T-plasty
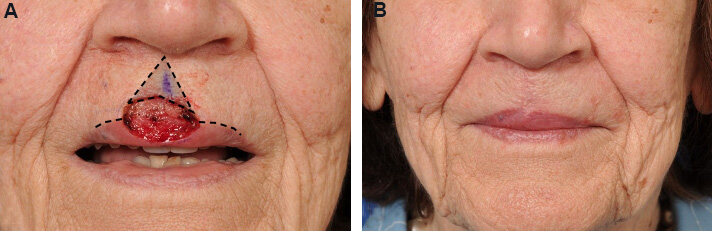
The T-plasty, like the H-plasty, is a bilateral unipedical flap that utilizes a single incision on each side of the defect to free up the skin to advance. The T-plasty may also be called an A-T or O-T, referencing the triangular or round shape of the original defect respectively. Sometimes a round defect may be made fusiform by superiorly excising a cone of tissue. The advancement of the flaps does create a standing cone deformity which is addressed by excising a Burow triangle when necessary. Like the H-plasty, the T-plasty requires smaller flaps to close the defect than a U-plasty which may be advantageous in areas with less available donor skin. Its single horizontal incision may offer a better aesthetic result than the H-plasty. The flap may be useful for forehead defects with the horizontal incision hidden in the brow or hairline or the lip with the horizontal limb oriented parallel to the vermillion border as seen in Figure 3. It is important to be mindful of scar contracture of the vertical limb when used for lip repairs, as this may result in distortion of the vermilion border[3,10].
Figure 3. T-plasty. (A) T-plasty planned to close a cutaneous defect of the upper lip. The horizontal limb is hidden along the vermillion border. The defect is extended to form an A shape to allow for the vertical limb to fall along the philtrum without tissue redundancy. (B) Closure following advancement. Scars are well hidden and the upper lip retains appropriate length. This figure is used from senior authors’ previous work, Shew et al.[1]. Rights retained.
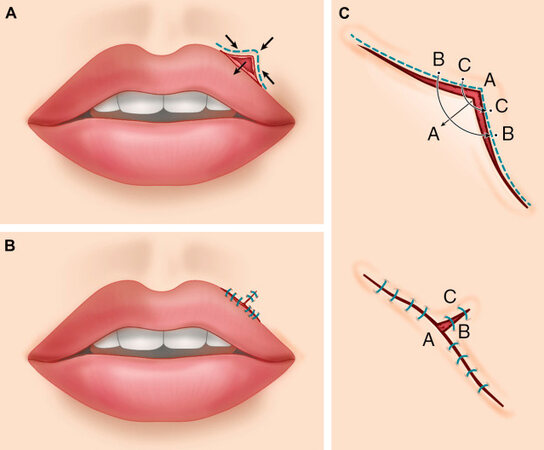
V-Y and Y-V
The V-Y advancement flap is unique in that the flap is allowed to recoil into position rather than be advanced under tension into the defect. The incision is designed so that the limbs of the V are perpendicular to the direction of desired tissue advancement. Once the tissue is advanced, the resultant triangular defect is closed with a vertical limb, the stem of the Y. This limb can often be made to fall within the boundary of an aesthetic unit or in a RSTL[11,12] [Figure 4].
Figure 4. V-Y. (A) A V-shaped incision is made along a distorted vermillion border to allow for release to normal contour. Arrows indicate anticipated vectors of tissue movement. (B) Final closure of V-to-Y advancement flap, correcting the vermillion border shape. (C) Magnified view of the planned incision and closure. The “A” marks the planned advancement, while the “B” and “C” mark the planned closure. This closure “pushes” the distorted vermillion inferiorly. This figure is used from senior authors’ previous work,
The inverse form of this advancement flap, the Y-V, starts with a Y-shaped incision that is allowed to relax and form a tissue void in the stem of the Y incision. The upper limbs of the Y then form the tissue flap that is advanced to fill the defect, resulting in a V-shaped suture line. Unlike the advancement flaps previously discussed in this article, the V-Y and Y-V are less often used for filling a defect. Their greatest benefit is addressing abnormal structures such as a short columella or retracted vermillion border[13].
Island advancement flaps
Island advancement flaps differ from the previously discussed flaps in that the incision is made circumferentially through the skin, relying on the subcutaneous tissues for the vascular supply. Some undermining can be done around the skin edges to allow for free movement into the defect though care should be taken to leave a sufficient subcutaneous pedicle. Once the donor skin is advanced into the defect and secured, the resultant secondary defect can often be closed primarily. This flap can be thought of as a V-Y approach to closing a defect, with the open end of the V lying along the edge of the defect. The limbs of the incision can be designed in a curved fashion to help hide the incision in the boundary of an aesthetic subunit. This flap can be utilized in situations where tension on a cutaneous pedicle would be too high or cause significant distortion[14-18].
A modification of the island advancement flap utilizes only the subcutaneous tissue. In this case, the skin overlying the donor tissue is left in place and only the subcutaneous fat or muscle is advanced to address the defect. This flap can be useful in addressing volume loss[3].
East-west flap
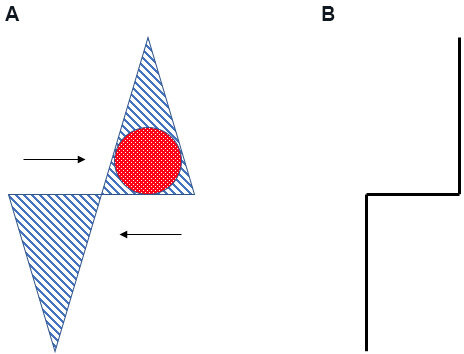
The east-west flap is a technique that utilizes diagonally opposing triangles to advance tissue along a horizontal plane into a defect while requiring relatively little tissue movement and therefore limiting distortion of surrounding tissues. The defect is incorporated into a vertically based isosceles triangle and a releasing triangle is designed along the short edge horizontal cattycorner from the defect triangle. The base of the releasing triangle is generally half the width of the defect triangle and of similar height. The skin of both triangles is excised and the resultant flaps are undermined to allow for free opposing movement along the horizontal or east-west access. Movement of the flaps to close the defect will result in a stair-step final closure appearance. This flap can be quite useful on the nose as it requires minimal tissue movement/laxity and therefore limits adjacent secondary movement. Generally, defects best served by an east-west flap are less than 1.5 cm and longer than they are wide[19-21] [Figure 5].
BIPEDICAL FLAP
The bipedicle advancement flap relies on parallel incisions made perpendicular to the direction of advancement. The bridge of tissue is then advanced into the defect. This type of flap is often used in the scalp to repair small mucosal lining defects adjacent to the nasal rim, or for septal perforation repair. These flaps leave a secondary defect that can be skin grafted or allowed to heal by secondary intention. In addition, these flaps can be useful for relocating a defect or ensuring coverage of bone or hardware with healthy tissue[22].
SPECIALTY ADVANCEMENT FLAPS
In some defects, the above-discussed flaps are not sufficient due to the size of the defect or the involvement of functional structures. Specialized advancement flaps can be used in these situations.
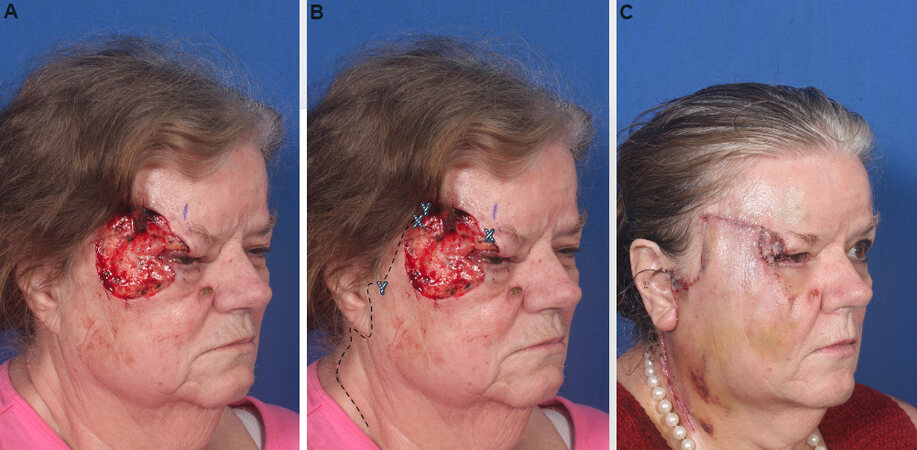
Cervicofacial advancement flap
The cervicofacial advancement flap is a random pattern flap that utilizes the tissue redundancy and elasticity often seen in the neck to address moderate to large defects of the cheek or temple. The flap is most often designed with the pedicle anterioinferiorly in the neck and the incision often follows the preauricular contour and falls into a neck crease in a similar fashion to the modified Blair incision used in parotidectomy. The flap skin is then fully undermined in the subcutaneous plane to allow free movement and rotated and advanced into the defect. Given the potentially large size of the skin paddle, attention should be paid to the distal edge of the flap for any signs of necrosis[23-26] [Figure 6].
Figure 6. Cervicofacial advancement flap. (A) Cutaneous post-Mohs defect of the temple and superior cheek measuring approximately 4 cm × 5 cm. (B) Incision premarked out with dashed lines. Incision lines are inconspicuously hidden between important aesthetic boundaries including hairline, preauricular crease and natural crease of the neck. X and Y markings demonstrate the advancement, rotation and anticipated attachment of the flap. (C) Following cervicofacial advancement flap closure. This figure is used from senior authors’ previous work, Shew et al.[1]. Rights retained.
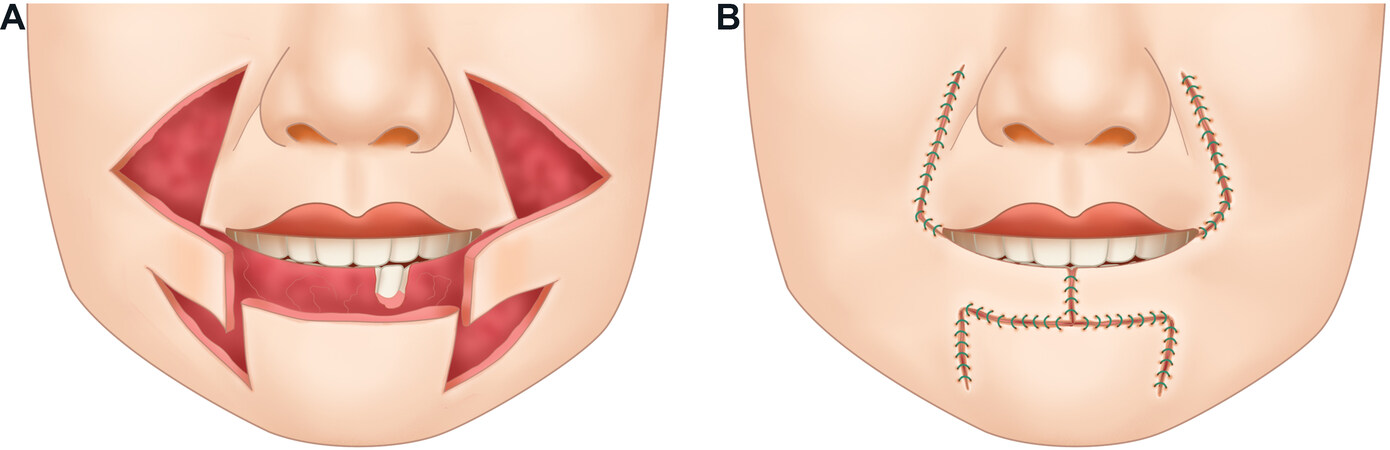
Bernard-Burow flap
The Bernard-Burow flap is a bilateral cheek advancement flap that can be used to repair up to total defects of the upper or lower lip. In this flap, skin from the bilateral cheeks is undermined and advanced to close the lip defect in a similar fashion to an H-plasty. The degree of tissue movement results in large standing cone deformities at all four corners which are addressed by excising a Burow triangle. The triangles are designed to lie in the alar facial sulcus superiorly and lateral to the oral commissure inferiorly. The vermillion lip is then reconstructed with a mucosal advancement flap. The incisions are made only through the skin and subcutaneous tissue in an effort to preserve sensory function though motor function is not preserved due to the absence of the orbicularis oris. The resultant shortened, tight lip does help with oral competency, but pursing of the lips for whistling or kissing is significantly impaired[3,27] [Figure 7].
Figure 7. Bernard-Burow flap. (A) Red portion represents a cutaneous lip defect. Blue dashed areas represent areas of excised skin to allow for free opposing movement of the skin flaps. Flaps are moved along a horizontal plane as indicated by the arrows. (B) Closed incision. An additional mucosal advancement flap is generally used for reconstruction of the vermillion lip.
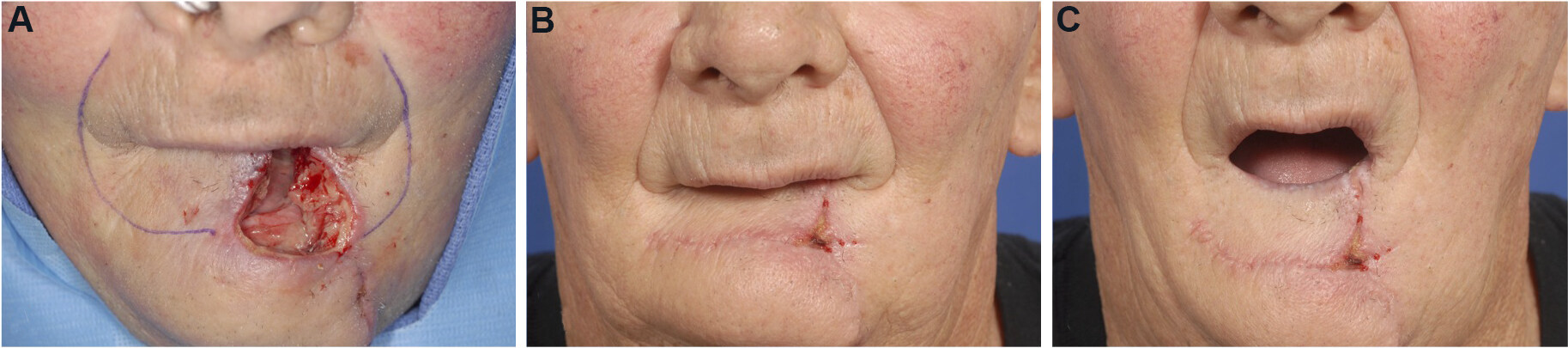
Karapandzic flap
The Karapandzic flap is a bilateral advancement flap used for closure of large full-thickness defects of the lip that do not involve the oral commissure. It differs from more simple advancement flaps for lip closure in that the incisions are not full-thickness in an effort to preserve neurovascular structures. The cutaneous incision for lower lip defects is designed to parallel to the lip within the mental crease with bilateral limbs extending around the oral commissure and up into the nasolabial creases to facilitate tissue movement. Though most often used in the lower lip, the inverse approach can be used for upper lip defects. If necessary, separate mucosal incisions are made and the intervening tissue is again bluntly dissected to preserve neurovascular structures. The flaps rotated and advanced to close the lip defect. The Karapandzic flap preserves the sensory and motor function of the lip but can create microstomia[28-31] [Figure 8].
Figure 8. Karapandzic flap. (A) Large lower mucosal and cutaneous lip defect that is full-thickness along the superior portion. Proposed partial thickness incisions marked with purple ink. (B) Post-operative photo demonstrating closure of the defect. Incision lines are hidden in the nasolabial folds and mental creases. (C) Dynamic view demonstrating minimal microstomia and intact orbicularis oris function.
OTHER CONSIDERATIONS
Solutions for inadequate local tissue - serial advancements, tissue expanders
In some situations, a defect may be situated in such a way that there is insufficient local tissue to perform the desired repair. While regional flaps, interpolated flaps, and free flaps can all offer solutions in this setting, local advancement flaps can also be utilized with some modifications. For scar revisions or the excision of large benign skin lesions, serial excisions and advancements can useful, allowing the native skin time to stretch and relax between procedures. A similar approach can be used for closure of a fresh defect. Partial closure is achieved with an advancement flap and the remaining defect is covered with a skin graft that is later serially excised[3,32,33].
Tissue expanders can also reconcile inadequate local tissue availability. Tissue expanders are often used for scalp defects to generate hair-bearing donor tissue. Expanders are sometimes useful in the cheek and forehead as well[33,34].
Complications
Skin necrosis is most often associated with flaps of larger size or length, particularly at the distal end or in areas of greater tension. Advancement flaps depend on a random pattern in blood supply that can increase this risk. Therefore, care should be taken to monitor flaps closely for congestion. Nitro paste can be used to improve congested or poorly perfused areas[5,6].
The trapdoor deformity is another potential complication of advancement flaps. This deformity is characterized by depression of the scar along the transposed tissue with bulging of the native tissue surrounding it. This deformity can be addressed in a number of ways including steroid injection, scar revision with Z-plasties, or laser treatments. The risk of developing a trapdoor deformity can sometimes be lessened with incision design and by sufficient undermining at the time of primary repair[35,36].
CONCLUSION
Advancement flaps represent a useful option for appropriately selected facial skin defects. Surgeons armed with the knowledge to effectively execute advancement flaps can close a variety of defects with limited morbidity and excellent aesthetic results.
DECLARATIONS
Authors’ contributionsMade substantial contributions to conception and design of the study and performed data analysis and interpretation: Schopper H, Humphrey C
Provided substantial review and editing support: Kriet JD
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationPatients seen at our facility sign a release of clinical photography form as part of their intake paperwork that gives blanket authorization to use photography (Figure3) for teaching or publication. The copyrights of Figures 1, 2, 4, 5 and 7 belong to authors.
Copyright© The Author(s) 2022.
REFERENCES
1. Shew M, Kriet JD, Humphrey CD. Flap basics II: advancement flaps. Facial Plast Surg Clin North Am 2017;25:323-35.
3. Baker SR. Local flaps in facial reconstruction. 3rd ed. Amsterdam: Elsevier; 2014.
4. Larrabee WF Jr. A finite element model of skin deformation. I. Biomechanics of skin and soft tissue: a review. Laryngoscope 1986;96:399-405.
5. Cutting C, Ballantyne D, Shaw W, Converse JM. Critical closing pressure, local perfusion pressure, and the failing skin flap. Ann Plast Surg 1982;8:504-9.
7. Onishi K, Okada E, Hirata A. The Rintala flap: a versatile procedure for nasal reconstruction. Am J Otolaryngol 2014;35:577-81.
8. Ogawa Y, Ogawa Y. Lateral nasal advancement flap for reconstruction of the nasal sidewall and dorsum. Arch Plast Surg 2020;47:102-5.
10. Hirshowitz B, Mahler D. T-plasty technique for excisions in the face. Plast Reconstr Surg 1966;37:453-8.
11. Narsete TA. V-Y advancement flap in upper-lip reconstruction. Plast Reconstr Surg 2000;105:2464-6.
12. Zhang WC, Liu Z, Zeng A, et al. Repair of cutaneous and mucosal upper lip defects using double V-Y advancement flaps. J Cosmet Dermatol 2020;19:211-7.
13. Yildirim S, Aköz T, Akan Md, Avci G. Nasolabial V-Y advancement for closure of the midface defects. Dermatol Surg 2001;27:656-8; discussion 658-60.
14. Kaufman AJ, Grekin RC. Repair of central upper lip (philtral) surgical defects with island pedicle flaps. Dermatol Surg 1996;22:1003-7.
15. Gardner ES, Goldberg LH. Eyebrow reconstruction with the subcutaneous island pedicle flap. Dermatol Surg 2002;28:921-5.
16. Omranifard M, Doosti MI. A trial on subcutaneous pedicle island flap for eyebrow reconstruction. Burns 2010;36:692-7.
17. Pepper JP, Baker SR. Local flaps: cheek and lip reconstruction. JAMA Facial Plast Surg 2013;15:374-82.
18. Leonhardt JM, Lawrence N. Back to basics: the subcutaneous island pedicle flap. Dermatol Surg 2004;30:1587-90.
19. Ascari-Raccagni A, Dondas A, Righini M, Trevisan G. The east-west advancement flap (horizontal advancement flap) to repair a defect on the nose ala. J Eur Acad Dermatol Venereol 2010;24:926-9.
20. Geist DE, Maloney ME. The “east-west” advancement flap for nasal defects: reexamined and extended. Dermatol Surg 2012;38:1529-34.
24. Sakellariou A, Salama A. The use of cervicofacial flap in maxillofacial reconstruction. Oral Maxillofac Surg Clin North Am 2014;26:389-400.
25. Shetawi AH, Quimby A, Fernandes R. The cervicofacial flap in cheek reconstruction: a guide for flap design. J Oral Maxillofac Surg 2017;75:2708.e1-6.
26. Hufschmidt K, Bozec A, Camuzard O, et al. Versatility of cervicofacial flaps: Cervical-medial cheek flap for reconstruction in cutaneous substance loss of the inner cheek. Head Neck 2018;40:2574-82.
27. Williams EF 3rd, Setzen G, Mulvaney MJ. Modified Bernard-Burow cheek advancement and cross-lip flap for total lip reconstruction. Arch Otolaryngol Head Neck Surg 1996;122:1253-8.
28. Sane VD, Rathi P, Narla B, Khandelwal S, Pathan W. Karapandzic flap: a useful option for reconstruction of lower lip. J Craniofac Surg 2019;30:e32-4.
29. Ethunandan M, Macpherson DW, Santhanam V. Karapandzic flap for reconstruction of lip defects. J Oral Maxillofac Surg 2007;65:2512-7.
30. Dadhich AS, Shah S, Saluja H, Tandon P, More V. Karapandzic flap for esthetic and functional reconstruction of large defect of lower lip. Ann Maxillofac Surg 2017;7:300-3.
31. Teemul TA, Telfer A, Singh RP, Telfer MR. The versatility of the Karapandzic flap: a review of 65 cases with patient-reported outcomes. J Craniomaxillofac Surg 2017;45:325-9.
32. Ford CN. Serial excision and advancement flaps in the management of facial lesions. Otolaryngol Head Neck Surg 1983;91:156-64.
33. Mostafapour SP, Murakami CS. Tissue expansion and serial excision in scar revision. Facial Plast Surg 2001;17:245-52.
34. Carruthers A. Tissue expansion and Mohs micrographic surgery. J Dermatol Surg Oncol 1993;19:1106-9.
35. Koranda FC, Webster RC. Trapdoor effect in nasolabial flaps. Causes and corrections. Arch Otolaryngol 1985;111:421-4.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Schopper H, Kriet JD, Humphrey C. Advancement flaps. Plast Aesthet Res 2022;9:25. http://dx.doi.org/10.20517/2347-9264.2021.72
AMA Style
Schopper H, Kriet JD, Humphrey C. Advancement flaps. Plastic and Aesthetic Research. 2022; 9: 25. http://dx.doi.org/10.20517/2347-9264.2021.72
Chicago/Turabian Style
Schopper, Heather, J. David Kriet, Clinton Humphrey. 2022. "Advancement flaps" Plastic and Aesthetic Research. 9: 25. http://dx.doi.org/10.20517/2347-9264.2021.72
ACS Style
Schopper, H.; Kriet JD.; Humphrey C. Advancement flaps. Plast. Aesthet. Res. 2022, 9, 25. http://dx.doi.org/10.20517/2347-9264.2021.72
About This Article
Special Issue
Copyright
Data & Comments
Data

 Cite This Article 23 clicks
Cite This Article 23 clicks










Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.