Septal perforation
Abstract
Aim: This study isolates septal perforations due to nasal surgery for clinical analysis and their effect on bilateral mucosal flap repair.
Methods: This is a retrospective review of a single surgeon’s 20-year experience with endonasal perforation repair utilizing bilateral mucosal advancement flaps supported with an autologous tissue interposition graft. Patients with a minimum of 4-month postoperative follow-up were included in the study. Comparative analyses of repair failure rates and perforation size of failures between surgical and non-surgical etiologies were performed.
Results: Three hundred ninety-two patients met the criteria for inclusion in the study. The incidence of perforation and prior septal surgery was 40.6%. Overall repair closure in patients with a minimum of 4 months follow-up was 94.8%. Failures were noted in 5.7% of surgical and 4.7% of non-surgical perforation etiologies (P = 0.816). Mean differences in perforation length and height in failed repairs between non-surgical and surgical etiologies
Conclusion: Post-surgical nasal septal perforations can be repaired with a low rate of failure. However, this study found that the size of perforations in failed repairs was significantly smaller in patients with a history of septal surgery, suggesting that prior septal surgery increases the technical difficulty of a bilateral flap perforation repair.
Keywords
INTRODUCTION
Any surgical manipulation of the nasal septum carries the risk of perforation. Procedures that attempt to control epistaxis or excise septal lesions can injure nasal mucosa or underlying cartilage, leading to cartilage devascularization, necrosis, and progression to a full-thickness septal defect. Septal perforation can be a complication of septoplasty, septorhinoplasty, surgical maxillary advancement, and extended endoscopic procedures that utilize a transseptal approach to access skull base pathology. Bilateral tearing of the mucoperichondrium/periosteum and subsequent suboptimal repair is the likely pathogenesis for most of these perforations. Tight septal splinting, nasal packing, and septal hematoma are other surgically related causes of perforation. An incidence of septal surgery perforation etiology ranging from 39% to 86% has been reported[1-6].
The perforated nasal septum is a heterogeneous condition, with management determined by symptomatology, multiple perforation and patient factors, concurrent nasal conditions, and physician experience. Symptoms unresponsive to moisturization and humidification may improve with a septal button prosthesis[7]. Repair of the perforation’s posterior margin or posterior septal resection may be offered to selected patients attempting to reduce symptoms[8,9]. Numerous and varied procedures have been developed to close septal perforations, and success rates exceeding 90% are frequently reported[1-6,10,11]. Techniques utilizing physiologic nasal mucosal advancement or rotation flaps have dominated the collective perforation repair experience since Fairbanks’ 1970 study introducing the bilateral mucosal flap and interposition graft repair[12]. Our primary technique is adapted from Fairbanks’ procedure and utilizes bilateral, bipedicled mucosal advancement flaps developed endonasally to achieve complete defect closure on at least one side[13]. An autologous interposition graft is placed as a third closure layer for repair support and durability.
This study reviews the senior author’s bilateral flap and graft perforation repair technique and isolates for clinical analysis those patients with a perforation and a history of septoplasty or septorhinoplasty who underwent attempted closure. Repair failure rates between perforations of surgical and non-surgical etiology were compared. Surgical challenges potentially encountered when attempting a flap closure following prior septal surgery are discussed. Alternative management options and the objective measurement of perforation symptoms utilizing the NOSE-Perf scale are presented.
METHODS
This retrospective study of the senior author’s (S.F.B.) septal perforation repair experience was approved by the Mayo Clinic Institutional Review Board (IRB 19-0011700). Patients who underwent nasal mucosal bipedicled flap repairs from January 2003 through December 2022 were identified for medical record review and data collection. Repairs utilizing pedicled nasal flaps were excluded from this study. Patient demographics were determined and perforations resulting from septoplasty or septorhinoplasty grouped into a distinct cohort for analysis. Non-surgical perforation etiologies were combined to facilitate a comparative analysis of repair failure rates between surgical and non-surgical etiologies. Patients followed for at least four months postoperatively were included for data collection and analysis. All descriptive analyses and statistical comparisons were completed using SPSS software (version 28.0; IBM Corporation, Armonk, NY, USA). Pearson’s chi-square test statistics, with various contingency table dimensions, were used for between-group comparisons of prevalence (%), while two-sided independent sample t-test was used to compare continuous measures, where applicable. Type 1 error probabilities (P-values) are reported for differences below the conventional alpha level of 0.050.
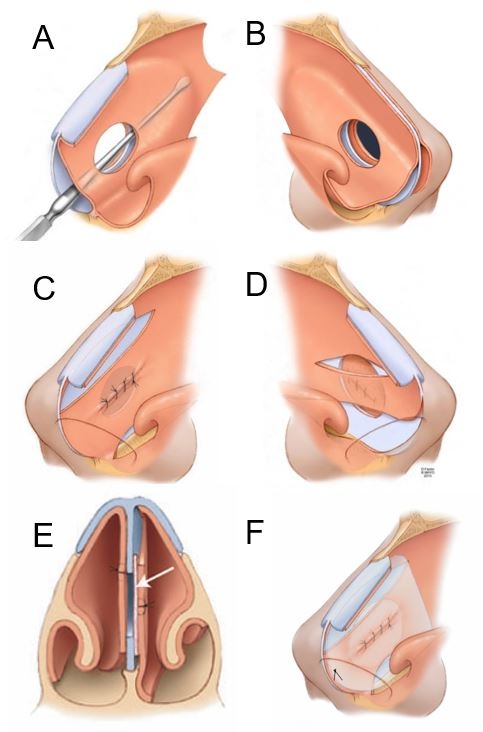
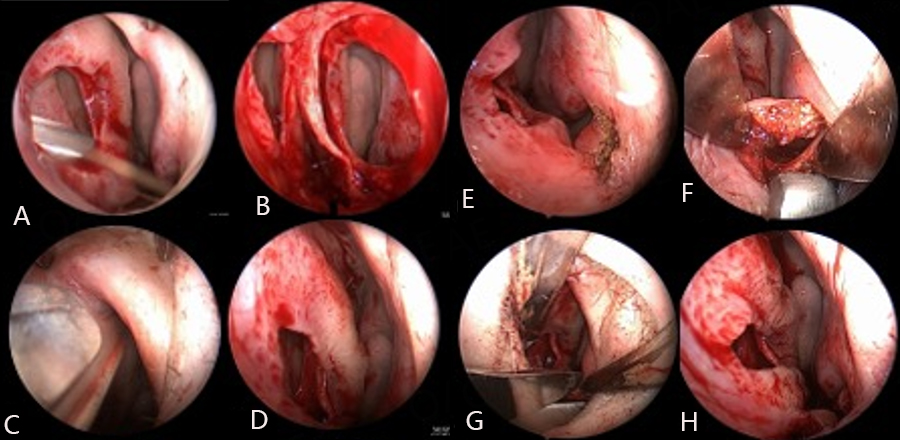
Perforation repair basic technique: Perforation length, height, and distance from the anterior perforation margin to the nasal valve angle and columella are recorded. The fundamental steps in our bilateral flap and graft repair are illustrated in Figure 1. Endoscopic photos of the left side closure are presented in Figure 2. Perforation repair is performed through a right hemitransfixion incision[13]. Mucoperichondrial/periosteal elevation proceeds on the left side through the incised circumference of the perforation margin and then superiorly towards the junction of the upper lateral cartilage (ULC) and septum. Mucosal elevation then proceeds inferiorly and laterally onto the nasal floor as determined by perforation size and position. For larger perforations, the elevation proceeds 2 cm posterior to the posterior margin. Mucosal elevation is then performed on the right side, extending through the perforation and then inferiorly and laterally onto the nasal floor. Elevation superior to the perforation’s superior margin on the right side is avoided. Flap development is first performed on the left side to accomplish complete and tension-free defect coverage. A superior bipedicled advancement flap is developed and, if necessary, an inferior bipedicled flap. The superior flap incision may start anterior to the internal valve angle as determined by perforation size and position. The incision arcs above the perforation and then for 2 cm beyond the posterior margin for larger defects to allow for flap release and advancement. Mucosa from the undersurface of the ULC can be incorporated into this flap through an intercartilaginous incision for larger perforations. The incision for the left inferior flap is made with cautery anterior and inferior to the head of the inferior turbinate. Submucosal elevation proceeds over the piriform aperture to connect to the prior elevation of nasal floor mucosa. The mucosal flap incision is made with a scissors or monopolar cautery, starting laterally at the nasal floor-inferior meatus junction and ending posteriorly at the septum-floor of nose junction 2 cm posterior to the perforation. Anteriorly, sharp undermining dissection through the hemitransfixion incision disrupts the fibrous elements binding mucosa to the nasal spine and premaxilla to allow for flap release and advancement. Superior and inferior flaps are advanced and the collapsed mucosal margins sutured with interrupted 4-0 chromic sutures on a Castroviejo needle holder with a P-3 needle slightly bent to tighten the rotation arc. Suturing of the superior margin of the superior flap to the defect’s superior cartilage margin is performed for flap stabilization when the overlap is tenuous. Attention is then directed back to the right side. A bipedicled advancement flap comprised of mucosa inferior to the perforation and adjacent nasal floor is developed. The hemitransfixion incision is extended posterolaterally onto the nasal floor and then medially to the floor-septum junction posterior to the perforation. This inferior flap is advanced superiorly over the defect to oppose the left suture line closure and support of the interposition graft. A superior flap is not developed for advancement on the right side to avoid bilateral compromise of superior septal cartilage vascularity and the risk of re-perforation. Septal deformities are addressed next, followed by the application of an autologous tissue (temporalis fascia, septal cartilage/bone, or auricular perichondrium) interposition graft. The repair is covered with thin 0.02 in soft polymeric silicone sheeting secured with a single nylon suture placed anteriorly and bolstered with folded pads of Telfa gauze. The packs are removed on postoperative day 2 and the sheeting in 10-14 days [Figure 3]. Frequent saline spray moisturization and ointment lubrication are recommended for 6 weeks post pack removal, and then as indicated for persistent dryness or crusting.
Figure 1. Illustrations of bilateral mucosal flap closure. (A) Extent of septal mucosal elevation on the left side; (B) Elevation superior to the perforation is avoided on the right side; (C) Superior and inferior flaps are advanced and sutured together for a tension-free closure on the left side; (D) The right inferior bipedicled flap is advanced to oppose the left-sided suture line and support the interposition graft; (E) An interposition graft is placed within the septal space to complete the perforation repair; (F) Repair is covered bilaterally with silicone sheeting.
Figure 2. Endoscopic photos of left-side mucosal flap closure. (A) Perforation margin rimmed with #15 blade; (B) Bilateral mucosal flap elevation; (C) Superior incision may extend anteriorly through valve angle; (D) Superior flap advanced inferiorly; (E) Anterior cautery incision for inferior flap; (F) Elevation connecting incision over piriform aperture to previously elevated nasal floor mucosa; (G) Inferior flap incision made with scissors; (H) Flaps advanced to collapse perforation margin for tension-free suture closure; Flaps span (bridge) over the underlying defect’s cartilage margin.
RESULTS
Over the time-period of this study, 433 patients underwent the mucosal flap repair illustrated. Forty-one (9.5%) patients were lost to postoperative follow-up prior to 4 months and were excluded from data collection and analysis, resulting in a study cohort of 392 patients. Patient demographics, mean perforation measurements, and the grouping of perforations into surgical and non-surgical etiology are noted in Table 1. The incidence of surgical etiology was 40.6%.
Patient demographics, perforation size, surgical vs. non-surgical etiology
| Patient (n) 392 |
| Gender Female n (%) 245 (62.5%) Male n (%) 147 (37.5%) |
| Mean age years (range) 49.2 (14-81) |
| Perforation size Mean length mm (range) 14.1 (2-37) Mean height mm (range) 10.5 (2-20) |
| Perforation etiology Surgical n (%) 159 (40.6%) Non-surgical n (%) 233 (59.4%) |
All repairs were performed endonasally. The mean (range) months to last postoperative follow-up was 20.9 (4-192). Overall repair closure rate at minimum 4-month follow-up was 94.8% (372/392). Recurrent perforation was noted in 9 of the 159 (5.7%) surgical etiology patients at last follow-up and 11 of the 233 (4.7%) non-surgical etiology patients (P = 0.816). Differences in perforation mean (± SD) mm measurements between length [non-surgical: 19.4 (± 6.9) vs. surgical: 13.7 (± 5.0)] and height [non-surgical: 15.5 (± 5.2) vs. surgical: 9.3 (± 3.4)] were significant (length: P = 0.048, height: P = 0.006). Information on each failed perforation repair patient at last follow-up is noted in Table 2.
Surgical failures by surgical versus non-surgical etiology
| Surgical etiology | ||||||
| Case | Age (yrs) /sex (m/f) | Etiology | Perforation size length × width (mm) | Postoperative time to failure (months) | Failure size (mm) / Septal position (anterior vs. mid) | Disposition at last follow-up |
| 1 | 40/F | Surgery | 16 × 16 | 2 | 3/mid | Asymptomatic |
| 2 | 51/F | Surgery | 16 × 10 | 4 | 5/ant | Successful second flap closure attempt |
| 3 | 41/M | Surgery | 12 × 10 | 2 | 3/mid | Decreased symptoms |
| 4 | 56/F | Surgery | 13 × 8 | 8 | 4/mid | Decreased symptoms |
| 5 | 28/F | Surgery | 8 × 7 | 2 | 5/ant | Failed second flap closure attempt, symptomatic |
| 6 | 17/M | Surgery | 5 × 4 | 3 | 5/ant | Successful second flap closure attempt |
| 7 | 57/F | Surgery | 15 × 7 | 4 | 3/mid | Asymptomatic |
| 8 | 76/F | Surgery | 16 × 12 | 5 | 14/ant | Symptom improvement following posterior septal resection |
| 9 | 32/M | Surgery | 22 × 10 | 6 | 8/mid | Asymptomatic, revision rhinoplasty 4 years postop |
| Non-surgical etiology | ||||||
| 10 | 60/M | Indeterminant | 26 × 24 | 3 | 2/mid | Asymptomatic |
| 11 | 58/F | Indeterminant | 32 × 21 | 4 | 8/mid | Symptomatic, on conservative treatment |
| 12 | 24/F | Cautery | 28 × 19 | 10 | Symptomatic revision valve surgery performed 6 months postop | |
| 13 | 58/F | Cocaine | 22 × 18 | 4 | 4/mid | Minimal symptoms |
| 14 | 52/M | Decongestant spray | 20 × 18 | 6 | 20/ant | Symptomatic posterior resection offered |
| 15 | 39/F | Granulomatous polyangiitis | 18 × 18 | 4 | 4/ant | Minimal symptoms. Rhinoplasty performed 13 months postop |
| 16 | 69/M | Cauterization | 17 × 14 | 2 | 3/ant | Deceased 4 months postoperative |
| 17 | 57/M | Indeterminant | 15 × 11 | 2 | 4/mid | Symptomatic |
| 18 | 47/F | Steroid nasal spray | 12 × 10 | 6 | 5/ant | Symptomatic |
| 19 | 19/M | Indeterminant | 12 × 8 | 5 | 4/ant | Minimal symptoms, offered second closure attempt |
| 20 | 22/F | Digital trauma | 12 × 10 | 2 | 4/ant | Successful second flap closure attempt |
Eight patients did not have interposition grafts placed at the time of surgery and one of those repairs failed. All patients in this no-graft cohort underwent prior septal surgery.
DISCUSSION
Though caudal end deformities frequently pose the greatest technical challenge to success in septoplasty and functional septorhinoplasty, it is the integrity of the mucosal elevation posterior to the caudal end that determines the risk for perforation. Wide bilateral elevation in the submucoperichondrial/periosteal plane prior to the mobilization and removal of cartilage/bone prevents the tearing or avulsion of mucosa. Intraoperative bleeding is minimized, and surgical visualization maximized, when meticulous dissection is performed in the proper subperichondrial plane. The thin mucosa overlying septal deviations and spurs can be difficult to elevate intact. Mucosal tunnel elevation inferior to the spur with subsequent fracturing of the bone to the opposite side improves the ability to separate mucosa intact from the spur. Endoscopic visualization can improve septal space surgical precision, especially when attempting to separate scarred, adherent mucosa following prior septal surgery[14]. Bilateral and opposing mucosal tears that occur during mucosal elevation increase the risk for perforation, though unilateral tears have been associated with perforation development[15]. We routinely place a mosaic of septal cartilage/bone pieces back into the septal space at the procedure’s conclusion for mucosal flap and airway support. Thin rigid splints are applied for septal stabilization and to minimize hematoma risk. In the presence of bilateral opposing tears, these maneuvers serve to support a unilateral mucosal tear repair. A soft tissue acellular dermal graft is placed in the septal space opposite the repair if bone or cartilage is not available for this purpose. Septal splint application for 7-10 days prevents desiccation to promote mucosal healing. The senior author’s septoplasty experience contributed one patient to this study.
Perforation etiology is not always apparent. Patients may have a history with multiple potential etiologies, or deny any condition associated with perforation development. Perforation patients with a history of septal surgery present with a readily identifiable event that determines etiology which may be clinically relevant when considering management options. Forty-one percent of the perforations in this study were attributed to prior septal surgery.
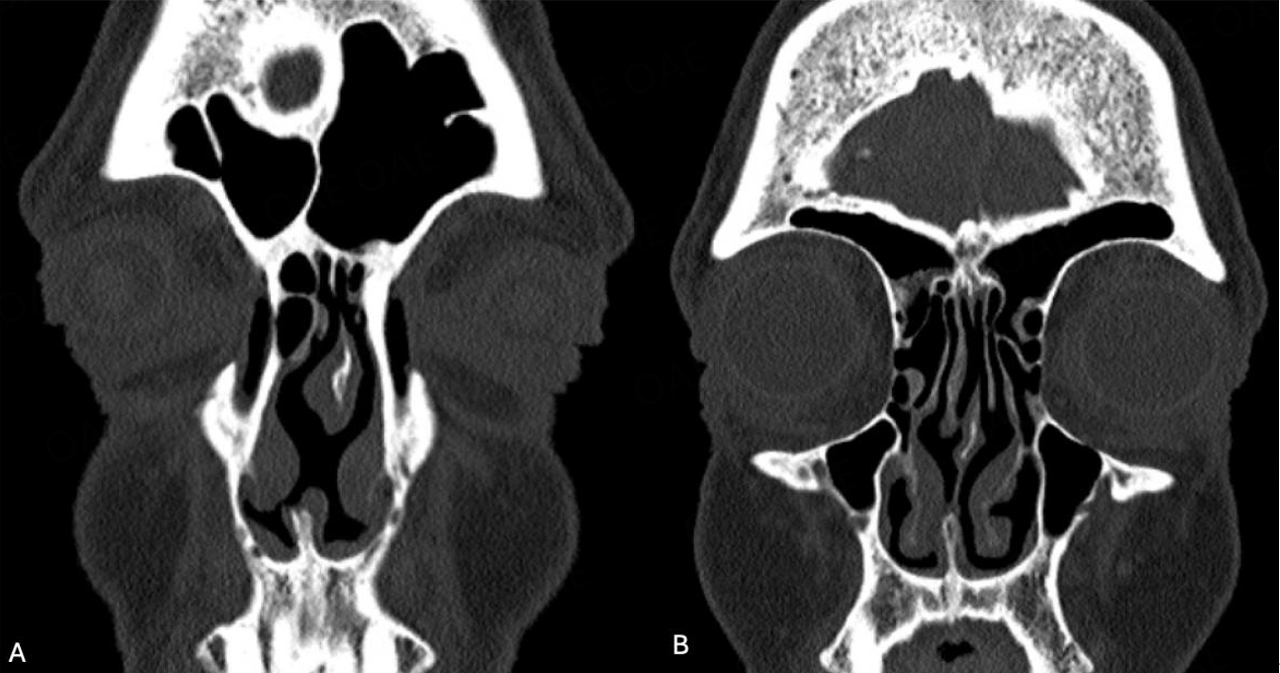
Despite substantial experience in closing perforations, attempted repair remains challenging when prior septal surgery has been performed regardless of the perforation size. Septal scarring due to one or more prior procedures can substantially impact the ability to develop surgical planes for intact mucosal elevation. The removal of bone and cartilage during septal surgery results in densely adherent and attenuated mucosa that can extend for a distance beyond the perforation margin. A slow and tedious dissection is common for perforations resulting from prior septal surgery. This condition is most problematic posteriorly, where a thin margin of fused mucosa can pose a substantial challenge to intact bilateral separation before reaching cartilage or bone located 1 cm or more posterior to the perforation mucosal margin [Figure 4]. Intact elevation of right and left mucosa is facilitated by the injection of saline or local anesthetic to widen the margin sharp separation with a #15 blade. The eight patients in this study for whom an interposition graft was not placed had prior septal surgery. Operative note review described the substantial difficulty in elevating mucosa intact in all patients, resulting in a tenuous single-layer repair that prevented the “interposing” of a tissue graft. The difference in perforation sizes for failed repairs between surgical and non-surgical etiologies noted in this study was significant. These clinical observations and measurement analysis findings support our impression that prior septal surgery increases the technical difficulty associated with flap closure procedures, irrespective of perforation size. The difference in failure rates between surgical and non-surgical (5.7% vs. 4.7%) etiologies found in this study was not significant and may, in part, reflect surgical experience.
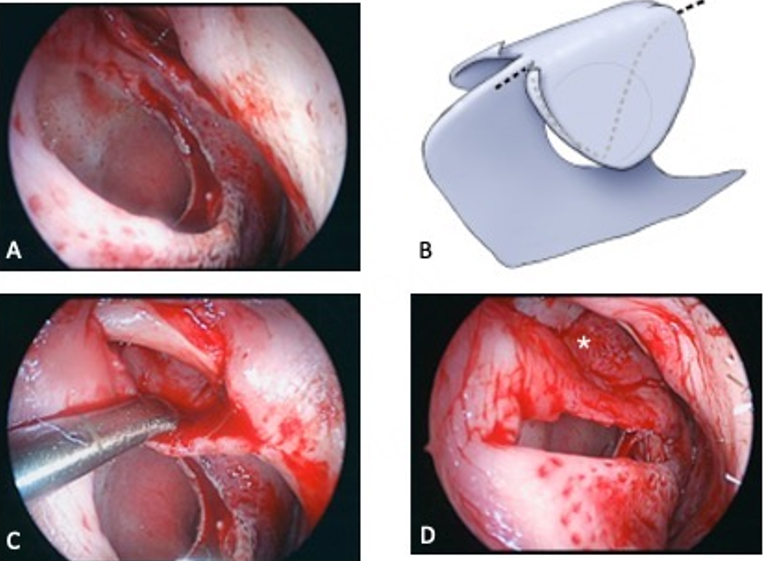
Complete tension-free closure on at least one side is a prerequisite for consistent success in perforation surgery utilizing mucosal flaps. The perforation repair procedure presented emphasizes complete coverage of the septal defect on the left side through the development and advancement of a superior bipedicled flap and, when necessary, an inferior bipedicled flap. The elliptical shape noted for most perforations conforms to a repair utilizing superior and inferior longitudinally oriented flaps. Flap incision placement and the need for an inferior flap are determined by several factors, most notably perforation position and size relative to nasal size. The left superior flap is the most consequential flap in this technique owing to its robust vascularity and thickness, as well as the degree of advancement that can be achieved compared to the inferior flap. Furthermore, mucosa from the undersurface of the ULC can be incorporated into the flap to increase width and achieve complete, tension-free defect coverage for relatively larger (vertical height) perforations and those that approach the internal valve angle[16] [Figure 5]. Prior rhinoplastic surgery, in which the upper lateral cartilages were separated from the septum, with or without spreader graft placement, interferes with the intact elevation of ULC mucosa utilizing an endonasal approach. An alternative, non-incisional technique that utilizes upper lateral cartilage mucosa has been described when using an open approach for the repair[5] [Figure 6].
Figure 4. Computed tomography (CT) scan coronal images of surgical etiology perforation 12 mm length by 9 mm height. (A) Image through perforation; (B) Image through thin posterior margin absent of cartilage; Patient opted for a customized septal button.
Figure 5. Upper lateral cartilage mucosa (ULM) flap. (A) Endoscopic photo of 1.5 × 1.2 cm perforation and intercartilaginous incision; (B) Dashed lines depicting the extent of elevation and incisions connecting to dorsal septum incisions; (C) Endoscopic photo of elevation; (D) ULM flap advanced for suturing; Note the thin ULC mucosa (*) overlapping the superior cartilage margin.
Placement of an interposition graft completes the standard 3-layer repair. The often-stated primary function of the interposition graft is to provide scaffold support for mucosal migration in the event of a suture closure dehiscence or incomplete coverage of the defect’s cartilage margin following flap advancement and suturing. Neovascularization of the graft may improve repair healing[12]. Our choice of autologous temporalis fascia, septal cartilage/bone, or auricular perichondrium is influenced by clinical circumstances[17]. The amount of septal cartilage or bone available for interpositional grafting may be insufficient following septoplasty. Fascia is frequently used for patients with a history of prior surgery or with larger perforations. Temporalis fascia is easily harvested with minimal morbidity and risk. Auricular cartilage that is harvested for concurrent valve or dorsal augmentation surgery can provide a perichondrium graft and avoid a temporal donor site[18]. A review of graft material selection in our bilateral flap repairs found no significant difference between autologous graft application and closure outcomes[17]. Another attempt at closure following a failed repair can be extremely difficult, or impossible. The addition of a graft to a bilateral flap repair poses minimal surgical effort or risk toward the goal of closure success.
Nasal congestion, crusting, and palatal paresthesias are noted by patients during the early postoperative period. The postoperative clinical course generally stabilizes by 6 months. As supported by this study’s findings, we note most repair failures by 6 months. Nasal obstruction may persist following the resolution of postoperative swelling. The development of a unilateral superior flap results in a technique-driven repair asymmetry related to the inferior advancement of physiologic mucosa that may contain thicker nasal swell body tissue[19,20]. Submucosal reduction of the swell body by sharp excision is offered to patients with persistent left-sided obstruction and corroborative exam findings 6 months post repair [Figure 7][19]. We have not noted valve angle scarring with our repairs, though inferior narrowing of the valve area has been infrequently noted. There is a small risk for dorsal saddling following larger perforation repairs. A supratip depression can be noted during the early postoperative period and then progresses over 3-4 months before stabilizing[16]. Nasal dorsum support is compromised in the patient with a large perforation, irrespective of the presence of saddle deformity at presentation. Secondary intention healing and wound contracture at the superior flap donor site places dorsal support at risk. Our study on large perforation repairs that incorporated upper lateral cartilage mucosa into the superior flap found a 4% incidence of delayed saddling[16].
Figure 6. Access to ULC through the open approach. Inset depicts separation of ULC from septum for mucosal elevation. Mucosa advances inferiorly without incisional release.
We developed the NOSE-Perf scale to objectively identify and quantify symptoms associated with perforations[21]. The instrument represents a fusion of the 5 NOSE scale items with 7 additional questions[21,22]. The NOSE-Perf questionnaire has been applied to 117 patients at 6 months or greater postoperatively who underwent the repair procedure presented in this study[23]. Reduction in mean scores of all symptoms measured was noted. Crusting was the most prevalent and severe preoperative, and persistent postoperative, symptom. On a scale where the maximum possible score is 48, significant postoperative reduction (P < 0.001) of mean NOSE-Perf score from 25.3 to 7.9 was realized. All patients noted improvement. The minimal clinically important difference was calculated and 94% of patients had postoperative NOSE-Perf scores greater than the threshold. Patient age, perforation size, or concurrent functional procedures did not impact outcomes. There was no difference in mean scores between successful closures and the 7 (6%) failed repairs, suggesting symptom improvement can occur following repair failure. The mean NOSE-Perf score for the control group in the validation study was 2.2[21]. For most patients, the nose does not normalize following our bilateral, bipedicled flap repair. These results should be interpreted taking into account our practice located in the desert Southwest and the effect of low ambient humidity on perforations and their repairs. We also use the recently revised Glasgow Benefit Inventory (GBI) patient-reported outcomes measurement instrument to assess quality of life 6 months post repair[24]. Analysis of GBI data found significant improvement in quality of life following our bilateral bipedicled flap repairs.
The endonasal bilateral mucosal flap and autologous interposition graft technique described in this study currently accounts for 60% of our repair procedures. We have recently incorporated endoscopically developed anterior ethmoidal artery (AEA) and nasopalatine artery (NPA) flaps into larger (> 10 mm vertical height) repairs[25-27]. These flaps leverage the relatively large quantity of posterior mucosa available on the septum and nasal floor for anterior rotation and suturing to the perforation margin. This closure dynamic contrasts with bipedicled flaps that span, or “bridge” over, the defect. We typically develop the pedicled flap on the right side of the septum to compliment the left-sided bipedicled flap repair, attempting to improve both closure and symptom outcomes for larger perforations.
Figure 7. Nasal swell body. (A) Swell body is thicker opposite the side of septal deviation. Computed tomography (CT) scan showing swell body adjacent to perforation’s superior margin; (B) Endoscopic photo of swell body obstructing valve area post repair; (C) Submucosal elevation with #15 blade to isolate swell body tissue (*); (D) Improved nasal airway following swell body reduction.
Multiple studies have been published on mucosal regeneration and migration procedures for perforation repair[28-30]. Though different grafts have been used, a construct of superficial temporoparietal fascia (TPF) wrapped around a thin supportive plate of polydioxanone (PDS) has emerged as the preferred graft[31-33]. This technique places the responsibility for repair success on regrowth and migration of mucosa over a tissue scaffold. The rationale for mucosal migration repairs includes technical ease and a decreased risk of postoperative obstruction compared to mucosal flap procedures.
Recent reviews on septal perforation repair have not found a difference in closure outcomes between mucosal flap single-layer repairs, multiple-layer repairs, regeneration and migration procedures, interposition graft application, or surgical approach (endonasal vs. open)[34,35]. Lack of a standardized approach to perforation assessment and the inconsistent reporting of treatment outcomes were cited in these reviews. Consensus guidelines on the reporting of perforation measurement and etiology, surgical complications, a required postoperative time period for study inclusion, and the objective assessment of symptom outcomes (NOSE-Perf scale) would facilitate the comparative analysis of treatment outcomes.
Aesthetic or functional rhinoplasty performed concurrently with perforation repair increases the surgical challenge. Multiple factors guide a decision on concurrent surgery, including prior surgical history of septoplasty, open vs. endonasal septorhinoplasty, perforation characteristics, extent of the aesthetic deformity, and surgeon preferences for rhinoplasty approach and perforation repair technique. Surgeons experienced in rhinoplasty and perforation repair have reported high rates of closure and patient aesthetic satisfaction with concurrent surgery[2,5]. The open approach provides excellent exposure for the execution of aesthetic and functional structural maneuvers that may be required for the nose with a perforated septum. Both surgeon and patient should understand that the perforation repair is prioritized over rhinoplastic modifications. A disadvantage of the open approach is the weakening of tip support that follows the separation of the medial crura from the caudal septum. The perforated septum rarely contains enough cartilage for the structural support required for open approach tip and dorsum stabilization[5,15]. Substantial saddling, when present, is often associated with columellar retraction, tip rotation and deprojection, and/or valve dysfunction. The caudal septum may be deficient or absent. These deformities are best addressed using costal cartilage grafting. Incision placement for superior flap development in the technique presented subjects these grafts to possible infection. Extensive cartilage grafting performed on an unstable and poorly vascularized foundation and skin-soft tissue envelope concurrent to repair risks a suboptimal aesthetic outcome. We perform conservative aesthetic and valve surgery, when indicated, at the time of perforation repair. Secondary reconstructive open rhinoplasty is recommended 6-12 months following endonasal repair for our patients with large perforations and/or substantial aesthetic/valve deformities at presentation.
Patients who are not interested in perforation repair, or who have a perforation in which an attempt at closure is not feasible, may realize improvement in nasal symptoms following placement of a septal button prosthesis, posterior septal resection, or posterior repair of the perforation margin[7,36-38]. We consider these treatments for selected patients with substantial health issues or who require chronic anticoagulation therapy. Perforations complicated by large size, poor mucosal condition, prior septal surgery, or a prior failed attempt at closure are also candidates for these treatments. Two failed patients noted in Table 2 were offered posterior septal resection. We use custom-designed septal buttons of soft polymeric silicone, attempting to improve fit and tolerance in 10% of patients presenting with symptomatic perforation[39]. Silicone buttons undergo progressive corrosion and generally require replacement within 5 years. Those patients with a repairable perforation who opt for a button prosthesis are informed that the perforation size can increase during its time of application, which can negatively impact the success of future treatment.
This study represents a retrospective review of one surgeon’s septal perforation repair experience. The large cohort size over a 20-year time period provides the best data available to study septal perforations in the context of prior septal surgery and the difficulty encountered when attempting their repair utilizing a bilateral mucosal flap and autologous graft technique. Short postoperative follow-up times pose limitations on septal perforation surgical studies that report a closure success rate. Re-perforation likely occurred in a small number of patients after last evaluation, though it is unlikely subsequent failures would significantly change the findings of this study. Furthermore, this is a single institution experience in the desert southwest which may limit generalizability of the results.
CONCLUSION
Forty-one percent of the perforations in this study were due to prior septal surgery. The perforation repair closure rate utilizing a bilateral advancement flap with interposition graft technique with a minimum of 4-month follow-up was 95%. This study found the sizes of perforations in failed repairs with surgical etiology were significantly smaller than in those of non-surgical etiology. Failure in the bilateral elevation of mucosa, though rare, occurred exclusively in patients with a history of prior surgery. These findings support our clinical observation that prior septal surgery increases the technical difficulty of mucosal flap perforation repairs. This information is important for both surgeons and patients. Multiple and varied options for surgical closure or symptom improvement are available to treat the patient with a perforated septum. Comparative analysis of treatment results would benefit from the establishment of guidelines to standardize perforation evaluation and outcomes assessment.
DECLARATIONS
Author’s contributions
Conceived and designed the study, collected the data, contributed to data analysis, and contributed to writing the manuscript: Bansberg SF, Miglani A
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
Both authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
This retrospective study of the senior author’s (S.F.B.) septal perforation repair experience was approved by the Mayo Clinic Institutional Review Board (IRB 19-0011700); Patient informed consent has been obtained.
Consent for publication
Consent for publication has been obtained.
Copyright
© The Author(s) 2024.
REFERENCES
1. Fairbanks DNF. Nasal septal perforation repair: 25-year experience with the flap and graft technique. Am J Cosmet Surg 1994;11:189-94.
2. Pedroza F, Patrocinio LG, Arevalo O. A review of 25-year experience of nasal septal perforation repair. Arch Facial Plast Surg 2007;9:12-8.
3. Ribeiro JS, da Silva GS. Technical advances in the correction of septal perforation associated with closed rhinoplasty. Arch Facial Plast Surg 2007;9:321-7.
4. Schultz-Coulon HJ. Three-layer repair of nasoseptal defects. Otolaryngol Head Neck Surg 2005;132:213-8.
5. Kridel RWH, Delaney SW. Simultaneous septal perforation repair with septorhinoplasty: a 31-year experience. Facial Plast Surg 2018;34:298-311.
6. Heywood EG, Daoud M, Talawdekar A, Ashraf N, Raghavan U. Surgical closure of nasal septal perforation using mucosal flaps and interposed graft: a case series of 154 patients and literature review. J Laryngol Otol 2021:1-34.
7. Taylor RJ, Sherris DA. Prosthetics for nasal perforations: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 2015;152:803-10.
8. Eng SP, Nilssen EL, Ranta M, White PS. Surgical management of septal perforation: an alternative to closure of perforation. J Laryngol Otol 2001;115:194-7.
9. Beckmann N, Ponnappan A, Campana J, Ramakrishnan VR. Posterior septal resection: a simple surgical option for management of nasal septal perforation. JAMA Otolaryngol Head Neck Surg 2014;140:150-4.
10. Morse J, Harris J, Owen S, Sowder J, Stephan S. Outcomes of nasal septal perforation repair using combined temporoparietal fascia graft and polydioxanone plate construct. JAMA Facial Plast Surg 2019;21:319-26.
11. Castelnuovo P, Ferreli F, Khodaei I, Palma P. Anterior ethmoidal artery septal flap for the management of septal perforation. Arch Facial Plast Surg 2011;13:411-4.
12. Fairbanks DN, Chen SC. Closure of large nasal septum perforations. Arch Otolaryngol 1970;91:403-6.
13. Miglani A, Taylor C, Bansberg SF. Septal perforation repair using bilateral mucosal flaps with a temporalis fascia interposition graft. Laryngoscope 2021;131:1277-80.
14. Eren E, Balcı MK, İşlek A. Analysis of patient- and procedure-related risk factors for nasal septal perforations following septoplasty. Eur Arch Otorhinolaryngol 2022;279:1357-61.
15. Becker DG. Repair of septal perforations in revision septoplasty. Available from: https://www.rhinoplastyarchive.com/articles/septal-surgery/repair-septal-perforations-revision-septoplasty [Last accessed on 10 Apr 2024].
16. Bansberg SF, Taylor CM, Howard BE, Courson AM, Miglani A. Repair of large nasal septal perforations using the upper lateral cartilage mucosal flap. Laryngoscope 2022;132:973-9.
17. Bansberg SF, Taylor CM, Marino MJ, Courson AM, Miglani A. Autologous interposition grafts for mucosal flap septal perforation repair. Facial Plast Surg Aesthet Med 2024;26:111-6.
18. Bansberg SF, Taylor CM, Neel GS. Auricular perichondrium graft for septal perforation repair. Ann Otol Rhinol Laryngol 2022;131:154-8.
19. Ghorab S, Taylor CM, Bansberg SF. The nasal swell body and septal perforation repair. Laryngoscope 2020;130:2795-801.
20. Brake DA, Snider S, Miglani A, Hamilton GS, Bansberg SF. Nasal swell body characteristics in patients with septal perforation. OTO Open 2023;7:e43.
21. Taylor CM, Bansberg SF, Marino MJ. Assessing patient symptoms due to nasal septal perforation: development and validation of the nose-perf scale. Otolaryngol Head Neck Surg 2021;165:739-44.
22. Stewart MG, Witsell DL, Smith TL, Weaver EM, Yueh B, Hannley MT. Development and validation of the nasal obstruction symptom evaluation (nose) scale. Otolaryngol Head Neck Surg 2004;130:157-63.
23. Taylor CM, Bansberg SF, Marino MJ. Validated symptom outcomes following septal perforation repair: application of the nose-perf scale. Laryngoscope 2024;Online ahead of print.
24. Taylor CM, Marino MJ, Bansberg SF. Septal perforation repair quality of life outcomes using the revised 15-item glasgow benefit inventory. Ann Otol Rhinol Laryngol 2023;132:1550-6.
25. Santamaría-Gadea A, Vaca M, de Los Santos G, Alobid I, Mariño-Sánchez F. Greater palatine artery pedicled flap for nasal septal perforation repair: radiological study and case series. Eur Arch Otorhinolaryngol 2021;278:2115-21.
26. Cavada MN, Orgain CA, Alvarado R, Sacks R, Harvey RJ. Septal perforation repair utilizing an anterior ethmoidal artery flap and collagen matrix. Am J Rhinol Allergy 2019;33:256-62.
27. Garaycochea O, Rodríguez Van Strahlen C, Rojas-Lechuga MJ, Alobid I. How to improve the outcomes of anterior septal perforations repair with combined flaps. Laryngoscope 2023;133:1614-7.
28. Ozkul HM, Balikci HH, Karakas M, Bayram O, Bayram AA, Kara N. Repair of symptomatic nasoseptal perforations using mucosal regeneration technique with interpositional grafts. J Craniofac Surg 2014;25:98-102.
29. Jeon EJ, Choi J, Lee JH, et al. The role of temporalis fascia for free mucosal graft survival in small nasal septal perforation repair. J Craniofac Surg 2014;25:e164-6.
30. Conrad DJ, Zhang H, Côté DWJ. Acellular human dermal allograft as a graft for nasal septal perforation reconstruction. Plast Reconstr Surg 2018;141:1517-24.
31. Flavill E, Gilmore JE. Septal perforation repair without intraoperative mucosal closure. Laryngoscope 2014;124:1112-7.
32. Epprecht L, Schlegel C, Holzmann D, Soyka M, Kaufmann T. Closure of nasal septal perforations with a polydioxanone plate and temporoparietal fascia in a closed approach. Am J Rhinol Allergy 2017;31:190-5.
33. Davis SJ, Rossi Meyer M, Misch E, et al. Septal perforation repair using a temporoparietal fascia and polydioxanone plate construct: a multi-institutional analysis. Facial Plast Surg Aesthet Med 2023;25:212-9.
34. Fermin JM, Bui R, McCoul E, et al. Surgical repair of nasal septal perforations: a systematic review and meta-analysis. Int Forum Allergy Rhinol 2022;12:1104-19.
35. McLaughlin EJ, Friedman O. Surgical repair of nasal septal perforations: an update. Curr Opin Otolaryngol Head Neck Surg 2016;24:37-42.
36. Luff DA, Kam A, Bruce IA, Willatt DJ. Nasal septum buttons: symptom scores and satisfaction. J Laryngol Otol 2002;116:1001-4.
37. Davis SJ, Morse JC, Kimura KS, et al. Septal perfoplasty for management of symptomatic nasal septal perforation: an alternative to surgical closure. Facial Plast Surg Aesthet Med 2021;23:103-9.
38. Medikeri GS, Khong GC, Fleming S, Malhotra T, Leong SC. Quality-of-life changes following three-dimensional printing of prosthesis for large nasal septal perforations-our experience of 13 patients. Clin Otolaryngol 2021;46:60-4.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Bansberg SF, Miglani A. Septal perforation. Plast Aesthet Res 2024;11:12. http://dx.doi.org/10.20517/2347-9264.2023.109
AMA Style
Bansberg SF, Miglani A. Septal perforation. Plastic and Aesthetic Research. 2024; 11: 12. http://dx.doi.org/10.20517/2347-9264.2023.109
Chicago/Turabian Style
Bansberg, Stephen F., Amar Miglani. 2024. "Septal perforation" Plastic and Aesthetic Research. 11: 12. http://dx.doi.org/10.20517/2347-9264.2023.109
ACS Style
Bansberg, SF.; Miglani A. Septal perforation. Plast. Aesthet. Res. 2024, 11, 12. http://dx.doi.org/10.20517/2347-9264.2023.109
About This Article
Special Issue
Copyright
Data & Comments
Data

 Cite This Article 0 clicks
Cite This Article 0 clicks













Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.