Fractional CO2 laser vs. Fraxel laser for lower eyelid rejuvenation following transconjunctival lower blepharoplasty
Abstract
Aim: Transconjunctival CO2 laser lower blepharoplasty is considered to be a safe and reliable approach. A retrospective review of transconjunctival approached CO2 laser lower blepharoplasty associated with fractional CO2 laser ablation or fractioned non-ablative Fraxel laser resurfacing for lower eyelid rejuvenation is presented for comparison.
Methods: From February 1996 to February 2016, 250 patients underwent CO2 laser lower blepharoplasty with a male to female ratio of 1:7.5. The age ranged from 43 to 68 years (mean 52 years). A CO2 laser was applied to make a transconjunctival lower blepharoplasty. Immediately after CO2 laser lower blepharoplasty, 40 patients received fractional CO2 laser and 40 patients took Fraxel laser for resurfacing.
Results: Swelling occurred in all patients postoperatively. Complications related to transconjunctival CO2 laser lower blepharoplasty were 6 (2.4%) patients with conjunctival chemosis, 5 (2.0%) with ecchymosis, and 3 (1.2%) with granulomas. The early complications (≤ 1 month) related to fractional CO2 laser ablation were 40 (100%) patients with mild erythema, 40 (100%) with mild edema, 1 (2.5%) with hyperpigmentation, 1 (2.5%) with infection, and 1 (2.5%) with scarring. These problems resolved in all patients after 3 months. There was no complication after Fraxel laser right after lower blepharoplasty. The Fraxel group had short recovery time. However, there was no statistically significant difference between the two groups in final outcome (≥ 6 months).
Conclusion: Transconjunctival CO2 laser lower blepharoplasty associated with fractional CO2 laser ablation or Fraxel laser resurfacing assisted the appearance around the periorbital regions.
Keywords
INTRODUCTION
Transconjunctival laser blepharoplasty is a standard technique for removing slight excess skin and fat in the lower eyelids[1,2]. David and Sanders[3] developed and popularized the transconjunctival laser blepharoplasty procedure using a CO2 laser and others[4-6] have explored this technique to reduce the operating and recovery time for patients. Although the transconjunctival procedure involves risk to the inferior oblique muscle and the eyelid itself[1-7], with specialized training and operation techniques, surgical violation such as ectropion can be avoided.
Advances in laser technology have led to the invention of lasers that can precisely use the transconjunctival approach to remove orbital fat and thin layers of skin with minimal thermal damage to the surrounding tissue. Laser skin resurfacing refers to the use of char-free laser energy to precisely ablate or vaporize skin in thin layers in a highly controlled manner without affecting the deeper layers of the skin. The rapid pulsing or scanning of the laser beam produces predictable and reproducible effects; therefore, they are ideal for skin resurfacing. Clinical studies have shown favorable results with high-energy ultrapulse and scanned continuous-wave CO2 lasers for removing upper skin layers that have wrinkles or blemishes. In particular, ablative fractional CO2 and pulsed Er:YAG lasers as well as non-ablative CoolTouch YAG lasers and Fraxel laser have yielded favorable results and have minimized complications[8-14].
The objective of this study was to compare the laser resurfacing results in patients who underwent transconjunctival lower blepharoplasty with a CO2 laser for lower eyelid rejuvenation. The results were observed and compared using either the ablative fractional CO2 laser or non-ablative Fraxel laser for ablative resurfacing. Written informed consent was obtained from all patients after the Human Subject Review Committee approved this study.
METHODS
Our study focused on 80 patients of a 250-patient group who underwent transconjunctival lower blepharoplasty with a CO2 laser from February 1996 to February 2016. They were all Asians with Fitzpatrick skin Type III. The male to female ratio was 1:7.5, and the age range was 43-68 years (mean, 52 years). For lower eyelid rejuvenation to improve their eye pouches and fine wrinkles, a CO2 laser was applied to make a transconjunctival lower blepharoplasty. Immediately after CO2 laser lower blepharoplasty, 40 patients were treated with the fractional CO2 laser for ablative resurfacing and another 40 patients were treated with the Fraxel laser randomly.
Anesthesia
Most laser resurfacing procedures were performed in the office with a topical or local anesthesia (nerve block or field block) and sedation analgesia[15]. Passing through a subdermal injection of lidocaine with epinephrine can be used as a local anesthesia for 45 min to 3 h. The injection pain can be minimized through addition of 1 mL of sodium bicarbonate (1 mEq/mL) to each 10 mL of lidocaine. In sedated patients, oxygen is best delivered through an intraoral pediatric feeding tube, which must be covered with a laser-impermeable material (dull surface of wrinkled aluminum foil) or wet towels, or both. Oxygen was turned off when laser treatment was administered. Volatile agents must not be used for skin preparation or in anesthesia. A basin of sterile saline solution and a fire extinguisher was made accessible. For some patients, the eutectic mixture of local anesthetics (EMLA) cream (lidocaine 2.5% and prilocaine 2.5%) satisfactorily anesthetizes the skin for laser resurfacing areas. A minimum of 45 min to 1 h is required for the cream to take effect preoperatively.
Transconjunctival lower blepharoplasty
Specific precautions are necessary to ensure patient safety. Under sterilized conditions, saline-soaked towels were draped around the operative field, the smoke evacuator was put in place, and the conjunctiva and lower eyelid were anesthetized at the beginning of the procedure. As the CO2 laser can perforate the eyeball, the eye must be protected. A DeMaris retractor or two double-hook retractors were used to retract the lower eyelid anteriorly. The Jaeger bone plate was inserted into the inferior fornix, and pressure was exerted to make the fat bulge the conjunctiva outward and anteriorly. The incision was made 2 mm inferior to the tarsus or 4-5 mm below the eyelid margin. Vertically oriented blood vessels were noted, and the incision was passed through them. A second pass was usually required to cut through the capsulopalpebral fascia and lid retractors. Subsequently, a third pass opened the fat compartment, and the fat bulged out. With a CO2 laser beam focused for cutting, the fat was excised. It is essential to redrape the lower lid skin with a cotton-tipped applicator and assess the completeness of fat removal. For all three fat compartments, checking hemostasis, redraping the lid, putting pressure on the globe, and checking the surface of the lid for bulging were performed. The transconjunctival incision was closed using 5-0 Dexon, which eliminates the need for suture removal, representing another source of bleeding and trauma to the eyelid. After closure of the wound, the lower eyelid and other facial (periorbital) areas were resurfaced using a laser.
Laser resurfacing of the lower eyelid
The ablative fractional CO2 laser (Active FX. Lumenis Inc., Santa Clara, CA, USA) was used on 40 patients for lower lid resurfacing upon an area of 10 mm2 × 10 mm2 at 80-100 mJ and 150-3000 μm spot, whereas 40 patients received the fractionated non-ablative resurfacing Fraxel laser (1540-nm; Fraxel® SR laser, Reliant Technologies, Palo Alto, CA, USA) for resurfacing upon an area of 10 mm2 × 10 mm2 at 6-25 mJ and 30-50 μm spot of microscopic microthermal zones (MTZs). Immediately after the completion of resurfacing, the skin surfaces were dried and topical wound dressing or wet compresses were applied. At the end of this procedure, ice packs and cold dressings were placed over the operative areas, and the patient’s head was kept elevated.
Postoperative care
A topical ointment, such as bacitracin or vaseline, or an occlusive, semipermeable dressing was applied to all 80 patients for 7-10 days to keep the treated area moist and aid re-epithelialization postoperatively. Patients may experience minimal discomfort if the artificial dressing is left intact. Active herpes should be treated vigorously with both oral and topical acyclovir (Zovirax). Swelling observed in all patients had subsided after 3 or 4 days with the application of an ice or cold pack, but some patients may have been prescribed systemic steroids if swelling persisted. Infections should be identified through culturing and treated with appropriate antibiotics. The treated area appears pink for 2-3 months for most patients and for as long as 6 months for some patients, and the skin may have a sensation of excessive tightness between the third and eighth week after treatment. To prevent post-inflammatory hyperpigmentation (PIH), Asian patients with Type III skin color were routinely treated with hydroquinone both before and immediately after re-epithelialization. To aggressively prevent the formation of scars or keloids, intralesional steroids must be used to treat any area with persistent texture change, firmness, or pain. After non-ablative resurfacing with the Fraxel laser, the skin surfaces were dried and topical wound dressing or cold pack and wet compresses were applied and administered immediately. To compare the results of treatment for the 2 patient groups, the images were rated by three plastic surgeons who objectively evaluated the overall clinical improvement according to the improvement scale. Score values were as follows: 1, worse than before; 2, no change; 3, moderately improved; 4, markedly improved; and 5, optimal result. A paired t-test was applied and observations were recorded. The study was IRB approved (202001256B0) and adhered to the tenets of the Declaration of Helsinki.
RESULTS
A CO2 laser was used for transconjunctival lower blepharoplasty in a focused pattern with a 3-5-W continuous wave. Laser resurfacing of the lower lid was performed following transconjunctival lower blepharoplasty on two separate groups using one of two laser machines: the parameters of the ablative fractional CO2 laser resurfacing was in a pixel pattern, with pulse energy of 80-100 mJ, pulse duration of 150-300 ms, and 150 μm spot with a maximum scan area of 14,314 mm2 for 40 patients. The other group of 40 patients received non-ablative Fraxel laser ablative resurfacing treatment in an area of 10 mm2 × 10 mm2 at 6-25 mJ and
After transconjunctival laser blepharoplasty was performed for the eye pouches of lower eyelids and resurfacing of the lower lid skin, all patients were analyzed in three separate clinical sessions: at 1 month (early phase), 3 months (late phase), and > 6 months (final outcome). In the early phase, swelling occurred in all patients postoperatively. Complications related to transconjunctival laser blepharoplasty were 6 patients (2.4%) with conjunctival chemosis, 5 (2.0%) with ecchymosis, and 3 (1.2%) with granulomas. However, these problems resolved within 3 months after conservative treatment.
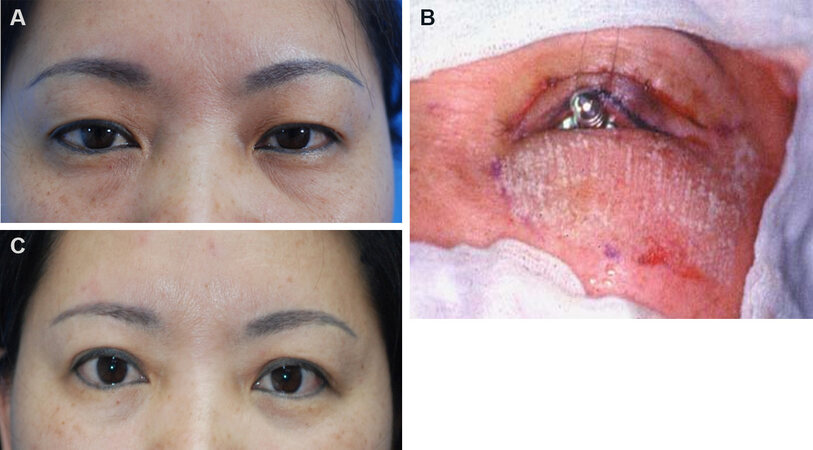
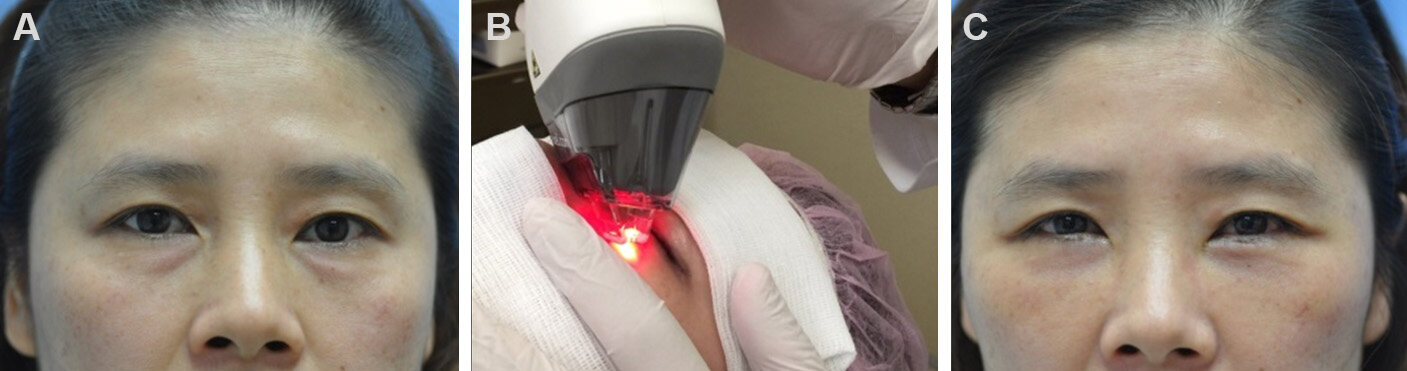
At the stages of posttreatment observation, 40 patients treated with the ablative fractional CO2 laser for resurfacing experienced minor complications of burning discomfort, edema, erythema, pruritus, and skin tightness. Among major complications in the early phase (≤ 1 month), hyperpigmentation and milia were noted in 2 patients (5.0%), while infection, ectropion, herpes simplex virus, and scarring were observed in 1 patient (2.5%). These problems resolved in most patients after the late phase (3 months). There were no minor or major complications in the 40 patients treated with Fraxel laser [Table 1]. At the final observation (> 6 months), all major and minor complications had subsided and eventually completely resolved. All patients achieved marked improvement. The difference between the two groups at the final observational status was not statistically significant (P > 0.05). Conversely, no complications were observed with the non-ablative Fraxel laser group even immediately after lower blepharoplasty [Table 1]. The typical appearance of patients before and after operation is shown in Figures 1-3.
Figure 1. A 50-year-old woman underwent CO2 laser upper and lower blepharoplasty followed by fractional CO2 laser dermabrasion: before operation (A); fractional CO2 laser dermabrasion immediately after orbital fat removal (B); and 6 months after operation (C).
Figure 2. A 47-year-old woman underwent CO2 laser lower blepharoplasty followed by Fraxel laser resurfacing: before operation (A); orbital fat was removed using CO2 laser followed by Fraxel laser resurfacing (B); and 6 months after operation (C).
Figure 3. A 57-year-old woman underwent CO2 laser transconjunctival lower blepharoplasty followed by Fraxel laser resurfacing: before operation (A); orbital fat was removed using CO2 laser followed by Fraxel laser resurfacing (B); and 6 months after operation (C).
Major complications in patients undergoing fractional CO2 laser vs. Fraxel laser resurfacing after CO2 laser lower blepharoplasty
| Phase | Early phase ≤ 1 month (%) | Late phase ≤ 3 months (%) | Final outcome ≥ 6 months (%) | |||||
| Wavelength (nm) | I | II | I | II | I | II | ||
| Hyperpigmentation | 2 (5.0) | 0 | 1(2.5) | 0 | 0 | 0 | ||
| Milia | 2 (5.0) | 0 | 0 | 0 | 0 | 0 | ||
| Infection | 1 (2.5) | 0 | 0 | 0 | 0 | 0 | ||
| Ectropion | 1 (2.5) | 0 | 1 (2.5) | 0 | 0 | 0 | ||
| Herpes simplex virus | 1 (2.5) | 0 | 0 | 0 | 0 | 0 | ||
| Scarring | 1 (2.5) | 0 | 1 (2.5) | 0 | 0 | 0 | ||
| P-value | < 0.05 | < 0.05 | > 0.05 | |||||
DISCUSSION
Baker et al.[16] were the first to report upper blepharoplasty using CO2 laser, and Baker[17,18] has been enthusiastically using this laser procedure for over 10 years. David and Sanders[3] and later Morrow and Morrow[4] compared the use of a CO2 laser with the cold-steel and electrocautery procedures for blepharoplasty through a comparative study in which one eyelid surgery was performed using a laser and the other using conventional techniques. Both studies[3,4] reported that the CO2 laser treatment reduced operating time and caused less bleeding, postoperative ecchymosis, and edema. However, these authors did not observe any discernible differences in the long-term outcomes. David and Abergel[19] monitored conjunctival temperature during upper eyelid laser blepharoplasty and found a maximum increase of 1.5 ℃ in conjunctival temperature, thus demonstrating the absence of any thermal injury to the conjunctiva or eye during this procedure. Although Mittelman and Apfelberg[20], in another paired eyelid study, reported that the CO2 laser has no advantages over a cold knife, Apfelberg now supports the use of a CO2 laser for blepharoplasty. A surgeon who used a CO2 laser in 4000 blepharoplasties found the laser to be faster and the recovery time of the patient shorter compared with cold steel[5]. Although a CO2 laser has been used for routine upper blepharoplasty and transconjunctival lower blepharoplasty, it is also an excellent tool for more complex skin-muscle flap procedures of the lower lid[21].
Laser administration nonetheless can have disadvantages. High costs, technical challenges, and safety hazards are the most apparent. Incisional procedures using the CO2 lasers can be technically challenging[22,23]. Although laser blepharoplasty is gaining acceptance rapidly by patients and surgeons alike, the superiority of this technique over cold steel has not been unequivocally established or disproved. Before transconjunctival blepharoplasty of the lower lid, the laser is tested on a tongue blade held over a nonflammable surface away from the patient to ensure the beam is under proper parameters. After the incision, the laser is defocused and used to coagulate any blood vessels larger than 0.5 mm that did not coagulate during the initial incision. Fat should not be excised by pulling or forceful distraction as this will tear the vessels and result in bleeding complications and fat over-resection, which produces a cadaveric appearance in the patient. Fat should be resected using gentle pressure on the globe until the fat flushes to the orbital rim but not beyond. During orbital fat removal, it is essential to note that the inferior oblique and inferior rectus muscles can be injured.
Laser resurfacing can also come with risks[24]. It is operator dependent and has a steep initial learning curve, and, therefore, specialized and state-of-the-art equipment is required with mandatory specialized staff training. Complications and risks are involved with laser resurfacing when safety regulations and precautions are not thoroughly followed. Laser safety guidelines should be established to ensure that eye, fire, respiratory, electrical, and patient safety measures are in place. Ablative and non-ablative lasers offer diversity in strength and coverage area. The beam from ablative lasers, such as 10,600-nm wavelength CO2 lasers, is efficiently absorbed in superficial (water-containing) cutaneous tissue. The beam pattern of such lasers is computer-controlled for precision, which allows uniform and rapid treatment, consistent results, reduced user errors, and considerably less thermal damage. The ablative laser’s precision control for tissue ablation and less residual thermal damage results in faster re-epithelialization and dermal remodeling induced by new collagen formation. Collagen shrinkage caused by controlled heat deposition leads to skin tightening, which is most easily observed on the infraorbital skin.
Fractional laser resurfacing involves delivery of the CO2 laser energy in a pixel-like fashion where 0.3-mm holes are punched into the skin through a computer-generated pattern. In this laser technology, microscopic columns of 10,600-nm CO2 laser energy are delivered across the skin barrier, penetrating 20% of the skin surface area close to each other. The remaining 80% of non-ablated skin surface areas facilitate faster healing with less complication risk[14]. The main non-ablative laser rejuvenation modalities involve midinfrared laser application. Certain lasers, such as Fraxel (1540-nm) lasers, have been demonstrated to induce dermal remodeling for improvement in skin tone. Furthermore, treating the skin fractionally with patterns of MTZs results in a unique wound-healing process. This is aided by the fact that each laser spot is surrounded with healthy tissue. Most stem cells and melanocytes in the papillary dermis are spared. Conversely, although only 15%-30% of the epidermis is affected during treatment under an MTZ pattern, the entire skin is affected in the wound-healing response. A type of protein called heat shock proteins (HSPs) helps in the repair process. Two types of HSPs exist: Hsp47 is a general inflammation marker, whereas Hsp72 is indicative of new collagen formation. On the first day after Fraxel laser treatment, Hsp72 is activated with increased dermal activity. However, Hsp47 level does not increase. Furthermore, 1 week after treatment, Hsp47 is upregulated in the dermis corresponding to new collagen remodeling around the MTZs[25,26]. Contrary to ablative laser rejuvenation procedures, non-ablative laser rejuvenation procedures induce a dermal healing response with minimal injury to the epidermis. Improving skin appearance without injuring the epidermis is a hallmark of non-ablative skin rejuvenation. A subthreshold laser-induced injury to the dermis or the dermal vasculature theoretically results in a wound repair response, fibroblast stimulation, and collagen reformation[27].
Complications with laser skin resurfacing were categorized as mild, moderate, and severe. Mild complications included edema, erythema, milia, acne exacerbation, pruritus, burning sensation, eczema, and allergic dermatitis. Moderate complications included transient PIH, hypopigmentation, limited bacterial or fungal infection (candidiasis), local herpes simplex reactivation, and telangiectasia. Severe complications included disseminated infection, hypertrophic scarring, and ectropion formation[28-30]. In our previous studies, we observed that Asian patients had skin reddening (erythema) and dyspigmentation (hypopigmentation and hyperpigmentation) for weeks or even months after CO2 laser treatment, as well as scarring in some cases. Therefore, to ensure good results and avoid complications, understanding the importance of laser tissue interactions is necessary[31].
With proper execution, laser resurfacing is effective and has many benefits. It is less operator dependent, has little intraoperative and postoperative bleeding, and has less infection risk. Pulse laser allows easier control, which means that thermal damage is controlled for collagen shrinkage. Because laser resurfacing is accurate, its postoperative care is simple, with little need for wound care; therefore, laser resurfacing can be combined with other methods and surgical procedures. Combining laser resurfacing with new laser systems allows even more precise ablation without excessive thermal damage. Furthermore, to minimize alteration in dermal-stromal tissue, which results in scarring and unwanted pigmentation, certain (parts of) skin structures must remain intact to allow for repopulation with melanocytes and keratinocytes. Parts of the follicular and the appendage apparatus function as a reservoir for reseeding. Extensive ablation and heat deposition may lead to irreparable damage to the deeper layers of the reticular dermis. However, some thermal damage is necessary to cause tissue (collagen) shrinkage, which is partially responsible for clinical improvement.
Transconjunctival laser blepharoplasty may affect the elasticity of patients’ lower eyelid(s) following CO2 laser treatment. The ablative fractional laser and non-ablative Fraxel laser can both be administered to aid in the ablative resurfacing of the lower eyelid, with the Fraxel laser posing optimal treatment and comparatively no resulting posttreatment complications for rejuvenating the periorbital skin. The limitation of this comparative study using scalpel, electrical cautery, and proper parameters for ablative lasers can be put into our further studies.
DECLARATIONS
AcknowledgmentsThis project was supported by research grants awarded of Chang Gung Memorial Hospital (CMRP 821, CMRPG3E0581). Additional institutional support was received from the National Science Council (NMRPG9002: NSC 89-2314-B-182A-150), Taiwan.
Authors’ contributionsConcept and design: Chang CJ
Data collection and analysis: Wang YP
Read, corrected the article and discussed the content: Wang YP, Hsiao YC, Chang CJ
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateThe study was IRB approved (202001256B0) and adhered to the tenets of the Declaration of Helsinki. The study is obtained consent to participate from participants.
Consent for publicationWritten informed consent was obtained from all patients.
Copyright© The Author(s) 2021.
REFERENCES
1. Jelks GW, Jelks EB. Preoperative evaluation of the blepharoplasty patient. Bypassing the pitfalls. Clin Plast Surg 1993;20:213-23; discussion 224.
2. Zarem HA, Resnick JI. Expanded applications for transconjunctival lower lid blepharoplasty. Plast Reconstr Surg 1991:88;215-20.
3. David LM, Sanders G. CO2 laser blepharoplasty: a comparison to cold steel and electrocautery. J Dermatol Surg Oncol 1987;13:110-4.
4. Morrow DM, Morrow LB. CO2 laser blepharoplasty. A comparison with cold-steel surgery. J Dermatol Surg Oncol 1992;18:307-13.
5. Lask G. Laser may be faster and better than scalpel for blepharoplasty. Skin Allergy News 1992;23:20.
6. Trelles MA, Sanchez J, Sala P, Elspas S. Surgical removal of lower eyelid fat using the carbon dioxide laser. Am J Cosmet Surg 1992;9:149-52.
7. Westfall CT, Shore JW, Nunery WR, Hawes MJ, Yaremchuk MJ. Operative complications of the transconjunctival inferior fornix approach. Ophthalmology 1991;98:1525-8.
8. Chernoff G, Slatkine M, Zair E, Mead D. SilkTouch: a new technology for skin resurfacing in aesthetic surgery. J Clin Laser Med Surg 1995;13:97-100.
9. Fulton JE Jr. Dermabrasion, chemabrasion, and laserabrasion. Historical perspectives, modern dermabrasion techniques, and future trends. Dermatol Surg 1996:22;619-28.
10. Waldorf HA, Kauvar AN, Geronemus RG. Skin resurfacing of fine to deep rhytides using a char-free carbon dioxide laser in 47 patients. Dermatol Surg 1995;21:940-6.
11. Lowe NJ, Lask G, Griffin ME, Maxwell A, Lowe P, Quilada F. Skin resurfacing with the Ultrapulse carbon dioxide laser. Observations on 100 patients. Dermatol Surg 1995;21:1025-9.
12. Cotton J, Hood AF, Gorin R, Beesen WH, Hanke CW. Histologic evaluation of preauricular and postauricular human skin after high-energy, short-pulse carbon dioxide laser. Arch Dermatol 1996:132;425-8.
13. Chang CJ. Combining the CO2 laser and the endoscope to remove soft tissue masses from the forehead area. Photomed Laser Surg 2005;23:509-12.
14. Li YH, Chen JZ, Wei HC, et al. A Chinese experience of fractional ultrapulsed CO2 laser for skin rejuvenation. J Cosmet Laser Ther 2010;12:250-5.
15. Wolfort FG, Kanter WR. Aesthetic blepharoplasty. 1st ed. Boston: Little, Brown and Company; 1995.
16. Baker SS, Muenzler WS, Small RG, Leonard JE. Carbon Dioxide Laser Blepharoplasty. Ophthalmology 1984;91:238-44.
18. Baker SS. The Ultrapulsed CO2 Laser as Cutting Tool: Upper Blepharoplasty &Lid Ptosis. Syllabus of the American Society for Aesthetic Plastic Surgery, Inc: endorsed course “New Horizons in Aesthetic Laser Surgery: Practical Use of the UltraPulse CO2 Laser for Facial Rejuveration”. San Francisco, California, 1995.
19. David LM, Abergel RP. Carbon dioxide laser blepharoplasty: conjunctival temperature during surgery. J Dermatol Surg Oncol 1989;15:421-3.
20. Mittelman H, Apfelberg DB. Carbon dioxide laser blepharoplasty--advantages and disadvantages. Ann Plast Surg 1990;24:1-6.
21. Seckei BR. Personal approach to blepharoplasty and skin-musle flap with the CO2 laser. Syllabus of the American Society for Aesthetic Plastic Surgery, Inc. endorsed course “New Horizons in Aesthetic Laser Surgery; Practical Use of the UltraPulse CO2 Laser for Facial Rejuvenation”. San Francisco, California, 1995.
22. Fitzpatrick RE, Goldman MP. CO2 laser Surgery. In: Goldman MP, Fitzpatrick RE, editors. Cutaneous laser surgery: The art and science of selective photothermolysis. St. Loui, Mosby-Yearbook, Inc. 1994;198-258.
23. Scarano A, Lorusso F, Brucoli M, Lucchina AG, Carinci F, Mortellaro C. Upper eyelid blepharoplasty with voltaic arc dermabrasion. J Craniofac Surg 2018;29:2263-6.
24. Grubbs, C Bowen. Mycobacterium abscessus infection following home dermabrasion. Cutis 2019;104:79-80.
25. Manstein D, Herron GS, Sink RK, Tanner H, Anderson RR. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med 2004;34:426-38.
26. Chan NP, Ho SG, Yeung CK, Shek SY, Chan HH. The use of non-ablative fractional resurfacing in Asian acne scar patients. Lasers Surg Med 2010;42:710-5.
27. Trelles MA, Alvarez X, Martín-Vázquez MJ, et al. Assessment of the efficacy of nonablative long-pulsed 1064-nm Nd:YAG laser treatment of wrinkles compared at 2, 4, and 6 months. Facial Plast Surg 2005;21:145-53.
28. Carraway JH, Mellow CG. The prevention and treatment of lower lid ectropion following blepharoplasty. Plast Reconstr Surg 1990;85:971-81.
29. Alster TS, Lupton JR. Treatment of complications of laser skin resurfacing. Arch Facial Plast Surg 2000;2:279-84.
31. Chang CJ. Laser skin resurfacing in Asian patients. In: Pu L, Chen YR, Li QF, et al, editors. Aesthetic Plastic Surgery in Asians: Principles and Techniques. Thieme Medical Pub, 2015.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Wang YP, Hsiao YC, Chang CJ. Fractional CO2 laser vs. Fraxel laser for lower eyelid rejuvenation following transconjunctival lower blepharoplasty. Plast Aesthet Res 2021;8:23. http://dx.doi.org/10.20517/2347-9264.2021.17
AMA Style
Wang YP, Hsiao YC, Chang CJ. Fractional CO2 laser vs. Fraxel laser for lower eyelid rejuvenation following transconjunctival lower blepharoplasty. Plastic and Aesthetic Research. 2021; 8: 23. http://dx.doi.org/10.20517/2347-9264.2021.17
Chicago/Turabian Style
Wang, Yen-Po, Yen-Chang Hsiao, Cheng-Jen Chang. 2021. "Fractional CO2 laser vs. Fraxel laser for lower eyelid rejuvenation following transconjunctival lower blepharoplasty" Plastic and Aesthetic Research. 8: 23. http://dx.doi.org/10.20517/2347-9264.2021.17
ACS Style
Wang, Y.P.; Hsiao Y.C.; Chang C.J. Fractional CO2 laser vs. Fraxel laser for lower eyelid rejuvenation following transconjunctival lower blepharoplasty. Plast. Aesthet. Res. 2021, 8, 23. http://dx.doi.org/10.20517/2347-9264.2021.17
About This Article
Copyright
Data & Comments
Data

 Cite This Article 3 clicks
Cite This Article 3 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.