One-stage mastopexy and augmentation mammoplasty in layers: outcome analysis of first 50 consecutive cases
Abstract
Aim: The single-stage procedure is a challenging procedure for Plastic Surgeons. The single-stage layered mastopexy with augmentation is a new technique that is aiming to add safety, preserving breast function and to restore normal parameters of breast.
Methods: A retrospective chart review of 50 consecutive cases of layered mastopexy with augmentation mammoplasties was performed. All patients had their implants placed in muscle splitting pocket. Incisions for mastopexy were selected on the basis of nipple areolar complex to inframammary crease. Mastopexy is performed using a medially based pedicle, leaving a sufficient tissue covering the implant. Patients were divided into three groups. Group “A” who had periareolar mastopexy, Group “B” had vertical scar mastopexy and Group “C” patients had mastopexy with Wise pattern markings.
Results: Group A comprised 11 patients. The mean age was 28.82 ± 7.01 years, mean preoperative and postoperative nipple areolar complex (NAC) to IMC measurement was recorded in 10 patients with the mean of 7.15 ± 1.98 cm and 8.35 ± 1.18 cm respectively. Mean size of the implant used was 379.55 ± 77.18 cm3. Group B comprised 29 patients. Mean age was 35.17 ± 12.37 years and the mean preoperative and postoperative NAC to IMC crease was 8.53 ± 1.48 cm and 9.72 ± 1.51 cm respectively. The mean implant size used was 289.48 ± 109 cm3. Group C had 10 patients. Mean age was 39.60 ± 12.15 years and the mean preoperative and postoperative NAC to IMC crease of 10.11 ± 1.24 cm and 8.75 ± 0.98 cm respectively. The mean implant size used was 287.00 ± 55.08 cm3.
Conclusion: The procedure allows better arterial supply, wider area for venous and lymphatic drainage, better sensory innervation to NAC and maximises lactation potential of the breast.
Keywords
Introduction
Historically breasts are considered a sign of femininity, fertility and beauty. From the time of puberty, attainment of body silhouette with feminine curve is considered an accomplished milestone. A lack of or loss of such proportions may potentially affect the self esteem in some individuals whether the condition is primary or secondary, following pregnancies, breast feeding, ageing or loss of weight. Augmentation and mastopexy is one commonly performed procedure to restore the body silhouette, feminine curves and attractive body proportions. The procedure can be performed in stages as mastopexy first to be followed by implant placement later or one stage mastopexy with augmentation. One-stage or simultaneous mastopexy with augmentation has an advantage of being cost-effective along with single hospitalisation and single recovery. Even though the procedure was first performed by Gonzalez-Ulloa[1] and Regnault[2], one still has to go through a challenging learning curve before starts achieving consistently predictable results. The results of one-stage augmentation mastopexy are frequently compared with mastopexy or breast augmentation when performed alone[3-8]. Outcome of these studies have concluded that in suitably selected patients, one-stage augmentation mastopexy procedure is relatively safe. However the analysis was primarily carried out to compare the complications of each constituent components without considering the influence of the technique used for implant placement or markings selection for breast or skin excision and their impact on the physiological, anatomical or aesthetic outcome.
Implant pocket for mammoplasty and skin tightening for mastopexy are two distinctively separate procedures regardless of the stages selected, each influencing the other as well as having an impact on overall results[9]. Various implant pockets, from initial subglandular pocket to the most recent Muscle Split Biplane technique, highlight the importance and advantages attached to each[10-14]. Scar selection for mastopexy can be a surgeon’s choice. However, it is not without its impact on the outcome leading to revision surgeries[5,15,16]. There is a lack of information where a technique has been defined for the preservation of the function of breast, the safety of the procedure along with the restoration of normal breast morphometry leading to a predictable aesthetic outcome. The following is the author’s experience of having performed 50 one-stage augmentation mammoplasties in two years.
Methods
A retrospective analysis of 50 cases of consecutive layered mastopexy with augmentation mammoplasties, over a 2-year period, was carried out. All patients had Regnault Grade II or III ptosis where Grade II ptosis is when nipple areolar complex (NAC) 2-3 cm below infra mammary crease (IMC) and grade III ptosis is when NAC is > 3 cm below IMC. All implants were placed in muscle splitting pocket first and access for the pocket was closed prior to the commencement of mastopexy. Incisions for mastopexy were selected on the basis of pre-existing NAC to IMC. In all cases, mastopexy is performed using a medially based pedicle, leaving a good layer of breast parenchymal tissue covering the implant, below and above the pedicle and where skin excision is performed. Patients were divided into three groups on the basis of existing NAC to IMC measurements.
Group “A” comprised patients who had periareolar mastopexy, Group “B” had patients with vertical single scar markings and Group “C” comprised patients who had their mastopexy carried out using Wise pattern markings.
All patients provided written informed consents. The study was performed with guiding principles set forth in the Declaration of Helsinki.
Markings and technique
After taking careful history and examination, patient’s breast measurements are taken. Markings for mastopexy are selected on the basis of NAC and IMC measurements. Selection of size of the implants is made for each patient according to the selected markings and patient’s requirements where possible. Limitation of increase in breast cup size is explained to the patient. When vertical or Wise pattern scar is selected, no more than two cup sizes are promised. Patients presenting with breast asymmetry and chosen for vertical or Wise pattern scars, have more tissue excised from larger breast with similar size breast implants placed on both sides. Patients presenting with breast asymmetry and selected for periareolar scars, are managed with different size implants.
All patients are marked in standing position with medially based flap and 4.2 cm NAC. IMC is taken as a reference for neo-NAC repositioning. Patients with NAC to IMC measurements of less than 5 cm and with a lack of skin envelope are selected for Benelli periareolar markings. Patients with measurements between 5 cm to 8 cm are selected for vertical scar and patients with NAC to IMC measurement of more than 8 cm are best suited for Wise pattern scar. Patients with pseudoptosis and wishing for an increment of at least three breast cup sizes are considered for periareolar mastopexy with implants, even if they present with more than 5 cm NAC to IMC distance.
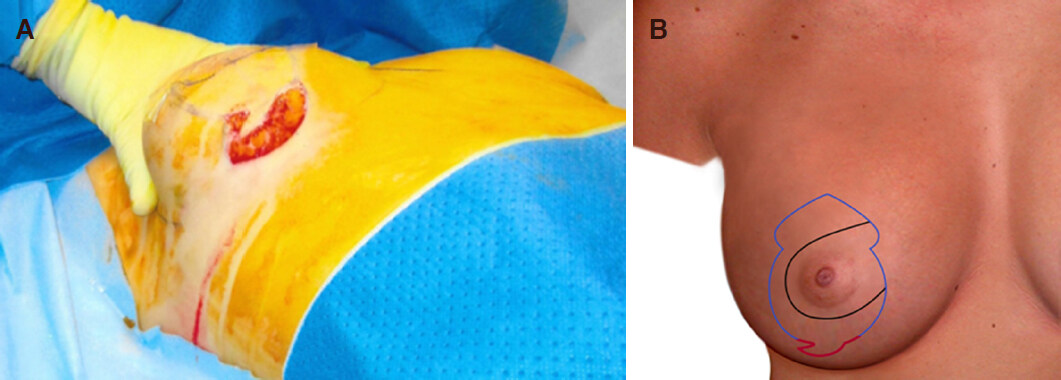
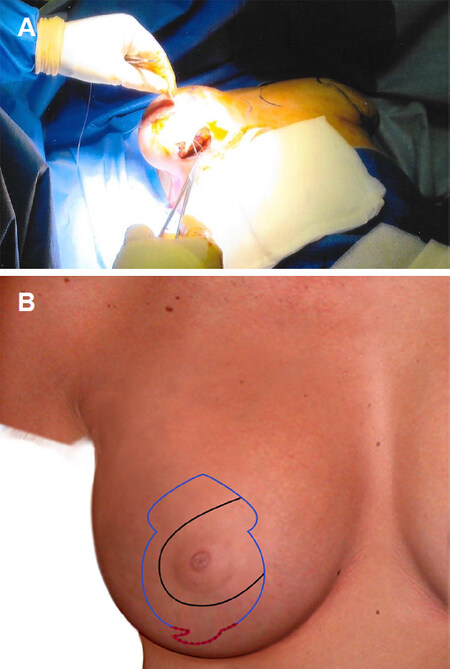
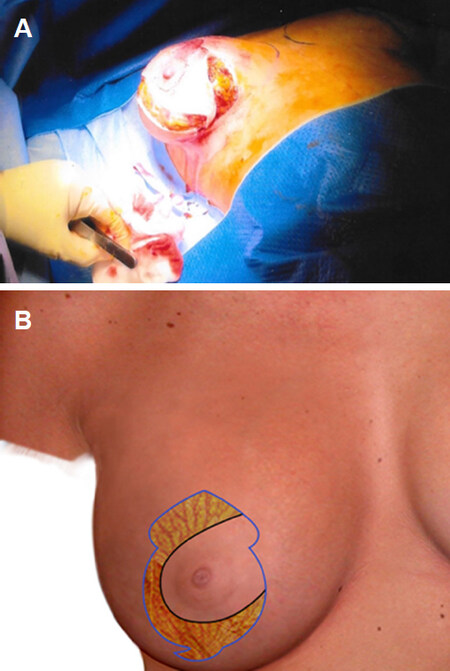
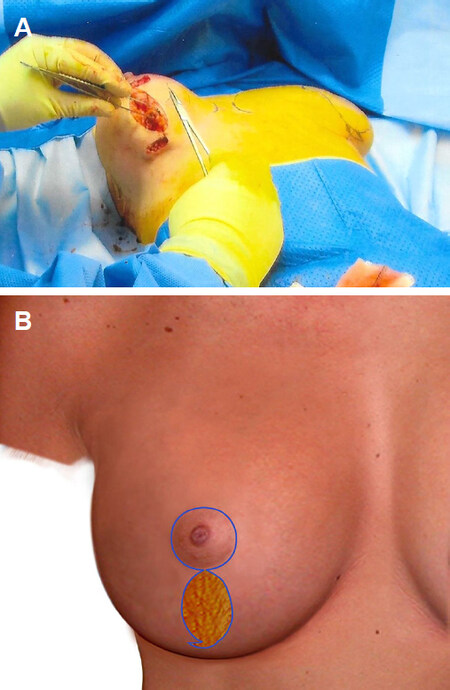
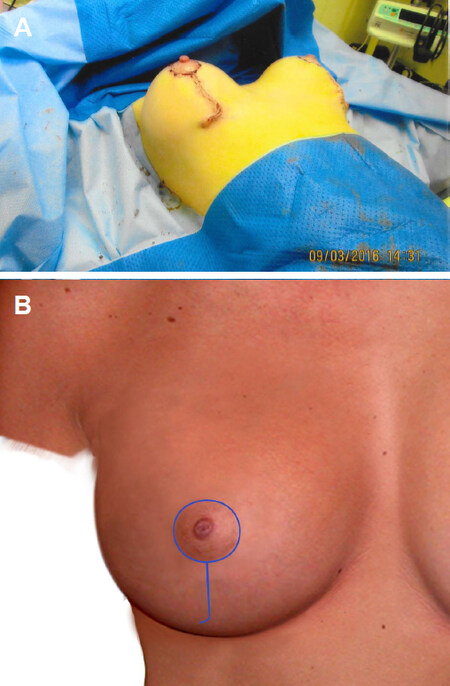
Single-staged mastopexy with augmentation is performed as a day case under full general anaesthetic with full muscle relaxation. A single intravenous dose of Cephalosporin is given followed later by an oral course of antibiotics for five days. No drains are used for this procedure. Existing IMC is marked along with new position of the nipple, usually 1.5 cm higher than IMC. In vertical and Wise pattern scars mastopexy, Keyhole for neo NAC is marked with upper margin of the neo-NAC, 2.5 cm higher than the marked neo-nipple position. Medial and lateral margins of the neo-NAC are marked at 3.5 cm from the centre of the keyhole. From this point two lines, 2.5-3 cm long each, are dropped, gently curving down centrally to leave 5-6 cm as the neck of the keyhole. From the neck of keyhole, 5-7 cm long gently curvilinear lines are dropped down and generally 6-8 cm apart at its widest. In vertical scar markings, the lines are extended inferiorly toward the central line drawn between the mid-clavicular points to a mid-point on IMC, generally 8.5-9 cm from body midline. These vertical markings end 2 cm higher than the existing inframammary crease and a cat’s tail extension is drawn laterally for the prevention of dog-ear. In Wise pattern markings, 5-7 cm long medial and lateral markings are extended to the medial and lateral extent of the marked IMC crease. This transverse wedge or ellipse of skin helps to raise the existing IMC, control and reduce postoperative NAC and IMC measurements and limits available skin envelop to prevent future bottoming out. Implant pocket is accessed through an incision made at the lower end of the Cat’s tail marking or middle of the transverse crease, which is about 5 cm wide [Figure 1A and B]. After initial subglandular pocket in lower and outer quadrant, a muscle split biplane pocket is created. The pectoralis is split from the junction of middle and lower third of sternal attachment and continues up and laterally to the anterior axillary fold along a line just below Neo-NAC . Round cohesive gel silicone implants are placed in muscle split biplane pocket through the lower end of the vertical scar or Wise pattern markings [Figure 2A-C]. Patients with periareolar markings have their implants placed through a separate access in IMC. Once implant placement is completed, haemostasis is checked and access is closed [Figure 3A and B].
Figure 1. Intraoperative picture and illustration of patient showing incision at the lower end of vertical scar single staged mastopexy with augmentation (A, B)
Figure 2. Picture showing showing implant in muscle split pocket (A); illustrations showing level of muscle split at the junction of middle and lower third sternum and implant in muscle splitting pocket (B, C)
Figure 3. Intraoperative picture and illustration showing deep fascial layer of implant pocket access being closed (A, B)
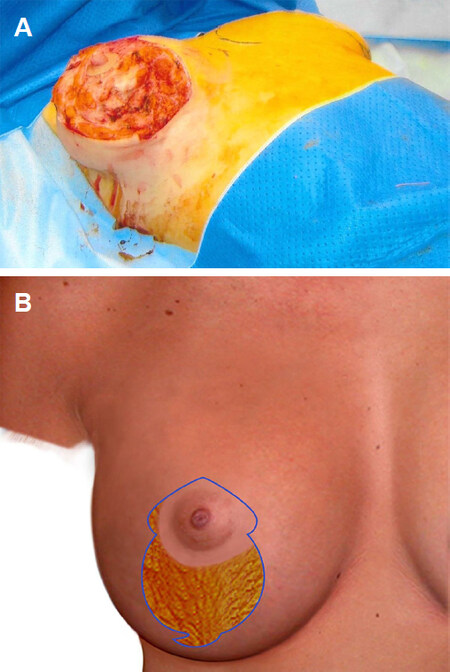
Using Lane’s forceps, skin markings are checked for tension free closure with implant already in place. Adjustments are made where required for a safe and tension free closure. Marked medially based flap is de-epithelialized, leaving 4.2 cm wide NAC as a routine in all three types of markings [Figure 4A]. Skin and subcutaneous tissue excision is performed, in moderation, superior and lateral to the de-epithelialised flap to create an adequate space for flap mobilisation and resetting [Figure 4B]. In vertical and Wise pattern markings, skin excision is continued below the medially based flap and according to the skin markings. Between the medial and lateral vertical markings, the tissue excision is little more generous to prevent lower pole redundancy but leaving enough tissue layer and without implant being visible through intermediate layer [Figure 5A]. In Wise pattern markings, tissue is excised from lateral and medial extensions, into the respective pole of the breast, in a similar way. A good layer of breast parenchymal tissue is left for implant coverage [Figure 5B]. Haemostasis is performed, three layer closure is done using absorbable sutures [Figures 6 and 7]. Flap is checked for tension free closure and nipple circulation, if any tightness is observed, piecemeal tissue is removed between flap and new-NAC margins. In case of skin envelope tightening, nipple circulation compromise or venous congestion, I do not hesitate exchanging for smaller size implants.
Figure 5. Tissue excision superior, lateral and inferior to the pedicle leaving enough tissue cover for the implant cover (A, B)
Figure 6. Intraoperative picture and illustration showing mobilised nipple areolar complex into its new position and commencement of layered closure of medial and lateral pillars (A, B)
After closure, steri-strips and light adhesive dressings are applied. A decent size hole is left in the dressing covering NAC for its circulation monitoring. A compression brassiere is placed and patients are transferred to the ward for postoperative monitoring. Nipple circulation is checked hourly before the patients are discharged. Patients are advised to take a picture of the nipples and send it to author if they notice any change in colour for an early and timely intervention.
Statistical analysis
The data were analysed using the Statistical Package for the Social Sciences (SPSS), version 19.0. The results are presented in the text as frequency, percentage for qualitative/categorical variables and mean, Standard deviation for quantitative/continuous variables. The Chi-square/exact test is used to compare the categorical variables and ANOVA test for quantitative/continuous variables. In all statistical analysis, only P-values < 0.05 are considered significant.
Results
Group A
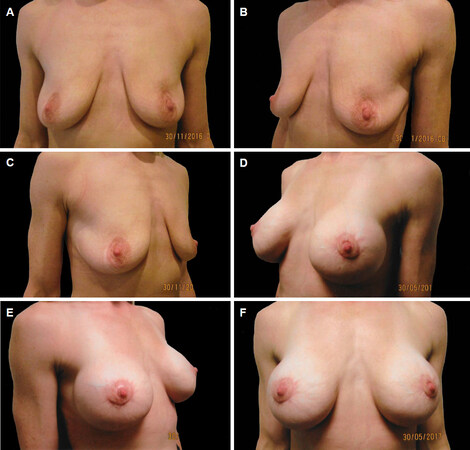
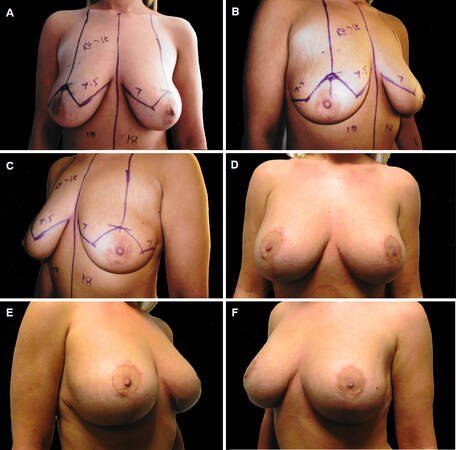
The group comprised 11 patients. The mean age of the patients was 28.82 ± 7.01 years (range 20-44), mean preoperative and postoperative NAC to IMC measurement, recorded in 10 patients, was 7.15 ± 1.98 cm (range 4.5-11) and 8.35 ± 1.18 cm (range 7.0-10.0) respectively. Mean preoperative Sternal Notch (SN) to NAC, marked SN to NAC and postoperative SN to NAC measurements were 22.45 ± 2.06 cm (range 19.5-26.0), 20.95 ± 1.01 cm (range 19.5-22.5) and 22.33 ± 0.60 cm (range 22-24) respectively. Tissue excised was minimal and not measured. Mean size of the implant used was 379.55 ± 77.18 cm3 [Table 1 and Figure 8A-F].
Showing age of the patients, implant size used and tissue removed in relevant groups
| Type of procedure | Number | Range | Mean | Std deviation | P value | |
|---|---|---|---|---|---|---|
| Age in years | PA | 11 | 20-44 | 28.82 | 7.01 | 0.101 |
| VSCT | 29 | 20-66 | 35.17 | 12.37 | ||
| WP | 10 | 23-64 | 39.60 | 12.15 | ||
| Implant size (cm3) | PA | 11 | 275-560 | 379.55 | 77.18 | 0.026 |
| VSCT | 29 | 240-800 | 289.48 | 109.00 | ||
| WP | 10 | 225-420 | 287.00 | 55.08 | ||
| Tissue excised right side (g) | VSCT | 12 | 17-78 | 46.67 | 17.39 | 0.001 |
| WP | 4 | 77-227 | 138.50 | 63.44 | ||
| Tissue excised left side (g) | VSCT | 12 | 28-106 | 56.0 | 23.84 | 0.001 |
| WP | 4 | 105-142 | 124.50 | 15.28 |
Group B
The group comprised 29 patients. The mean age of group was 35.17 ± 12.37 years (range 20-66) and the mean preoperative and postoperative NAC to IMC crease of 8.53 ± 1.48 cm (range 5.0-13) and 9.72 ± 1.51 cm (range 6.5-12) respectively. Mean preoperative Sternal Notch (SN) to NAC, marked SN to NAC and postoperative SN to NAC measurements were 24.69 ± 2.01 cm (range 21.5-30), 21.00 ± 1.25 cm (range 18.5-23.5) and 20.76 ± 1.40 cm (range 19-24) respectively. Mean weight of the tissue excised was 46.67 ± 17.39 g (range 17-78) and 56.00 ± 23.84 g (range 28-106) on the right and left side respectively. The mean implant size used was 289.48 ± 109 cm3 [Table 1 and Figure 9A-F].
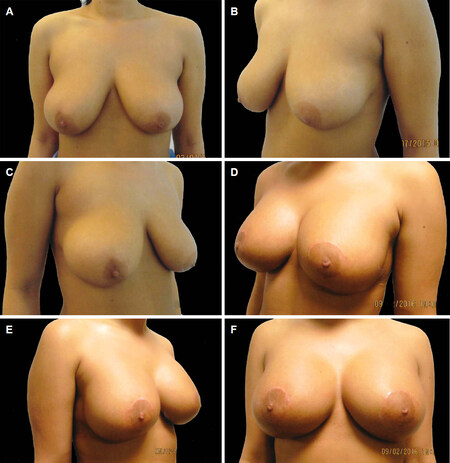
Group C
The group comprised 10 patients. The mean age of group was 39.60 ± 12.15 years (range 23-64) and the mean preoperative and postoperative NAC to IMC crease of 10.11 ± 1.24 cm (range 9-13) and 8.75 ± 0.98 cm (range 7-10) respectively. Mean preoperative Sternal Notch (SN) to NAC, marked SN to NAC and postoperative SN to NAC measurements were 27.27 ± 2.70 (range 23.0-32.0), 23.30 ± 3.22 (range 19.5-31.0) and 21.92 ± 2.33 cm (range 19-25) respectively. Mean weight of the tissue excised was 138.50 ± 63.44 g (range 77-227) and 124.50 ± 15.28 g (range 124.50) on the right and left side respectively. The mean implant size used was 287.00 ± 55.08 cm3 [Table 1 and Figure 10A-F].
Figure 10. Preoperative pictures of a 22-year-old patient who presented with Grade B ptosis following pregnancy (A-C); postoperative pictures taken five months following her surgery using 230 low profile textured round cohesive gel silicone implants (D-F)
In the series, there was no haematoma, wound breakdown or nipple loss. There was one implant related complication in which patient developed a Grade III to IV Capsular contracture without pain or loss of shape. There were two revisions performed/planned related to mastopexy. One patient developed bottoming out following a vertical scar mastopexy where preoperative NAC to IMC measurements on the right larger breast was 9cm. The other was a patient who presented with a breast hypertrophy and severe ptosis, lost the shape of the breast postoperatively following further weight loss. She is waiting for her scars to settle down before a skin envelope readjustment is performed.
Discussion
One-stage mastopexy and augmentation mammoplasty remains a challenging procedure for all Plastic Surgeons especially for those who are at the beginning of their career. Since the introduction of the procedure[1,2], single stage mastopexy with augmentation’s overall safety, outcome and complications are compared when the augmentation mammoplasty or mastopexy is performed alone[3-8]. Intrinsically single-stage mastopexy with augmentation is a combination of two procedures[9], the augmentation, in which an implant is placed in any pocket[9-14] and the mastopexy, where markings can be selected on the basis of surgeon’s experience[5-7,16]. The challenging aspect of the surgery is the combination of the two procedures where mastopexy is performed to reduce and tighten the breast skin envelope and breast implant is placed to expand skin envelope and enhance breast cup size, both being diagonally opposite[17]. As opposed to patients requiring breast implants for augmentation or requesting mastopexy for ptosis correction, the cohort of patient requiring single-stage mastopexy with augmentation is a totally different clinical subgroup. In later cohort of patients, mastopexy alone will leave them with too small and disproportionate breasts and augmentation alone will result in a larger breast with displeasing ptosis. A patient requiring augmentation mammoplasty alone generally has a hypoplastic breast with parameters in normal but reduced proportion, in these cases an implant alone will enhance breast proportionally without disturbing overall interrelationship of individual normal breast parameters. On the other hand, a patient requiring mastopexy with augmentation presents with a relatively larger breast accompanied with ptosis along with deranged inter-relationship of its constituent morphological parameters. An ideal breast surgery in this cohort needs to restore the normal parameters, enhance breast size in moderation and reduce skin envelope without compromising safety or physiological function. Ideally, incision and marking selection for single-stage mastopexy with augmentation is paramount to achieve such desired goals and symmetry[18]. These parameters are achieved in current series where relative proportions of operated breasts were brought into harmony again. With statistically different preoperative NAC to IMC and STN to NAC measurements in all three types of markings used [Tables 1-3], markings based on preoperative NAC-IMC measurements, allowed the postoperative measurement and dimensions in all three subsets to be similar and comparable without any statistical significance [Tables 1-3]. In restoring and achieving such proportions, parameters and desired aesthetic results are achieved when the two components of single stage procedure were performed independently to each other in the same setting. Augmentation mammoplasty is performed first independent of the mastopexy and once accomplished, the access is closed and then operation proceeds to mastopexy at the same time as the second half of the procedure. The independence of each procedure, performed separately at the same time, helps to maintain the integrity of each and without disturbing the other and allowing the surgeon to have a control on each of the procedure’s components. When the procedure is performed in layers, as described in the technique section, the process allows maximising safety of the procedure and aimes to retain the physiological functions of the breasts at the same time. Medially based NAC flap has an enhanced blood supply due to its broader link to surrounding tissues as it is not entirely based on length and breadth ratios, similarly venous and lymphatic drainage is assisted due to pedicle’s wider connections. Retention of the sensory potential of the NAC is more predictable and in childbearing age females, lactation potential of the breast for future pregnancies is sufficiently preserved.
Preoperative and postoperative nipple areolar complex and inframammary crease measurements in three groups
| Type of Procedure | Number | Range | Mean | Std deviation | P value | |
|---|---|---|---|---|---|---|
| NAC-IMC Preoperative | PA | 10 | 4.5-11.0 | 7.15 | 1.98 | 0.001 |
| VSCT | 29 | 5.0-13.0 | 8.53 | 1.48 | ||
| WP | 9 | 9.0-13.0 | 10.11 | 1..24 | ||
| NAC-IMC Postoperative | PA | 7 | 7.0-10.0 | 8.35 | 1.18 | 0.056 |
| VSCT | 23 | 6.5-12.0 | 9.72 | 1.51 | ||
| WP | 6 | 7.0-10.0 | 8.75 | 0.98 |
Pre and postoperative Suprasternal notch to nipple areolar complex measurements in three groups
| Type of procedure | Number | Range | Mean | Std deviation | P value | |
|---|---|---|---|---|---|---|
| Preoperative STN-NAC | PA | 11 | 19.5-26 | 22.45 | 2.06 | 0.001 |
| VSCT | 29 | 21.5-30.0 | 24.69 | 2.01 | ||
| WP | 10 | 23.0-32.0 | 27.27 | 2.70 | ||
| Marked STN-NAC | PA | 10 | 19.5-22.5 | 20.95 | 1.01 | 0.003 |
| VSCT | 29 | 18.5-23.5 | 21.00 | 1,25 | ||
| WP | 10 | 19.5-31.0 | 23.30 | 3.22 | ||
| Postoperative STN-NAC | PA | 6 | 22-24 | 22.23 | 0.60 | 0.063 |
| VSCT | 19 | 19-24 | 20.76 | 1.40 | ||
| WP | 6 | 19-25 | 21.92 | 2.33 |
In the series Moderate profile implants were most commonly used in VSCT and WP scars mastopexy as compared to extra high implants used in PA mastopexy with implants [Table 4].
Profile of the cohesive gel silicone implants used in periareolar, vertical scar cat’s tail and Wisw pattern markings
| Implant profile | Type of procedure | P value | ||
|---|---|---|---|---|
| PA | VSCT | WP | ||
| High profile | 5 (45.5%) | 6 (20.7%) | 1 (10.0%) | 0.017 |
| Moderate profile | 1 (9.1%) | 19 (65.5%) | 7 (70.0%) | |
| Extra high profile | 5 (45.5%) | 4 (13.8%) | 2 (20.2%) | |
Another safety feature of having an intervening layer of robust tissue, between closure lines and implant, is the potential advantage of implant not being exposed should there be any skin envelope breakdown. This wound breakdown is not uncommon following Wise pattern markings at the junction of vertical and horizontal closure. Wound breakdown with resultant exposure or extrusion of implant necessitates implant removal with a time lapse to allow healing to consolidate before further insertion of the prosthesis is considered possible. The intermediate layer can enable the wound to be treated conservatively obviating the explantation of the device with its concomitant morbidity and patient’s disappointment and distress. Even though there is a lack of techniques described to preserve function and add safety to the procedure, a recently published Balcony Technique, has described the preservation and use of lower half of subcutaneous layer of breast tissue as an intermediate layer of balcony sandwiching implant between itself and pectoralis muscle[19]. This preserved layer of tissue acts, as a safety net in Wise pattern closure where T-junction wound breakdown is not uncommon. However, lower half of balcony tissue layer requires its dissection separately and once achieved, is discontinuous with the upper half of the breast. The balcony technique is novel on its own but layered mastopexy provides continuity of the intermediate tissue layer without additional dissection that enhances arterial supply to the pedicle with wider area for venous and lymphatic drainage and is associated with least cutaneous sensation and lactation potential discontinuity and disruption. Other breast conserving single stage mastopexy with augmentation procedures have been described. The least invasive being simple deepithelialisation with a temporary overinflated expander and once the mastopexy is completed, the expander would be replaced with suitable smaller size implants in the same setting[20].
Owsley has described breast conserving single stage augmentation mastopexy. The technique involves circumferential skin undermining between proposed new NAC level and existing inframammary crease. Pocket for implant is approached by incising lower edge of the breast and inflatable devices placed and skin only excision performed as Wise pattern[21]. Similarly minimal tissue excision in Wise pattern inferior pedicle flap or periareolar markings with submuscular implants is described[22]. However almost all of these techniques have limitations in that they are suitable for hypoplastic or small ptotic breasts. Preservation of tissue in lower pole of the breast may result in redundancy and secondary ptosis of lower pole. Layered single stage augmentation mastopexy addresses this issue, with excision of tissue in the lower central pole allowing breast tissue to mould and drape over the implant for natural and aesthetic rejuvenation. The Layered single stage augmentation mastopexy technique also allows the procedure to be performed in less than ideal patients who present with hypertrophy with ptosis without much risk to the safety of the nipple. However, the outcome of these procedures where larger reductions are performed for mastopexy, is less than ideal in aesthetic terms. The aim and priority of an ideal procedure has to be safety of the procedure as well as good aesthetic outcome with longer lasting results. I prefer to operate on this particular group of patients as a staged procedure where reduction and mastopexy should be performed first and augmentation mammoplasty should follow later.
The weakness of the study is that there was no objective and scientific assessment of enhanced arterial supply, better venous and lymphatic drainage performed. There were no tests carried out for claimed sensation or lactation potential nor were either of these modalities compared to a control group. A larger sample with longer follow up along with quantitative and qualitative assessment of these modalities will be the way forward to establish and quantify increased blood supply, better venous return, improved lymphatic drainage, quality and degree of sensation and lactation potential.
In conclusion, early results of single-stage augmentation with mastopexy have shown that the design of this technique carries a greater potential of conserving physiological function with added safety to nipple circulation, sensation and venous drainage. Selection of incision for skin removal based on preoperative NAC to IMC measurements increases the potential to bring harmony in breast parameters.
Declarations
Authors’ contributionsThe author contributed solely to the article.
Availability of data and materialsNone.
Financial support and sponsorshipNone.
Conflicts of interestThe author declared that there are no conflicts of interest.
Ethical approval and consent to participateAll procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individuals participants included in the study.
Consent for publicationNot applicable.
Copyright© The Author(s) 2018.
REFERENCES
1. Gonzalez-Ulloa M. Correction of hypertrophy of the breast by exogenous material. Plast Reconstr Surg 1960;25:15-26.
2. Regnault P. The hypoplastic and ptotic breast: a combined operation with prosthetic augmentation. Plast Reconstr Surg 1966;37:31-7.
3. Stevens WG, Macias LH, Stoker DA, Chacon CO, Eberlin SA. One-stage augmentation mammoplasty: a review of 1192 simultaneous breast augmentation and mastopexy procedures in 615 consecutives patients. Aesthet Surg J 2014;34:723-32.
4. Calobrace MB, Herdt DR, Cothron KJ. Simultaneous augmentation/mastopexy: a retrospective 5-year review of 332 consecutive cases. Plast Reconstr Surg 2013;131:145-56.
5. Swanson E. Prospective comparative clinical evaluation of 784 consecutive of breast augmentation and vertical mammoplasty performed individually and in a combination. Plast Reconstr Surg 2013;132:30e-45e.
6. Spear SL, Pelliere CV, Menon N. One-stage augmentation combined with mastopexy: aesthetic results and patient satisfaction. Aesthetic Plastic Surg 2004;28:259-67.
7. Khan UD. Augmentation mastopexy and augmentation mammoplasty: an analysis of 1,406 consecutive cases. Plast Aesthet Research 2016;3:26-30.
8. Khan UD. A long-term review of augmentation mastopexy in muscle splitting biplabe. Plast Aesthet Res 2016;3:21-5.
9. Khan UD. Augmentation Mastopexy in muscle splitting biplane: an outcome of first 44 consecutive cases of mastopexies in a new pocket. Aesth Plast Surg 2010;34:313-21.
10. Cronin TD, Gerow RM. Augmentation mammoplasty: new “natural feel” prosthesis. In the translation of the Third International Congress of the Plastic Surgery. Excerpta Medica International Congress Series, no 66 Excerpta Medica. Amsterdam: Excerpta Medica Foundation; 1964. pp. 41-9.
11. Dempsey WC, Latham WD. Subpectoral implantsin augmentation mammoplasty: a preliminary report. Plast Reconstr Surg 1968;42:515.
12. Tebbet JB. Dual plane breast augmentation: optimizing implant-soft tissue relationship in a wide range of breast types. Plast Reconstr Surg 2001;107:1255.
13. Graf RM, Bernardes A, Rippel R, Araujo LR, Damasio RC, et al. Subfascial breast implant: a new procedure. Plast Reconstr Surg 2003;111:904.
14. Khan UD. Muscle splitting breast augmentation: a new pocket in a different Plane. Aesth Plast Surg 2007;31:553-8.
15. Spear SL, Boehmler JH, Clemens MW. Augmentation/mastopexy: a 3-year review of a single Surgeon’s practice. Plast Reconstr Surg 2006;118:136S-47S. discussion 148S-9S, 150S-1S
16. Khan UD. Vertical scar mastopexy with Cat’s tail extension for prevention of skin redundancy: an experience with 17 consecutive cases following mastopexy and mastopexy with breast augmentation. Aesth Plast Surg 2012;36:303-7.
17. Khan UD. Use of nipple areolar complex to inframammary crease measurements to reduce bottoming out after augmentation mastopexy. In: Mugea TT, Schifmann MA, editors. Aesthetic Surgery of the Brest 1st ed. Berlin, Heidelberg: Springer-Verlag; 2015.
18. Khan UD. Preoperative planning and breast implant selection for volume difference management in asymmetrical breasts. Plast Aesthet Res 2017;4:108-15.
19. Vita RD, Zoccali G, Buccheri EM. The balcony technique of breast augmentation and inverted-T mastopexy with an inferior dermoglandular flap. Aesthet Surg J 2017;37:1114-23.
20. Rappaport NH, Spira M. A simplified technique for deepithelialisztion in patients requiring augmentation mastopexy. Plast Reconstr Surg 1982;70:494-5.
21. Owsley JQ. Simultaneous mastopexy and augmentation for correction of the small, ptotic breast. Ann Plast Surg 1979;2:195-200.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Khan UD. One-stage mastopexy and augmentation mammoplasty in layers: outcome analysis of first 50 consecutive cases. Plast Aesthet Res 2018;5:45. http://dx.doi.org/10.20517/2347-9264.2018.58
AMA Style
Khan UD. One-stage mastopexy and augmentation mammoplasty in layers: outcome analysis of first 50 consecutive cases. Plastic and Aesthetic Research. 2018; 5: 45. http://dx.doi.org/10.20517/2347-9264.2018.58
Chicago/Turabian Style
Khan, Umar Daraz. 2018. "One-stage mastopexy and augmentation mammoplasty in layers: outcome analysis of first 50 consecutive cases" Plastic and Aesthetic Research. 5: 45. http://dx.doi.org/10.20517/2347-9264.2018.58
ACS Style
Khan, UD. One-stage mastopexy and augmentation mammoplasty in layers: outcome analysis of first 50 consecutive cases. Plast. Aesthet. Res. 2018, 5, 45. http://dx.doi.org/10.20517/2347-9264.2018.58
About This Article
Copyright
Data & Comments
Data
 Cite This Article 0 clicks
Cite This Article 0 clicks













Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.