Tips and tricks for getting more out of your delayed primary repair of ruptured flexor pollicis longus tendon
Sir,
Primary tendon repairs are often difficult in patients with delayed presentation. Tendons are contracted and shortened with extensive scarring occurring along the path of the tendon. Pulleys and the wound bed can be filled with granulation tissue which obstructs the passage of the tendon. Many of such patients would then be treated with a two stage tendon reconstruction, which involves the insertion of a silicone rod for pseudosheath formation[1] before tendon grafting at a second stage. This however, would set the patient back for roughly six months, especially involving multiple visits to physiotherapy and being off work. We would like to describe several tips and tricks in our armamentarium and illustrate these using a case we recently encountered [Figure 1].
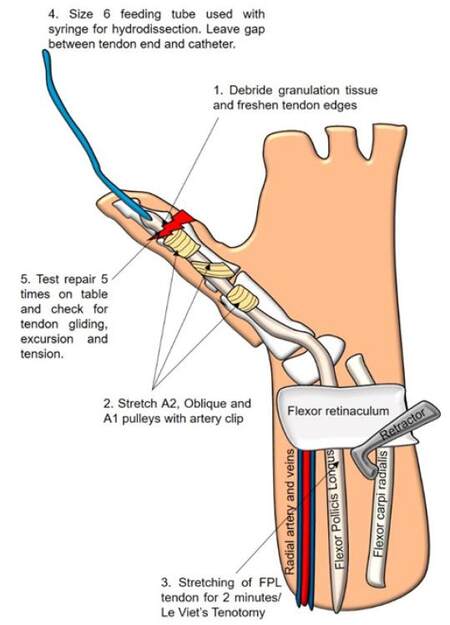
Figure 1. Schematic diagram illustrating the tips and tricks used for getting more out a primary FPL tendon repair. FPL: flexor pollicis longus
A 40-year-old mechanic presented with a 5-week-old rupture of the flexor pollicis longus (FPL) at the interphalangeal joint (IPJ) of the left thumb. A plan for a two-stage reconstruction of the tendon was discussed with him and was scheduled for a silicone rod insertion. Bruner incisions to zone 3 were made and the distal end of FPL was seen but the proximal end had retracted to the wrist.
Our tips and tricks used were as follows:
1. Use of a size 6 feeding catheter attached to a saline-filled syringe for hydrodissection of the path. Palpation of the catheter through the skin can be performed to allow localisation of path.
2. Adequate debridement of granulation and scar tissue was performed along the path of the tendon, especially under the pulleys of the thumb. Pulleys were also stretched using a fine tooth artery clip for several seconds, which avoided any venting.
3. The FPL tendon found at the wrist level was delivered through a wrist incision and stretched under tension for 2 min using an artery clip. Le Viet’s releasing incisions can be performed at the tendon-muscle belly junction for added length if required.[2]
4. When attaching the FPL tendon to the feeding catheter, a gap is left when suturing the two together. Careful retraction of the feeding catheter with the tendon is then performed.
5. A combination of a two strand modified Kessler core suture and a mattress suture was used with a 3/0 prolene suture. A running epitendinous repair with 4/0 prolene was performed.
We tested our repair on table by flexing and extending the thumb IPJ five times, and ensured tendon gliding and excursion was not compromised. The thumb was splinted with a dorsal blocking splint in slight IPJ flexion. If on table tendon rupture or inadequate tendon excursion and gliding occurs despite the techniques performed above, a two-stage tendon reconstruction is then indicated.
Declarations
Authors’ contributionsManuscript preparation: C.Y.Y. Loh, A. Tan
Manuscript review: M. Tare
Financial support and sponsorshipNone.
Conflicts of interestThere are no conflicts of interest.
Patient consentObtained.
Ethics approvalNot required.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Loh CYY, Tan A, Tare M. Tips and tricks for getting more out of your delayed primary repair of ruptured flexor pollicis longus tendon. Plast Aesthet Res 2017;4:135-6. http://dx.doi.org/10.20517/2347-9264.2017.43
AMA Style
Loh CYY, Tan A, Tare M. Tips and tricks for getting more out of your delayed primary repair of ruptured flexor pollicis longus tendon. Plastic and Aesthetic Research. 2017; 4: 135-6. http://dx.doi.org/10.20517/2347-9264.2017.43
Chicago/Turabian Style
Loh, Charles Yuen Yung, Alethea Tan, Makarand Tare. 2017. "Tips and tricks for getting more out of your delayed primary repair of ruptured flexor pollicis longus tendon" Plastic and Aesthetic Research. 4: 135-6. http://dx.doi.org/10.20517/2347-9264.2017.43
ACS Style
Loh, CYY.; Tan A.; Tare M. Tips and tricks for getting more out of your delayed primary repair of ruptured flexor pollicis longus tendon. Plast. Aesthet. Res. 2017, 4, 135-6. http://dx.doi.org/10.20517/2347-9264.2017.43
About This Article
Copyright
Data & Comments
Data

 Cite This Article 0 clicks
Cite This Article 0 clicks










Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.