Lymphaticovenular-anastomosis treatment of the peripheral component in chyle leakage after axillary surgery: case report and review
Abstract
Axillary lymph node dissection-dependent chyle leakage is a rare complication with an incidence of < 0.7%. The morbidity could be high, and the management prolonged and not clear. The literature offers us many therapeutical tools, yet there is no consensus about the management of this complication. Usually, the management focuses on reducing the chyle flow in the thoracic duct (central origin), neglecting the possibility of a parallel lymphorrhea from other regional lymphatic vessels (peripheral origin), which causes a prolonged approach with high morbidity. In this paper, we introduce the supermicrosurgery technique as a surgical therapeutic option for chyle leakage. To decrease morbidity and shorten treatment duration, we offer a therapeutic algorithm based on the literature and our experience.
Keywords
INTRODUCTION
Chyle is a milky substance derived from the intestines during digestion and then carried by the lymphatic system[1]. Usually, it enters the venous system at the level of the left brachiocephalic vein. During surgery, iatrogenic injuries to the thoracic duct could lead to chylous leakage, especially due to aberrant anatomy[2]. Chyle leakage rarely occurs secondary to axillary surgery and little guidance exists regarding its management[3-5]. This iatrogenic complication may cause high physiological morbidity, high mental burden, prolonged treatment, and delayed primary oncologic treatment. The current therapy focuses mainly on reducing flow in the thoracic duct[6]. Our case shows that chyle leakage may include a peripheral component in addition to the central one. We demonstrated that lymphaticovenular anastomosis (LVA) can reduce peripheral component flow, therefore decreasing the total chyle leakage.
CASE REPORT
A 43-year-old woman, with a history of diabetes type 1 and bilateral breast augmentation, presented with a lump in the lateral aspect of her left breast. Mammography and breast US showed a mass, 1.8 cm in diameter without suspected axillary lymph nodes. Ultrasound-guided biopsy showed invasive duct carcinoma. Immunohistochemical evaluation showed ER+, PR+, HER2-, Ki 10%-15%. MRI imaging showed two not enlarged axillary lymph nodes with moderate cortical thickness and did not show any additional breast lesions.
Breast conservative surgery and sentinel lymph nodes biopsy were performed. Intraoperative histological examination of the lymph nodes was positive for macro metastasis. Axillary lymph node dissection (Level 1-2 nodes) was performed. It was an uneventful operation that ended with the placement of an axillary suction drain. Definitive histology revealed metastases (pN+) in 16 out of 20 removed lymph nodes. Following those findings, initiation of chemotherapy was suggested.
By the end of Postoperative Day 1 (POD), the drain collected 500 mL of a milky fluid [Figure 1]. Analysis of the milky fluid was compatible with chyle (triglycerides 2200 mg/dL). The chyle leakage was stable
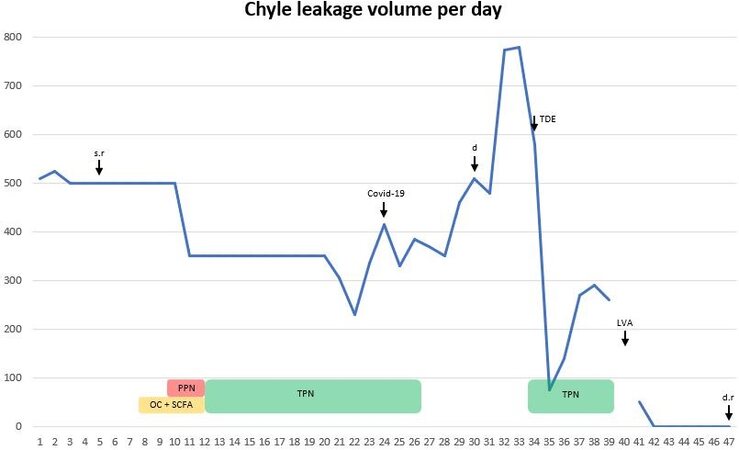
Figure 2. The graph shows the chyle leakage volume in milliliters per day, as it was measured by drain’s output. The days are counted as POD (postoperative day). During POD 4-9 and 10-20, an average chyle leakage volume was given. s.r: Surgical revision; COVID-19: date of diagnosis; d: decision; TDE: thoracic duct embolization; LVA: lymphaticovenular anastomoses; d.r: drain removal; PPN: partial parenteral nutrition; TPN: total parenteral nutrition; OC: octreotide; SCFA: short chain fatty acids.
On POD 30, the patient presented with a dehiscence of the operated wound with lymphatic fluid leakage through it. The treatment included wound debridement and skin suturing. Chyle leakage output increased significantly in the following days.
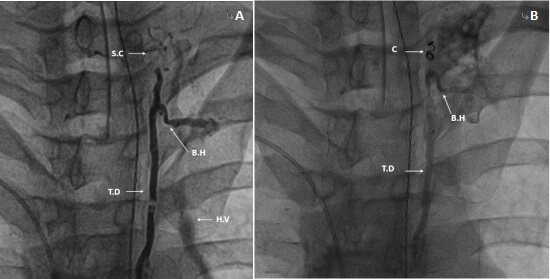
On POD 34, an inguinal intranodal lymphangiography was performed and the cisterna chyli was located and entered via percutaneous abdominal puncture. A microcatheter lymphangiography detected abnormal thoracic duct drainage laterally into the hemiazygos vein and para vertebral collateral vessels without clear evidence of axillary leakage. The distal end of the thoracic duct branched into a small collateral lymph vessel that was draining in the direction of the neck. No clear leakage was detected, and, with the idea that the small collateral lymphatic vessel might be the source of the chylous leakage, the distal end of the thoracic duct was embolized by placing two "Tornado Embolization Coils" (COOK MEDICAL LLC, USA) and using acrylic glue, "Glubran 2" (GEM Srl, Viareggio, Italy) [Figure 3]. Following the procedure, TPN was reinitiated. Initially, the leakage decreased significantly, but, within few days, it stabilized on 270 mL per day.
Figure 3. (A) A lymphographic demonstration of the thoracic duct, its draining branch (B.H) into the hemiazygos vein (H.V), and the small collateral lymph vessel (S.C) that originates from its distal end; and (B) a coil (C) used for the embolization of the distal thoracic duct.
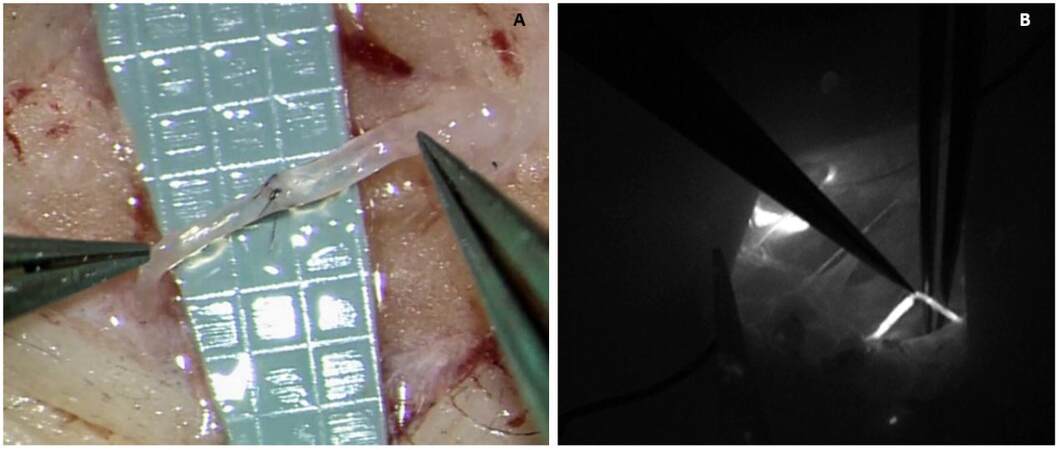
On POD 40, TPN was discontinued. Up to this day, the patient had lost about 6 kg (10% of her initial body weight). Indocyanine green (ICG)-based lymphography of the left hand was performed by injecting 0.2 mL (25 mg/10 cc) "Verdye" (Diagnostic Green LLC, Germany) into the finger web. The imaging demonstrated lymphatic vessels directing towards the axillary region and the wound bed. About 5 min after the injection, ICG started to flow into the drain, proving that lymphatic leakage from the left hand had also contributed to the chyle leakage volume [Figure 4]. This diagnostic tool demonstrated the contribution of a peripheral component to the total leakage output volume. Four end-to-end lymphaticovenular anastomoses (LVA) in the proximal left arm were performed, based on the ICG imaging of the main lymphatic pathways leading to the wound bed and drain [Figure 5]. The patency of the anastomoses was demonstrated using SPY fluorescence imaging system (Stryker Corp/Novadaq Technologies, Kalamazoo, Mich) fluorescence imaging system [Figure 6]. Exploration of the operative wound followed by debridement, placement of a new drain, and insertion of 2 mL of fibrin glue, "Tisseel" (Baxter Healthcare Corporation, USA). In the evening, the patient started P.O. nutrition. On the next day, the lymphatic drain summed to
Figure 4. (A) Lymphography demonstrates the site of ICG injection and the lymphatic vessels draining proximally to the axilla; (B) ICG-stained fluid flows through the axillary drain; and (C) ICG-stained fluid in the collecting chamber of the drain.
Figure 5. (A) One of the LVAs that were performed; and (B) the lymphography demonstrates LVA patency, by showing ICG-stained lymph draining into a local vein.
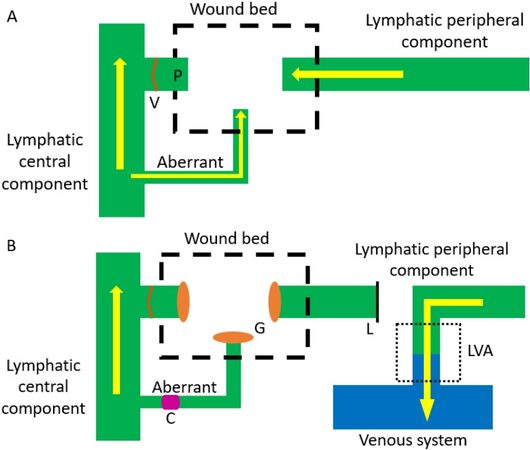
Figure 6. Schematic representation of surgical intervention. (A) The pre-interventional schematic representation. The yellow arrows represent the direction of the lymphatic flow. (B) Summary of the surgical interventions. The right yellow arrow represents the redirection of lymphatic flow from the peripheral component (limb lymphatics) towards the venous system. E: Vessels of lymphatic peripheral component; V: lymphatic vessel valves; C: embolizing coil used to stop leak from the central component; G: fibrin glue applied in wound bed; LVA: lymphaticovenular anastomosis; L: ligation of the efferent lymphatic vessel.
DISCUSSION
Chyle is a milky substance containing a high content of lipids, proteins, and lymphocytes. It is derived from the intestines during digestion and carried by the lymphatic system[1]. The thoracic duct drains lymph from the entire left body and the right side below the diaphragm. Usually, it enters the venous system at the level of the left brachiocephalic vein. During surgery, iatrogenic injuries to the thoracic duct could lead to chylous leakage, especially due to aberrant anatomy[2].
Owing to the remote anatomical location of the thoracic duct, post-axillary surgery chyle leakage is a rare complication, with an incidence of 0.36%-0.68%[3-5]. Chyle leakage complication is more commonly seen in head and neck surgery; however, because of its complexity and the lack of clinical trials, there is no consensus regarding the algorithm of management. Due to the obvious milky appearance of chyle, the current literature assumes that the main origin of the leaking fluid is the thoracic duct. Therefore, clinical experience focuses on reducing flow in the injured thoracic duct and local wound therapy. The treatment divides between conservative and surgical approaches.
The conservative management includes the following measures:
(1) Suction drain is traditionally placed during the final steps of axillary lymphadenectomy for preventing the accumulation of fluids (seroma) in the potential dead space[7]. This enables favorable wound healing conditions.
(2) Local pressure dressing: Applying external pressure on the wound bed may compress the leaking lymphatic vessels[8].
(3) Bed rest: The flow in the lymphatic system is generated by physical activity. By minimizing physical activity, the flow in the thoracic duct and its leaking branches can be reduced. Bed rest with the head of bed elevated to 30°-45° is recommended[9].
(4) Diet: A MCT diet is commonly used, with the thought that most of its absorption crosses the mucosa, straight into the portal system, sparing the lymphatic system. Despite its disadvantages, when chyle leakage does not decreases, TPN may be required to completely avoid the entrance of nutrients into the lymphatic system[10].
(5) Drugs: A somatostatin analog (octerotide) can reduce chyle production by inhibiting gastric, intestinal, and pancreatic secretions[11]. Further, lymphatic flow is reduced by its effect on smooth muscle contraction in the thoracic duct[12].
An invasive approach is used when conservative management fails to stop the leakage. The available interventional methods include the following:
(1) Surgical reexploration: Finding lymphatic vessels is a challenging task, especially when the surrounding tissue is inflamed due to the extravasated chyle. Localizing the leaking thoracic duct and its branches could become easier by the administration of a lipophilic dye such as methylene blue, patent blue, or Sudan black B[13,14]. For ameliorating its detection, a fasting patient with a lucid chyle leakage could receive a fat-rich formula a few hours prior to the surgery for whitening the chyle and increasing its flow[15]. After demonstrating the leakage, the vessels could be ligated.
(2) Local agents: Local inflammatory reaction can generate fibrosis and seal the chylous leakage. This reaction may be induced by applying an intralesional injection of sclerosing agents such as OK-432[16] or tetracycline[17]. Other agents that could be used for sealing the leakage are cyanoacrylate[18,19], fibrin glue, and polyglactin (Vicryl) mesh[20]. Reexploration after using those agents could be difficult due to the tissue alteration of the wound bed.
(3) Thoracic duct embolization: Inguinal intranodal lymphangiography is used for the visualization of the leakage. The next step involves percutaneous transabdominal catheterization of the cisterna chyli and the embolization of the thoracic duct proximally to the leaking segment[21].
The supermicrosurgery technique is an additional tool we would like to add to the treatment option of axillary lymph node dissection (ALND)-related chyle leakage. This technique is already widely used for creating LVA in a minimally invasive surgery for effectively treating limb lymphedema[22,23]. Another application is the creation of LVA in the groin for the reduction of flow and pressure in central lymphatic structures (thoracic duct) for the treatment of lymphatic pleural effusion or ascites in infants with generalized lymphatic dysplasia[24]. Although it has never been used before, the same principle could also be used for reducing axillary chyle leakage.
In the treatment of our patient, LVA created a peripheral shunt between the lymphatic system and venous system. This physiological alteration resulted in an acute decrease of lymph flow from the left arm (peripheral component) towards the lymphatic subclavian trunk and the wound bed [Figure 6]. As a consequence of creating a LVA, the drain leakage dropped from its previous steady output volume of
Farkas’s systemic review shows that conservative management was found to be effective in 38/40 of low output leakage cases (< 500 mL/day), while surgical intervention was necessary in 7/9 of high output leakage cases (> 500 mL/day)[6]. His review offers a therapeutic algorithm based on chyle leakage output per day.
Our experience shows that volume output alone was not enough to determine the best treatment approach, as was offered by Farkas’s algorithm[6]. First, surgical reexploration and the following intensive conservative treatment could not solve the chyle leakage of our patient. As a consequence, we think that the right therapeutic approach should rely mostly on the dynamics of the leakage output, as offered by Delaney’s algorithm for the treatment of chyle leakage for head and neck surgery[28].
From Farkas’s systemic review, we learn that the diagnosis of chyle leakage is usually given by sampling the milky fluid collected by the postoperative drain[6]. Diagnosis could also be made by aspirating a new postoperative swelling[29-32]. In the case of diagnosis made by collecting chyle from the drain, we suggest initiating a conservative management for the next 3-4 days and to observe the chyle output dynamics. Early surgical reexploration is suggested when the output volume does not decrease.
Rarely, the diagnosis is made by aspirating a new postoperative swelling[29-32]. In those rare cases, the chyle leakage was treated conservatively and had stopped on average 35 days after its diagnosis. Thus, with the goal of shortening the duration of treatment, we suggest proceeding to a local wound surgical treatment. Conservative management should be continued for another 3 days after the surgical treatment and chyle output dynamics should be monitored closely.
When there is no decrease in volume output and before proceeding to a thoracic duct focused approach, we would like to offer the exclusion of a peripheral component to the leakage.
ICG lymphography, a low morbidity and simple diagnostic tool, could be performed for demonstrating the lymphatic flow from the distal arm to the direction of the axilla. Diagnosis of lymphorrhea can be made if ICG, injected into the finger web, appears to flow in the drain. In this case, performing LVA in the proximal arm could decrease lymphatic leakage to the wound bed, thus ameliorating wound healing conditions and decreasing the total volume leakage output.
Exclusion of lymphorrhea (peripheral component) or no decrease in leakage output after performing LVA suggests that the main origin of leakage is the thoracic duct (central component). Inguinal intranodal lymphangiography can demonstrate this leakage. The leaking branch of the thoracic duct could be demonstrated and embolized proximally by using percutaneous transabdominal catheterization of the cisterna chyli.
Lastly, if there is no improvement after those interventions, fasting and TPN could be considered for further decreasing lymphatic flow from the intestines. TPN is reserved for the most difficult cases due to its association with an increased rate of infections, venous thrombosis, and hepatic and gastrointestinal complications[33]. Further surgical intervention should be evaluated by a multidisciplinary team.
After every intervention, we suggest continuing conservative management and monitoring chyle output. The drain should be removed when the output drops below 30 mL/day or after 5-7 days of a consecutive output decrease[7].
The algorithm in Figure 7 summarizes our above-described approach.
Figure 7. Suggested treatment algorithm for chyle leakage following axillary surgery. LVA: Lymphaticovenular anastomosis; POD: postoperative day; TPN: total parenteral nutrition.
In conclusion, axillary chyle leakage may have a significant peripheral component that can be demonstrated using ICG-based lymphography, and it can be treated effectively with LVA.
DECLARATIONS
Authors’ contributionsMade substantial contributions to conception and design of the study and performed data analysis and interpretation: Drobot A, Drobot D, Sagi OI
Provided technical and material support: Bruckheimer E, Cohen E, Atar E
Provided administrative and material support: Kakiashvili E
Availability of data and materialsThe data supporting our findings is written in Hebrew, in the discharge letters from the numerous hospitalizations of our patient.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationOur study obtained a consent from the presented patient.
Copyright© The Author(s) 2021.
REFERENCES
1. McCray S, Parrish CR. When chyle leaks: nutrition management options. Pract Gastroenterol 2004;28:60-76.
2. Phang K, Bowman M, Phillips A, Windsor J. Review of thoracic duct anatomical variations and clinical implications. Clin Anat 2014;27:637-44.
3. Nakajima E, Iwata H, Iwase T, et al. Four Cases of Chylous Fistula after Breast Cancer Resection. Breast Cancer Res Treat 2004;83:11-4.
4. Cong MH, Liu Q, Zhou WH, Zhu J, Song CX, Tian XS. Six cases of chylous leakage after axillary lymph node dissection. Onkologie 2008;31:321-4.
5. Zhou W, Liu Y, Zha X, et al. Management of chylous leakage after breast surgery: report of four cases. Surg Today 2011;41:1639-43.
6. Farkas N, Wong J, Monib S, Thomson S. A systematic review of chyle leaks and their management following axillary surgery. Eur J Surg Oncol 2020;46:931-42.
7. He XD, Guo ZH, Tian JH, Yang KH, Xie XD. Whether drainage should be used after surgery for breast cancer? Med Oncol 2011;28 Suppl 1:S22-30.
8. Nussenbaum B, Liu JH, Sinard RJ. Systematic management of chyle fistula: The Southwestern experience and review of the literature. Otolaryngol Head Neck Surg 2016;122:31-8.
9. Crumley RL, Smith JD. Postoperative chylous fistula prevention and management. Laryngoscope 1976;86:804-13.
10. Jensen GL, Mascioli EA, Meyer LP, et al. Dietary modification of chyle composition in chylothorax. Gastroenterology 1989;97:761-5.
11. Jain A, Singh SN, Singhal P, Sharma MP, Grover M. A prospective study on the role of octreotide in management of chyle fistula neck. Laryngoscope 2015;125:1624-7.
12. Jiang H, Deng XF, Duan CM, Chen C, Xiang JL, Lu YL, et al. Somatostatin receptors SSTR2 and SSTR5 are expressed in the human thoracic duct. Lymphology 2011;44:21-8.
13. Kuroiwa M, Toki F, Suzuki M, Suzuki N. Successful laparoscopic ligation of the lymphatic trunk for refractory chylous ascites. J Pediatr Surg 2007;42:E15-8.
14. Asch MJ, Sherman NJ. Management of refractory chylous ascites by total parenteral nutrition. J Pediatr 1979;94:260-2.
15. Mitsunaga T, Yoshida H, Iwai J, et al. Successful surgical treatment of two cases of congenital chylous ascites. J Pediatr Surg 2001;36:1717-9.
16. Roh JL, Yoon YH, Park CI. Chyle leakage in patients undergoing thyroidectomy plus central neck dissection for differentiated papillary thyroid carcinoma. Ann Surg Oncol 2008;15:2576-80.
17. Kassel RN, Havas TE, Gullane PJ. The use of topical tetracycline in the management of persistent chylous fistulae. J Otolaryngol 1987;16:174-8.
18. Anestis N, Christos FC, Ioannis P, Christos I, Lampros P, Stephanos P. Thoracic duct injury due to left subclavicular vein catheterization: a new conservative approach to a chyle fistula using biological glue. Int J Surg Case Rep 2012;3:330-2.
19. Muthusami JC, Raj JP, Gladwin D, Gaikwad P, Sylvester S. Persistent chyle leak following radical neck dissection: a solution that can be the solution. Ann R Coll Surg Engl 2005;87:379.
20. Gregor RT. Management of chyle fistulization in association with neck dissection. Otolaryngol Head Neck Surg 2000;122:434-9.
21. Higgins MC, Park AW, Angle JF. Chylothorax: percutaneous embolization of the thoracic duct. Oper Tech Thorac Cardiovasc Surg 2015;20:402-12.
22. Scaglioni MF, Fontein DBY, Arvanitakis M, Giovanoli P. Systematic review of lymphovenous anastomosis (LVA) for the treatment of lymphedema. Microsurgery 2017;37:947-53.
23. Drobot A, Bez M, Abu Shakra I, et al. Microsurgery for management of primary and secondary lymphedema. J Vasc Surg Venous Lymphat Disord 2021;9:226-233.e1.
24. Mihara M, Hara H, Shibasaki J, et al. Indocyanine green lymphography and lymphaticovenous anastomosis for generalized lymphatic dysplasia with pleural effusion and ascites in neonates. Ann Vasc Surg 2015;29:1111-22.
25. Jørgensen MG, Toyserkani NM, Sørensen JA. The effect of prophylactic lymphovenous anastomosis and shunts for preventing cancer-related lymphedema: a systematic review and meta-analysis. Microsurgery 2018;38:576-85.
26. Disipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol 2013;14:500-15.
27. Johnson AR, Kimball S, Epstein S, et al. Lymphedema incidence after axillary lymph node dissection: quantifying the impact of radiation and the lymphatic microsurgical preventive healing approach. Ann Plast Surg 2019;82(4S Suppl 3):S234-41.
28. Delaney SW, Shi H, Shokrani A, Sinha UK. Management of chyle leak after head and neck surgery: review of current treatment strategies. Int J Otolaryngol 2017;2017:8362874.
29. Lagarde SM, Tanis PJ, Van Der Meij S, Rutgers EJ. Chylous fistula after internal mammary chain sentinel node biopsy. Am Surg 2010;76:1309-11.
30. Abdelrazeq AS. Lymphoscintigraphic demonstration of chylous leak after axillary lymph node dissection. Clin Nucl Med 2005;30:299-301.
31. Malik M, Ruiz DE, Annamalai A, Lee S, Karsif K. Chyle fistula after simple mastectomy and sentinel lymph node biopsy: a rare occurrence. Breast J 2012;18:488-90.
32. Oba T, Ono M, Iesato A, et al. Chylous leakage after axillary lymph node dissection in a patient with breast cancer. Breast J 2018;24:438-40.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Drobot A, Drobot D, Sagi OI, Bruckheimer E, Cohen E, Atar E, Kakiashvili E. Lymphaticovenular-anastomosis treatment of the peripheral component in chyle leakage after axillary surgery: case report and review. Plast Aesthet Res 2021;8:30. http://dx.doi.org/10.20517/2347-9264.2021.19
AMA Style
Drobot A, Drobot D, Sagi OI, Bruckheimer E, Cohen E, Atar E, Kakiashvili E. Lymphaticovenular-anastomosis treatment of the peripheral component in chyle leakage after axillary surgery: case report and review. Plastic and Aesthetic Research. 2021; 8: 30. http://dx.doi.org/10.20517/2347-9264.2021.19
Chicago/Turabian Style
Drobot, Assi, Denis Drobot, Omer Itzhak Sagi, Elchanan Bruckheimer, Einav Cohen, Eli Atar, Eli Kakiashvili. 2021. "Lymphaticovenular-anastomosis treatment of the peripheral component in chyle leakage after axillary surgery: case report and review" Plastic and Aesthetic Research. 8: 30. http://dx.doi.org/10.20517/2347-9264.2021.19
ACS Style
Drobot, A.; Drobot D.; Sagi OI.; Bruckheimer E.; Cohen E.; Atar E.; Kakiashvili E. Lymphaticovenular-anastomosis treatment of the peripheral component in chyle leakage after axillary surgery: case report and review. Plast. Aesthet. Res. 2021, 8, 30. http://dx.doi.org/10.20517/2347-9264.2021.19
About This Article
Special Issue
Copyright
Data & Comments
Data

 Cite This Article 8 clicks
Cite This Article 8 clicks













Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.