Augmentation mastopexy and augmentation mammoplasty: an analysis of 1,406 consecutive cases
Abstract
Aim: Simultaneous augmentation mastopexy is a challenging operation for esthetic plastic surgeons. Complication and revision rates following augmentation mammoplasty or mastopexy are less commonly seen when these two procedures are performed separately. However, when the two procedures are combined, the complication rate is reported exponentially higher when compared with its individual component carried out separately. The current retrospective chart review is a comparative analysis of the two procedures performed by a single surgeon.
Methods: Retrospective data were collected using patient’s charts. All patients who had augmentation mammoplasty (Group A) or simultaneous augmentation with mastopexy (Group B) in muscle splitting biplane using round cohesive gel textured silicone implants by a single surgeon were included.
Results: A total of 1,406 patients had consecutive augmentation mammoplasty or simultaneous augmentation mastopexy. Augmentation mammoplasty (Group A) included 1,298 and simultaneous augmentation with mastopexy (Group B) had 108 patients, respectively. The mean age of the patients in Group A and B was 29.6 years and 32.2 years, respectively (P = 0.006). The mean size of the implants in Group A and B was 340 mL and 308 mL (P = 0.001), respectively. Wound infection in Group A and B was seen in 0.6% and 3.7%, respectively. Wound breakdown was seen in 1.1% in Group A as compared to 6.5% in Group B (P = 0.001). Revision surgeries were performed in 1.4% and 11.1% of Group A and B, respectively (P = 0.001).
Conclusion: There was a statistically and clinically significant higher rate of complications and revision rate noted in simultaneous augmentation with mastopexy (Group B) as compared to augmentation mammoplasty alone (Group A). However, the rise in complications rate is sum of the complications of the two individual components performed and not exponential.
Keywords
Introduction
Augmentation mammoplasty and simultaneous augmentation mastopexy constitute a vast majority of the esthetic procedures.[1] With the rise in a total number of procedure, a rise in total revisions is expected by a plastic surgeon.[2] Earlier complications leading to revision surgery following primary augmentation mammoplasty is generally low with a very high satisfaction rate.[3] A 3-year revision rate following primary mammoplasty has been reported between 0%, 1.97%, and 15% for silicone and 13.2% for saline filled implants.[3-6] In studies with a follow-up spanning between 6 and 12 years, revision rate has been reported between 0% and 1.2%.[7,8] However, long-term 25 years study has shown a revision rate of 15.5% following primary augmentation mammoplasty.[9] On the other hand, revision rate following simultaneous augmentation mastopexy is considerably higher. The reported revision rate may vary from 0%, 16.7%, and 25.8% respectively, depending on the duration of the study and follow-up.[10-12] In both groups of patients, there is a noticeable time-dependent increase in the revision rate. The current article is an analysis of 10-year data in which 1,406 consecutive cases of augmentation mammoplasty and simultaneous augmentation mastopexy using single technique was eviewed for an early comparative complications and revisions rate. The results confirm that when augmentation mastopexy is carried out as a single procedure, it carries a higher rate of complication when compared with augmentation mammoplasty performed alone. However, the higher number of early complications seen in the combine procedure is the addition of the 2 distinctively individual procedures and not an exponential rise.
Methods
Retrospective data were collected using patient’s charts. All patients who had augmentation mammoplasty and simultaneous augmentation mastopexy in muscle splitting biplane using round cohesive gel textured silicone implants performed by author were selected. Patients were divided in Group A, which included augmentation mammoplasties alone, and Group B, who had simultaneous augmentation mastopexy.
All patients were operated under general anesthetic with full muscle relaxation and with their arms abducted and supported at an angle less than 90°. A single dose of intravenous cephalosporin was given to all patients at induction time. Augmentation mammoplasty is performed using inframammary incision, and periareolar, vertical or wise pattern scars were used for augmentation mastopexy depending on the preoperative measurements and wishes of the patient. Muscle splitting submuscular pocket was used for implant placement and procedure is performed as a day case. Drains were used in the earlier part of the study period. All patients wore support brassiere for 3 weeks as a routine.
Earlier complications related to wound infection, wound breakdown, hematoma, periprosthetic infection, use of drains, and size of the implants between the two groups were compared.
The data analysis was done. The results were given in the text as mean ± standard deviation for quantitative/continuous variables and percentages for qualitative/categorical variables. Two-tailed independent t-test is used for statistical significance between groups for quantitative/continuous variables and Chi-square/Fischer exact test for qualitative/categorical variables between groups. In all statistical analysis, only P < 0.05 is considered significant.
Results
A total of 1,406 patients had augmentation mammoplasty and augmentation mastopexy in muscle splitting submuscular pocket by a single surgeon using round cohesive gel textured silicone implants. Group A included 1,298 augmentation mammoplasties, and Group B had 108 simultaneous augmentation mastopexy. The mean age of the patients in Group A and B was 29.6 ± 8.62 years (range: 18-67 years) and 32.2 ± 9.50 years (range: 18-67 years), respectively (P = 0.006). Mean follow-up was 4.5 years (range: 3 months to 10 years). Mean size of the implants in Group A and B was 340 ± 56.7 mL (range: 200-630 mL) and 308 ± 76.0 mL, respectively (range: 200-555 mL) (P = 0.001) [Table 1]. Wound infection in Group A and B was seen in 0.6% and 3.7%, respectively (P = 0.010). Wound breakdown was seen in 1.1% in Group A as compared to 6.5% in Group B (P = 0.001). Hematoma was seen in 0.9% and 0% in Group A and B, respectively. Drains were used in 5.5% and 23.1% of Group A and Group B, respectively (P = 0.001). Revision surgeries were performed in 1.4% and 11.1% of Group A and B patients, respectively (P = 0.001). Three patients developed late seromas in augmentation mammoplasty group, and all were treated conservatively without any recurrence. A total of 5 patients were treated for Grade IV capsular contracture, of these patients, 4 (0.32%) belonged to the augmentation mammoplasty and 1 (0.9%) from augmentation mammoplasty. There were no cases of deep venous thrombosis, pulmonaryembolism, or death in the series.
Relative age and implant size distribution between two groups
| Group A (1,298) | Group B (108) | P | |
|---|---|---|---|
| Age (years) range, (mean ± SD) | 18-67 (29.6 ± 8.62) | 18-67 (32.2 ± 9.50) | 0.006 |
| Mean implant size (mL) range, (mean ± SD) | 200-630 (340 ± 56.7) | 200-555 (308 ± 76) | 0.001 |
Discussion
Simultaneous augmentation mastopexy has been cited as a technically demanding procedure with unpredictable outcome with high nipple and skin flap necrosis, however, a later article by the same author reported satisfactory results.[13,14]
Complications of augmentation mammoplasty and simultaneous augmentation mastopexy may require a planned or an unplanned theater visit for surgical intervention. Common early complications requiring surgical intervention are hematoma and periprosthetic infection. In current series, the hematoma in Group A was seen in 12 patients (0.9%). There were no hematomas seen in Group B when compared with a rate of 0.6% of hematoma in a large series of simultaneous mastopexy with augmentation mammoplasty.[15]
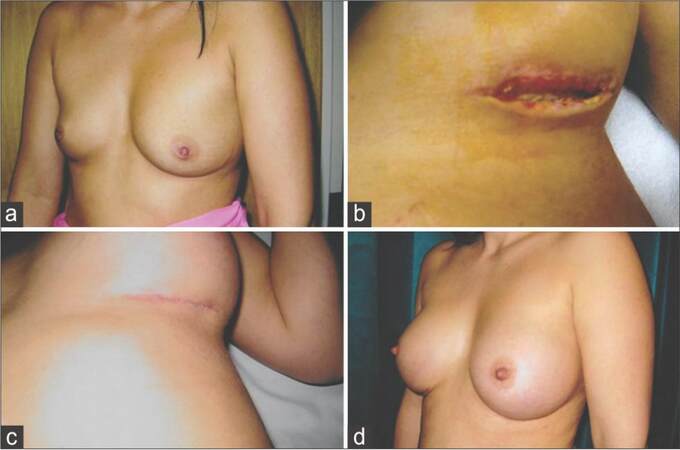
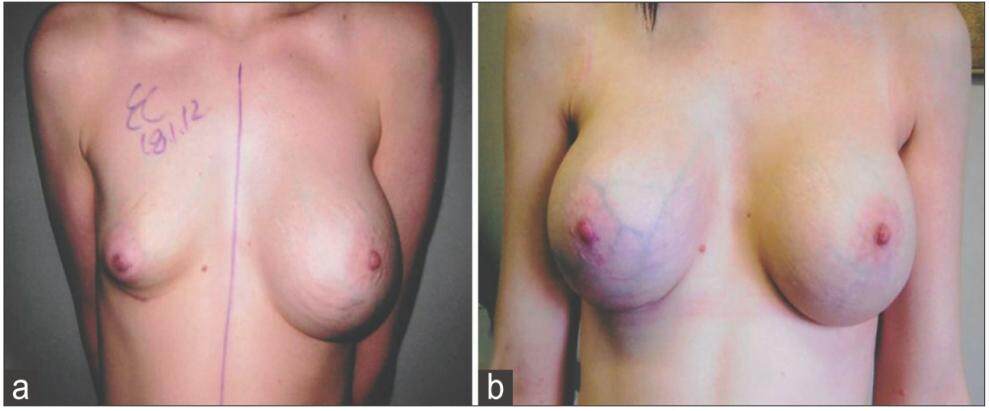
Periprosthetic infection rate has been reported for primary and secondary mammoplasties, respectively.[2,16] Wound breakdown of varying degree was less common inaugmentation mammoplasty as compared to augmentation mastopexy [Figures 1 and 2, Table 2].
Complications between the two groups
| Group A (1,298) (%) | Group B (108) (%) | P | |
|---|---|---|---|
| Wound breakdown | 14 (1.1) | 7 (6.5) | 0.001 |
| Hematoma | 12 (0.9) | 0 | - |
| Revision surgery | 18 (1.4) | 12 (11.1) | 0.001 |
| Grade IV capsular contractures | 4 (0.3) | 1 (0.92) | |
| Periprosthetic/wound infection | 8 (0.6) | 4 (3.7) | 0.010 |
Figure 1. (a) Preoperative picture of a patient interested in augmentation mammoplasty; (b) postoperative picture showing left inframammary wound break down 4 weeks following augmentation mammoplasty when 300 mL round textured cohesive gel silicone implants were used; (c) completely healed wound following conservative treatment; (d) final result 3 months following augmentation mammoplasty
Figure 2. (a) Two weeks following simultaneous mastopexy with augmentation using 230 mL low profile round textured cohesive gel silicone implants showing left partial nipple necrosis; (b) right vertical scar breakdown in the same patient; (c) postoperative pictures taken 4 months following conservative treatment with regular change of dressings and wound cleansing
In current series, periprosthetic and wound infection were seen less commonly in augmentation mammoplasty when compared with augmentation mastopexy [Figure 3, Tables 2 and 3].
Management of early complications
| Procedure (n) | Hematoma | Periprosthetic/wound infection | Wound breakdown | |||
|---|---|---|---|---|---|---|
| Surgical | Conservative | Surgical | Conservative | Surgical | Conservative | |
| Group A (1,298) | 2 | 10 | 6 | 2 | 0 | 14 |
| Group B (108) | 0 | 0 | 0 | 4 | 0 | 7 |
Figure 3. (a) Postexplantation picture of a patient who developed right periprosthetic infection following augmentation mammoplasty; (b) results following reimplantation using 360 mL round textured cohesive gel silicone implants 6 months after explantation
Implant size selection is an important part of the surgery, especially when a vertical scar or wise pattern markings are used for primary mastopexy augmentation [Table 1]. The skin envelope reductions in later two procedures limit the size of the implants in primary procedures and is due to the direct pressure and tension on newly sutured wounds exerted by expanded skin envelope.
The high number of complications or revision rate in combined augmentation with mastopexy is not exponential as reported in the past.[15] The simple reason is that, in patients with augmentation mammoplasty alone, the known early complications are infection and hematoma [Table 4]. In this group, nipple areolar complex (NAC) size and level asymmetry, NAC level under or over positioning, ischemia and necrosis of nipple, loss of nipple sensation, skin and wound breakdown, and scar-related complications are not seen [Table 5]. Similarly, when a mastopexy alone is performed, capsular contracture, implant rupture, revision for size change, rippling, change for size, or other device-related complications are not the reason for revision surgeries. When the two are combined together, the incidence is likely to be higher than the single component performed separately. A long-term follow-up has shown a revision rate of 15.5% when silicone gel round textured implants were used alone,[9] and a long-term tissue-related revision rate of 8.6% is reported when mastopexy alone was performed.[11] A revision rate of 10% and 25.8% has been shown in simultaneous augmentation mastopexy.[11,17] Although the revision rate in augmentation mastopexy is statistically significant, the increased rate of revision is simply the sum of the two individual components.
Reasons for revisions in augmentation mammoplasty group
| Reason for revision | n (%) |
|---|---|
| Capsular contracture | 4 (0.3) |
| Hematoma | 3 (0.23) |
| Explantation and replantation later for infection | 3 (0.23) |
| Debridement, curettage, lavage and immediate implant replacement for infection | 3 (0.23) |
| Explantation without replacement | 2 (0.15) |
| Bottoming out unilateral | 1 (0.07) |
| Explantation with mastopexy | 1 (0.07) |
| Bottoming out bilateral | 1 (0.07) |
Reasons for revision surgery in mastopexy with augmentation
| Reason for revision | n (%) |
|---|---|
| Dog ear bilateral | 2 (16.7) |
| Dog ear unilateral | 2 (16.7) |
| Areolar scar revision | 2 (16.7) |
| Periareolar to vertical scar conversion | 2 (16.7) |
| Nipple level asymmetry | 1 (8.3) |
| Capsular contracture | 1 (8.3) |
| Vertical scar revision | 1 (8.3) |
| Bottoming out | 1 (8.3) |
In a retrospective study performed by Calobrace, it was reported that tissue-related reoperation rate in combined procedures was 13.6% as compared to 10.2% for mastopexy alone. Whereas the implant-related reoperation rate was only 9.6% when the procedure was performed alone as compared to 19.4% reoperation rate in Mentor 6 years core data.[6,18]
Earlier concerns about the safety of the procedure with exponential complication and revision rate were further reviewed by Swanson in a prospective study in which consecutive cases of augmentation mammoplasty, simultaneous augmentation mastopexy, and mastopexy alone were analyzed. A single surgeon did all procedures, all implants were placed in a submuscular pocket, and all mastopexies were performed using vertical scar with superomedial flaps. There was a revision rate of 20.5%, after augmentation mastopexy, 10.7% in augmentation, and 24.6% in mastopexy alone.[19] Again the results support the argument for a combine procedure than to stage the procedure without an added risk of higher complication. When the procedure is staged, the second operation rate is 100%, with two visits to hospital, two costs of individual procedures, and two lots of recovery time from each procedure.
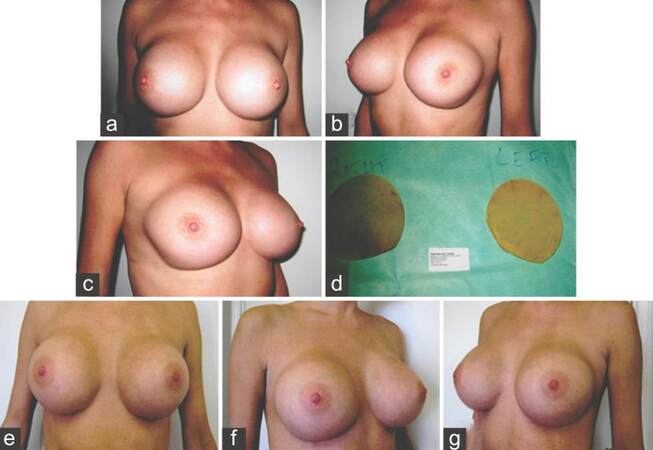
Late complications following simultaneous mastopexy with augmentation mammoplasty and augmentation mammoplasty are mostly implant-related and include capsular contracture, rippling, and device failure. The complications related to implants are not unique to each individual procedure and are shared between the two. The revision for capsular contracture being the most common reason for reoperation in both these groups [Figure 4]. In general, capsular contracture and device failures are time dependent and longer the follow-up, higher the incidence resulting in revision surgery.
Figure 4. (a-c) A patient presenting with bilateral Grade IV capsular contracture following augmentation mammoplasty; (d) explanted implant showing bilateral fold flaw failure; (e-g) three months postoperative pictures following bilateral capsulectomy and change of prosthesis using 460 mL textured round cohesive gel silicone implants
Rippling in the lower pole is almost unavoidable and largely depends on the type of implant and existing breast envelope thickness. Breast augmentation in subglandular pocket, regardless of the preoperative tissue thickness, tends to have a higher revision rate for rippling due to the ever-changing breast envelope thickness.[20] One very important tissue-related and avoidable complication following augmentation mastopexy is the siting of nipple and the choice of the markings. Choice of marking can vary from 65% areolar to 100% vertical scar markings.[18,21] Inappropriate marking for neo-NAC positioning, either too low or too high, also may result in persistent ptosis or bottoming out.[21] In authors experience, use of periareolar markings should ideally be limited for unilateral mastopexy with asymmetrical nipple areolar level and with a difference of not more than 2 cm or patients presenting with early ptosis with an NAC at inframammary crease level. A breast with skin excess in horizontal excess, a breast with a wide base, or a breast with lower pole skin excess, periareolar skin excision from above the nipple does not address the tissue excess and result in less than optimal outcome. Bottoming out following mastopexy using vertical scars in patients presenting more than 9 cm distance from nipple to inframammary crease is a common observation. Nipple elevation to another few centimeters results in increased and above average nipple to inframammary crease length leading to bottoming out. Vertical scar markings selection for all mastopexies or augmentation mastopexies as all-season markings is a novel idea but should be used with caution. Lower pole redundancy or persistent ptosis has been reported in 28% of all the mastopexies when vertical scar mastopexy alone was used for all types of mastopexies.[19] Other published studies also have shown that use of periareolar mastopexy or vertical scars markings was one of the leading cause for revision surgery in this group of patients.[22,23]
The current article did not include authors own mastopexy alone revision rate and results. Therefore, based on the study design, our conclusion has limitation. However, previously published data of mastopexy alone has been used, and our data correlate with what has been published. Furthermore, there was no patient satisfaction survey included that would have indeed added strength to the outcome analysis.
In conclusion, there was a statistically and clinically significant higher rate of complications and revision rate in simultaneous augmentation with mastopexy (Group B) as compared to augmentation mammoplasty alone (Group A). However, the overall revision rate in simultaneous augmentation with mastopexy was lower is actually a total sum of its two individual and distinct component and not exponential.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
1. The American Society for Aesthetic Plastic Surgery's Cosmetic Surgery National Data Bank: Statistics; 2013. Available from:http://www.surgery.org/media/statistics. [Last accessed on 2015 Oct 09].
2. Khan UD. Secondary augmentation mammoplasties and periprosthetic infection: a three-year retrospective review. Aesthet Surg J 2012;32:465-73.
3. Tebbetts JB. Achieving a zero percent reoperation rate at 3 years in a 50-consecutive-case augmentation mammoplasty premarket approval study. Plast Reconstr Surg 2006;118:1453-7.
4. Khan UD. The impact of preoperative breast implant selection on the 3-year reoperation rate. Eur J Plast Surg 2013;36:503-10.
5. Cunningham B. The mentor core study on silicone memorygel breast implants. Plast Reconstr Surg 2007;120:19S-29S.
6. Mentor Corporation. Saline Filled Breast Implant Surgery: Making an informed Decision. Mentor Corp, Santa Barbara, Calif. Available from: https://www.mentordirect.com.au/sites/mentordirect.com.au/files/doc/79549_Mentor_MID_Brochure_v0.pdf [Last accessed on 2015 Sep 09].
7. Heden P, Bone B, Murphy DK, Slicton A, Walker PS. Style 410 cohesive silicone breast implants: safety and effectiveness at 5 to 9 years after implantation. Plast Reconstr Surg 2006;118:1281-7.
8. Khan UD. Muscle-splitting, subglandular and partial submuscular augmentation mammoplasties: a 12-year retrospective analysis of 2026 primary cases. Aesthetic Plast Surg 2013;37:290-302.
9. Handel N, Cordray T, Gutierrez J, Jensen JA. A long-term study of outcomes, complications, and patient satisfaction with breast implants. Plast Reconstr Surg 2006;117:757-67.
10. Khan UD. Vertical scar mastopexy with cat's tail extension for prevention of skin redundancy: an experience with 17 consecutive cases after mastopexy and mastopexy with breast augmentation. Aesthetic Plast Surg 2012;36:303-7.
11. Stevens WG, Stoker DA, Freeman ME, Quardt SM, Hirsch EM, Cohen R. Is one-stage breast augmentation with mastopexy safe and effective? A review of 186 primary cases. Aesthet Surg J 2006;26:674-81.
12. Discussion. A 15-year experience with primary breast augmentation. Plast Reconstr Surg 2011;127:1301-13.
14. Spear SL, Pelliere CV, Menon N. One-stage augmentation combined with mastopexy: aesthetic results and patient satisfaction. Aesthetic Plast Surg 2004;28:259-67.
15. Stevens WG, Macias LH, Spring M, Stoker DA, Chacón CO, Eberlin SA. One-stage augmentation mastopexy: a review of 1192 simultaneous breast augmentation and mastopexy procedures in 615 consecutive patients. Aesthet Surg J 2014;34:723-32.
16. Khan UD. Breast augmentation, antibiotic prophylaxis, and infection: comparative analysis of 1,628 primary augmentation mammoplasties assessing the role and effi cacy of antibiotic prophylaxis duration. Aesthetic Plast Surg 2010;34:42-7.
17. Khan UD. Augmentation mastopexy in muscle-splitting biplane: outcome of first 44 consecutive cases of mastopexies in a new pocket. Aesthetic Plast Surg 2010;34:313-21.
18. Calobrace MB, Herdt DR, Cothron KJ. Simultaneous augmentation/mastopexy: a retrospective 5-year review of 332 consecutive cases. Plast Reconstr Surg 2013;131:145-56.
19. Swanson E. Prospective comparative clinical evaluation of 784 consecutive cases of breast augmentation and vertical mammoplasty, performed individually and in a combination. Plast Reconstr Surg 2013;132:30e-45e.
20. Khan UD. Selection of breast pocket using pinch test in augmentation mammoplasty: can it be relied in long term? Aesthetic Plast Surg 2009;33:780-1.
21. Spear SL, Boehmler JH 4th, Clemens MW. Augmentation/mastopexy: a 3-year review of a single surgeon's practice. Plast Reconstr Surg 2006;118:136S-47S.
22. Mugea TT, Schifmann MA. Aesthetic Surgery of the Brest. 1st ed. Berlin, Heidelberg: Springer-Verlag; 2015. pp. 649-56.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Khan UD. Augmentation mastopexy and augmentation mammoplasty: an analysis of 1,406 consecutive cases. Plast Aesthet Res 2016;3:26-30. http://dx.doi.org/10.20517/2347-9264.2015.67
AMA Style
Khan UD. Augmentation mastopexy and augmentation mammoplasty: an analysis of 1,406 consecutive cases. Plastic and Aesthetic Research. 2016; 3: 26-30. http://dx.doi.org/10.20517/2347-9264.2015.67
Chicago/Turabian Style
Khan, Umar Daraz. 2016. "Augmentation mastopexy and augmentation mammoplasty: an analysis of 1,406 consecutive cases" Plastic and Aesthetic Research. 3: 26-30. http://dx.doi.org/10.20517/2347-9264.2015.67
ACS Style
Khan, UD. Augmentation mastopexy and augmentation mammoplasty: an analysis of 1,406 consecutive cases. Plast. Aesthet. Res. 2016, 3, 26-30. http://dx.doi.org/10.20517/2347-9264.2015.67
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 5 clicks
Cite This Article 5 clicks













Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.