Twenty years of experience with the rabbit model, a versatile model for tracheal transplantation research
Abstract
Pathologies comprising more than half the length of the trachea are a challenge to the reconstructive surgeon. Innovative tracheal transplantation techniques aim to offer the patient a curative solution with a sustained improvement in quality of life. This review summarizes the authors’ experience with the rabbit as a versatile model for research regarding tracheal transplantation. Because of the segmental blood supply of the trachea, it is not feasible to transplant the organ together with a well-defined vascular pedicle. As such, the key element of successful tracheal transplantation is the creation of a new blood supply. This vascularized construct is created by prelaminating the rabbit trachea heterotopically, within the lateral thoracic fascia. After prelamination, the construct and its vascular pedicle are transferred to the orthotopic position in the neck. This model has become gold standard because of the advantages of working with rabbits, the anatomy of the rabbit trachea, and the reliability of the lateral thoracic artery flap. In this paper, the key elements of surgery in the rabbit are discussed, as well as the tracheal anastomosis and the harvest of the lateral thoracic artery flap. Practical tips and tricks are presented. The data described in this review represent the fundaments of ongoing translational research in the center over the past twenty years.
Keywords
Introduction
Pathologies comprising more than half the length of the trachea are a challenge to the reconstructive surgeon. Innovative transplantation techniques aim to offer the patient a curative solution with a sustained improvement in quality of life. In the nineties, Delaere et al.[1] developed a rabbit model for orthotopic tracheal transplantation following a period of heterotopic revascularization in the lateral thoracic fascia. This animal model has become the gold standard of the authors for research regarding tracheal transplantation. As a result of this benchwork, the first human allogenic trachea was transplanted with withdrawal of immunosuppression in 2008.[2] Since then, 5 more patients have been transplanted in our center.[3,4] This clinical breakthrough, in addition to ongoing translational research in the rabbit model, has contributed to the authors’ experience in the field. To date, over 200 tracheal transplantations in the rabbit have been performed. The authors wish to share their 20 years of experience with this versatile model by discussing the key elements of tracheal surgery in the rabbit, by reviewing key elements of the tracheal anastomosis and the harvest of the lateral thoracic artery flap, and by giving practical examples. The importance of proper revascularization of the construct is emphasized, as it is the authors’ opinion that it is paramount in obtaining a successful tracheal transplantation.
Definitions
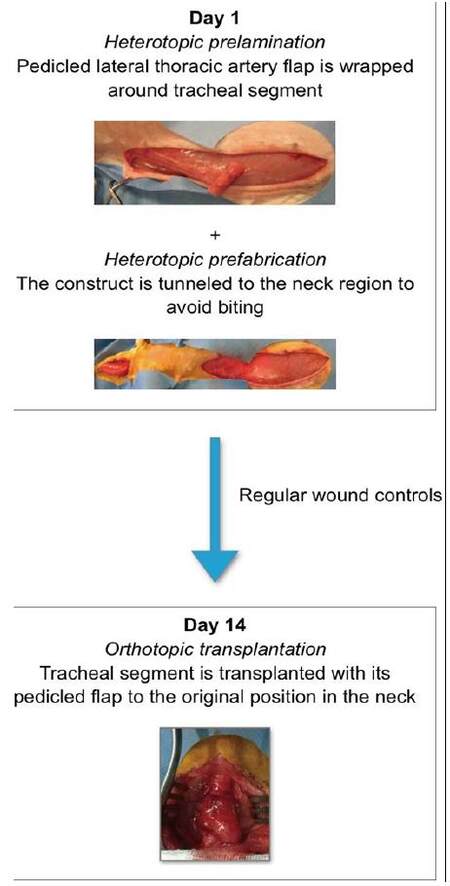
The term prelamination was defined by Pribaz and Fine[5] to describe the implantation of tissue or another device into a vascular territory without manipulation of the blood supply. In a second stage, the construct with its blood supply can be transferred as a pedicled or free flap. As such, it is possible to create a multilayered, vascularized flap. Prelamination is not to be confused with prefabrication, introduced by Yao,[6] which is the implantation of a vascular pedicle into a new territory. After neovascularization, tissue in this territory can be transferred based on the implanted pedicle.
Heterotopic placement of the trachea refers to the temporary placement of the tube in an anatomical location other than its normal position in the neck, for example in the lateral thoracic area. When the trachea is transplanted to its anatomically correct position in the neck, it is referred to as orthotopic position.
Why rabbits?
Numerous advantages are associated to working with rabbits. Rabbits have a long cervical trachea, allowing for easy access to the tube and segmental transplantation. Also, in contrast to larger animals such as pigs or sheep, rabbits are more readily accessible for research purposes and are more convenient to manage. Rabbit cell-surface markers for recognition by the immune system have been mapped out.[7] These rabbits major-histocompatibility complexes are referred to as Rabbit Leukocyte Antigens. Rabbits are phylogenetically closer to primates and have a more diverse genetic background than inbred and outbred rodent strains.[7-9] This makes the model a better overall approximation to humans, mimicking human genetic diversity more accurately. Moreover, the tracheal anatomy of humans resembles that of the rabbit closely. It is also possible to perform tracheoscopy as a monitoring tool following transplantation, and to obtain an adequate tracheal length for epithelial cell-cultivation. Together with the relative cost-effectiveness compared to larger animal models, these characteristics make the rabbit our experimental model of choice.
Tracheal anatomy and blood supply
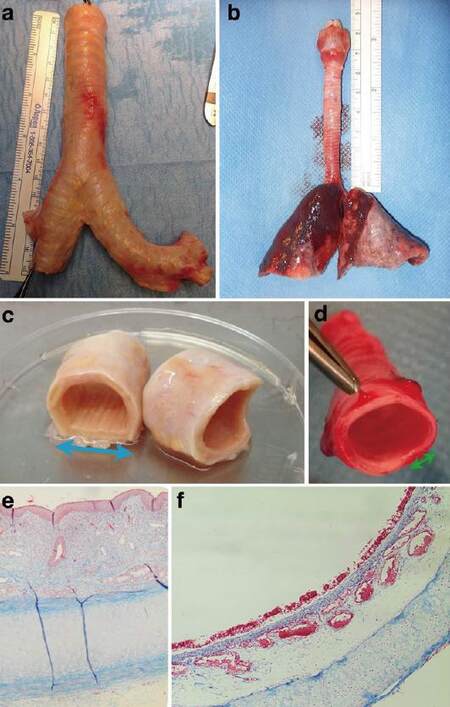
The rabbit trachea is approximately 6.5 cm in length and 0.5 cm in diameter [Figure 1].[10] It is composed of cartilage rings connected by intercartilaginous ligaments anteriorly, and the trachealis muscle posteriorly. Both the cartilage and trachealis muscle contribute to the typical semi-rigid, semi-flexible characteristic of the trachea.
Figure 1. Human vs. rabbit trachea. (a) Human trachea measures 10 cm ± 9 cm;[10] (b) rabbit trachea measures on average 6.5 cm; (c) human cartilage rings comprise two-thirds of tracheal circumference vs. 90% in rabbits (d). The blue (c) and green (d) arrows represent the trachealis muscle; (e and f) Masson's trichrome stain: human trachea (e) contains more submucosal glands, compared to the better-developed submucosal capillaries in rabbits (f)
Hyaline cartilage is composed of an outer layer of highly-organized collagen type I and II fibrils, which provide strength to the construct.[11] This outer layer surrounds a hydrated proteoglycan-core, which is able to resist compression. The rings are connected by fibroelastic ligaments, through which vessels penetrate to create a richly-anastomosing submucosal capillary network. The trachealis muscle shapes the posterior part of the circle. This smooth muscle alters luminal diameter, e.g. during coughing.
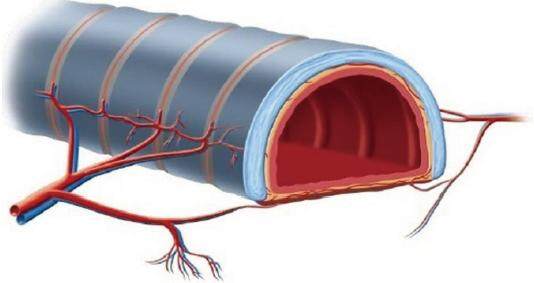
The intrinsic blood supply of the trachea is segmental [Figure 2].[12] As such, unlike other solid organ transplants, a direct microvascular transfer of the organ together with its own vasculature is unfeasible. To solve this problem, the technique of indirect revascularization or prelamination is used.[5,13] The trachea is wrapped with heterotopic tissue that is perfused by an identifiable vascular pedicle, such as the lateral thoracic fascia with the lateral thoracic artery and vein. In a second stage, the trachea and its new vascular pedicle are transferred to the orthotopic position in the neck.
Figure 2. The tracheal blood supply is segmental.[12] Branches from the inferior thyroid, subclavian, internal thoracic, innominate, superior and middle bronchial arteries form two lateral longitudinal anastomoses to supply the anterolateral trachea. These anastomoses give off transverse branches, which penetrate through the intercartilaginous ligaments to feed the submucosal capillary plexus. Cartilage is nourished via diffusion from this plexus. The posterior membranous trachea has an independent vascular supply derived from the oesophageal branches of the above-mentioned large neck vessels
Lateral thoracic artery flap
The authors’ workhorse flap for tracheal revascularization in humans is the free radial forearm flap. The counterpart in the rabbit is the pedicled lateral thoracic artery flap. The lateral thoracic artery flap is composed of subcutaneous fascia with a thin muscular layer, i.e. the panniculus carnosus.[14] This striated muscle is particularly well developed in the trunk of rabbits. In humans, with the exception of remnants such as the platysma, it is almost entirely regressed.
The rabbit’s lateral thoracic artery originates from the external thoracic artery.[14] It travels caudally together with the lateral thoracic vein and nerve, deep to the pectoralis muscle. On the latero-inferior border of the muscle, the artery continues superficially within the thoracoabdominal panniculus carnosus. Around the second to third nipple, the artery anastomoses with secondary branches from the superficial inferior epigastric artery.[15,16] One prominent lateral thoracic vein, which runs parallel to its artery, drains into the axillary vein.
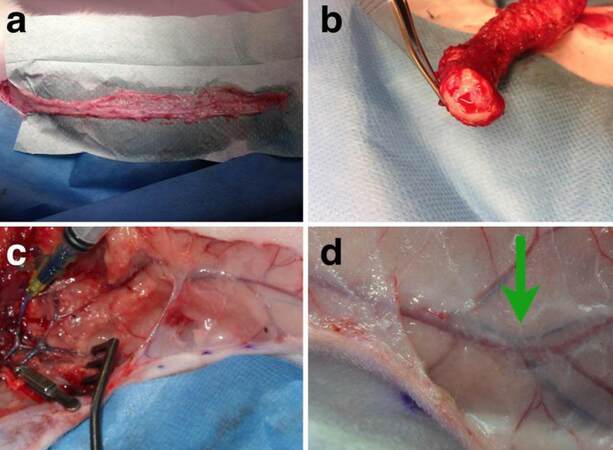
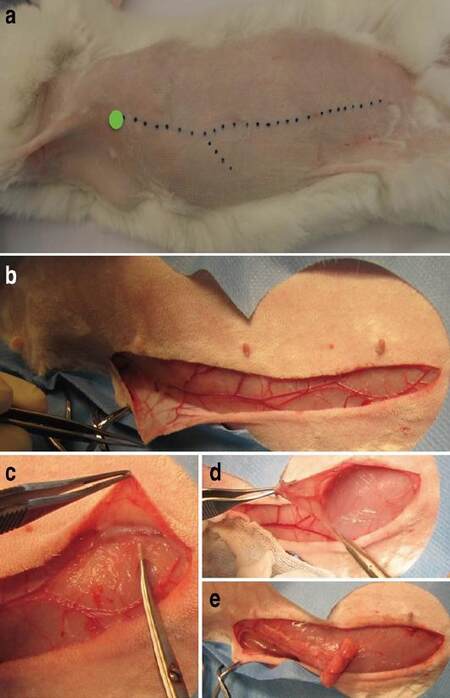
The human lateral thoracic artery has a small caliber and shows anatomical variations.[17,18] Compared to the shorter, variable human lateral thoracic vessels, rabbit vessels in our series (n > 200) had a consistent, long course before anastomosing with the superficial inferior epigastric artery. As in humans, the caliber of the artery is small. Patency and course of the pedicle were demonstrated by isolating the flap for 2 weeks in situ, and by injecting silicone dye into the lateral thoracic artery (Microfil, Flow Tech, Inc., Massachusetts) [Figure 3].
Figure 3. (a) Dissection of the lateral thoracic artery flap. The flap is isolated for 2 weeks within the donor area; (b) patent artery and vein after 2 weeks of flap isolation; (c) injection of silicone dye into the lateral thoracic artery; (d) patent artery with blue silicone dye up to distal from the bifurcation and anastomosis with the superficial inferior epigastric artery (green arrow)
Rabbit anesthesia and euthanasia
Animal handling
All rabbits are treated according to the European Directive on the Protection of Animals. The Ethical Committee for Animal Experimentation of KU Leuven verifies each study protocol. As with any animal, it is important to handle rabbits with care. When lifting rabbits out of their cages, their lower legs are supported to prevent spinal cord injuries secondary to kicking.
Anesthesia
General anesthesia is performed by the researcher after having obtained adequate training skills and qualifications regarding laboratory animal science, the use of anesthetic agents, and monitoring tools.
Adult New Zealand white rabbits, weighing approximately 3 kg, are used in all studies. Rabbits are anesthetized by inhalation of isoflurane. Because of the particular smell of this gas, conscious rabbits will counteract its use. Moreover, induction with isoflurane may cause life-threatening apnea in rabbits.[19] Therefore, proper induction is carried out with the use of xylazine 6 mg/kg and ketamine 40 mg/kg intramuscularly, each injected into 1 gluteal region. The primary function of xylazine is sedation, while ketamine induces dissociative anesthesia. Analgesia is achieved by administering buprenorphine 0.05 mg/kg subcutaneously in the gluteal region. Additional doses are administered every 8 to 10 h, up to 72 h or as needed. Once proper induction is achieved, maintenance gas-anesthesia with isoflurane 1% to 2% supplemented with oxygen 1 L/min is administered by mask ventilation with spontaneous breathing. Rabbits are obligate nasal breathers, and as such, a mask firmly attached around the nose provides adequate inhalation of isoflurane. Rabbits are monitored with pulse oximetry. It is important to work in an adequately-equipped environment with proper ventilation and a scavenging system to minimize spills. Upon orthotopic transplantation, it is useful to have a sterile tube available in the operating field which can be inserted into the distal tracheal segment at the moment that the trachea is opened.
Euthanasia
Rabbits are euthanized by intravenous injection of a lethal dose of T61 0.3 mL/kg into the marginal auricular vein. When the trachea is used for transplantation or in vitro research, it is important to limit warm ischemia time.[20,21] Therefore, opening of the neck is performed under general anesthesia. Only after exposure of the entire tracheal length, is the euthanizing agent administered and the trachea procured.
Operating technique
Tracheal surgery as well as flap dissection can be performed with the rabbit in dorsal decubitus without the need to change position. After achieving proper sedation, the rabbit is shaved and the skin is disinfected with an alcoholic preparation. Both upper legs can be fixed in relaxed extension, taking care to avoid brachial plexus injury caused by overstretching of the limbs.
Tracheal surgery
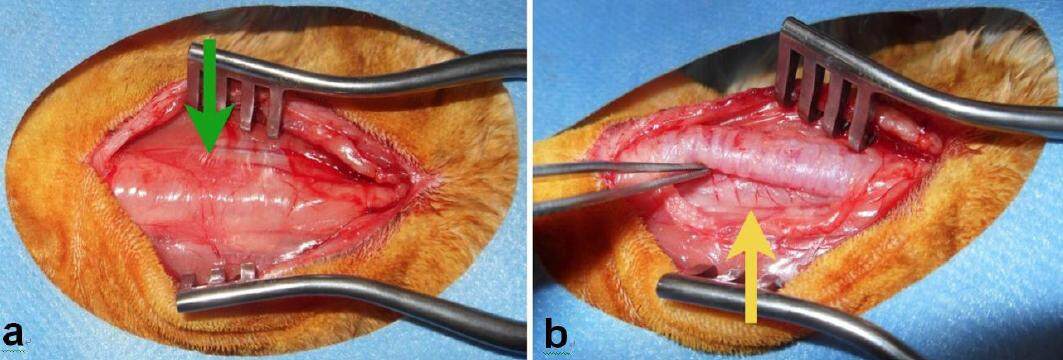
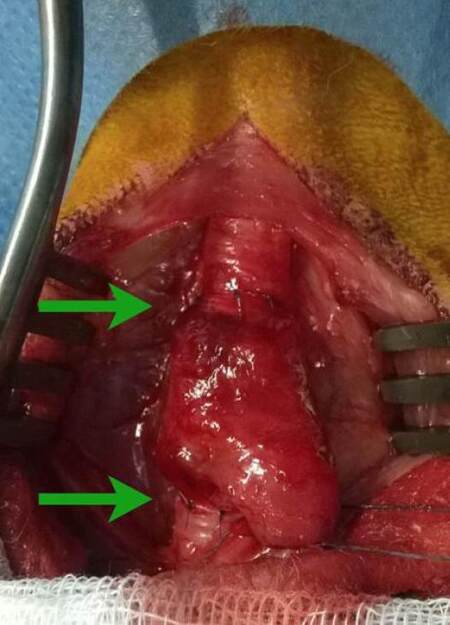
The neck is opened via a vertical midline incision to expose the superficial investing fascia. Deep to this fascia, the paired sternocleidomastoid and strap muscles are divided via their connecting raphe, forming a bloodless plane at the midline. The raphe is opened from the thyroid cartilage to the sternal notch to expose the cervical trachea over its entire length. Upon approaching the sternal notch, the venous jugular arc is encountered, running deep to the distal part of the sternocleidomastoid muscles and crossing the midline. The branch is ligated and an orthostatic retractor is placed to provide adequate exposure [Figure 4]. The trachea is covered by pretracheal fascia. The thyroid gland is also incorporated into this fascia, and can be divided along the midline while opening the fascia longitudinally. The cervical trachea is then circularly detached from the surrounding tissue.
Figure 4. (a) Peroperative view on the pretracheal fascia with the thyroid gland (green arrow), after dividing the strap muscles; (b) image of posterior oesophageal branches (yellow arrow) after opening the pretracheal fascia
The recurrent laryngeal nerve travels within the tracheal-esophageal groove and enters the larynx on the posterior surface of the trachea.[22] The nerve is identified and dissection is pursued close to the trachea to avoid vocal-cord paralysis.
The quality of the anastomosis depends on the degree of exposure, the presence of a bloodless field, and well-prepared tracheal ends. To control both segments, a retraction suture is placed proximal and distal to the segment that will be removed. The circularly-detached trachea is elevated and the desired tracheal length is procured. At this point, a sterile tube providing isoflurane can be placed into the distal native segment. A suctioning device is used to prevent blood from the submucosal capillary plexus of the tracheal ends from leaking into the tube.
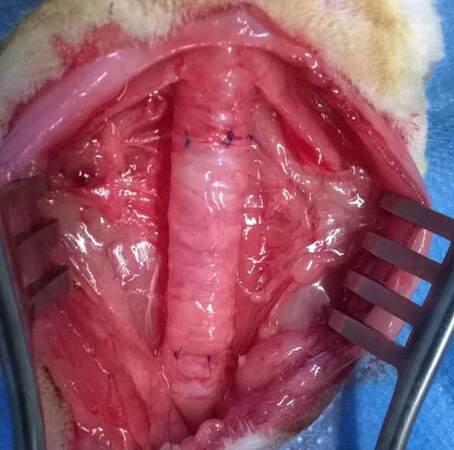
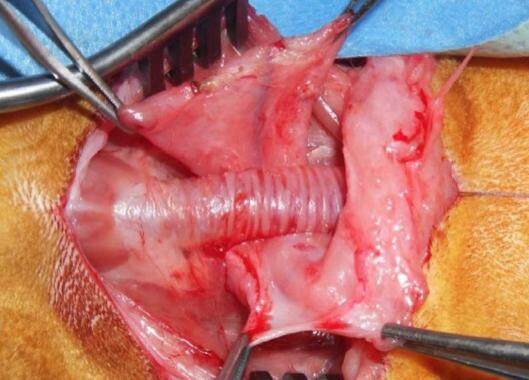
Tracheal anastomosis
The tracheal anastomosis is performed under loop magnification with Prolène 6-0 interrupted sutures [Figure 5]. As with every anastomosis, careful approximation of both segments without overlap is important. To minimize the risk of stenosis, as few sutures as necessary are used to close the gap while preventing the leakage of air. On average, 6 to 7 points per anastomosis are used. If the caliber-difference is substantial, a short vertical incision is made in the narrowest segment to enlarge the diameter. To prevent secondary healing, it is important not to damage the mucosa. Microsurgical tissue handling techniques are used and grasping of the inner lumen with a forceps is avoided.
Figure 5. Peroperative image of autologous rabbit tracheal transplantation. Each anastomosis was closed with 6 points, using interrupted Prolène 6-0 sutures with external knots. The result shows no caliber mismatch
The first two interrupted sutures are placed posteriorly. Full-thickness bites are avoided by passing the suture from externally to the submucosal space. As such, the integrity of the fragile mucosa is preserved, and the risk of stenosis is diminished. Knots are tied externally, as intraluminal knots and suture ends will obstruct airflow. By suctioning the lumen, again without harming the mucosa, stasis of secretions or blood is prevented. Next, the remaining sutures are placed, progressing anteriorly. Once the tube is closed, a tracheoscopy can be performed to check the quality of the anastomosis from the luminal side.
Strap muscles and investing fascia are closed. Rabbits do not tolerate foreign material such as a Penrose drain to prevent possible air trapping. As a preventive measure, loose, interrupted sutures are placed, taking care not to impair flap vascularization. The distal part of the incision is left open for a distance of approximately one centimeter.
Flap dissection
Heterotopic prelamination
After the thoraco-abdominal region has been shaved, the lateral thoracic vessels are easily recognizable [Figures 6 and 7]. The vessels are palpable and visible through the skin. When in doubt, a handheld Doppler can be used to assist in marking the visible portion of the vessels. The point at which the vessels dive deeper to reach the axillary artery is the pivot point of the flap. The length from the pivot point to the native trachea is measured to ensure that the fabricated flap reaches the neck without tension. Extra length is added to the distal part of the flap for tracheal wrapping.
Figure 7. Harvest of lateral thoracic artery flap. The rabbit's head is located on the left. (a) The pedicle is visible throughout the skin after shaving. The pivot point of the flap (green circle) is situated at the latero-inferior border of the pectoralis muscle, where the lateral thoracic artery appears superficially; (b) view on the lateral thoracic artery and vein within the panniculus carnosus, coursing over the thorax (left) and abdomen (right). The lateral thoracic artery anastomoses with the superficial inferior epigastric artery at the level of the third nipple; (c) opening of fascia and panniculus carnosus distally; (d) elevation of the flap from the underlying muscles; (e) heterotopic prelamination of trachea within the lateral thoracic artery flap
The skin overlying the vessels is incised and undermined between the dermis and subcutaneous fascia. Once the correct plane has been identified, dissection proceeds easily from distal to proximal. Operating clips or fine bipolar coagulation are used to divide branches to the skin. Once the length of the flap has been established, the pedicle is divided distally. It is important to preserve enough width of the flap to be able to wrap the desired tracheal length. The flap is elevated from the underlying muscles via the intervening bloodless plane. Elevation is continued towards the pivot point while leaving a cuff of tissue on each side of the pedicle. It is not necessary to skeletonize the pedicle proximally.
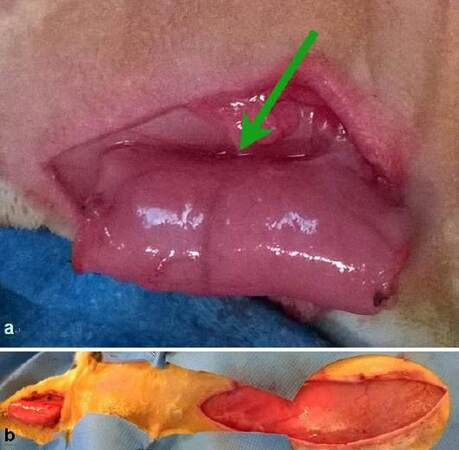
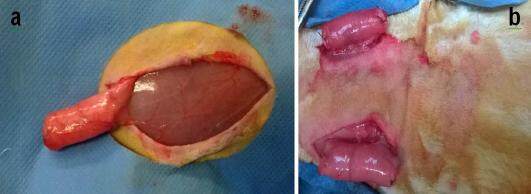
The flap is wrapped around the tracheal tube with its pedicle perpendicular to the longitudinal axis of the trachea to facilitate future orthotopic inset of the tube [Figure 8].
Figure 8. (a) Trachea wrapped within lateral thoracic artery flap, tunneled to cervical incision. The pedicle (green arrow) is oriented perpendicular to the longitudinal tracheal axis. The flap is fixed loosely to the local subcutaneous tissue to prevent dislocation; (b) lateral neck incision with tunneled construct (left) and lateral thoraco-abdominal incision (right), the flap donor site
Rabbits tend to bite wounds in the trunk. To avoid trauma during prelamination, the construct is tunneled with its flap to a lateral neck incision [Figures 6 and 8]. This region is not accessible to biting and has an abundance of excess skin. The technique is a combination of prelamination and prefabrication. The trajectory from the lateral thoracic incision to the neck incision is freed subdermally, creating enough width in the tunnel to prevent flap congestion. The flap is fixated in the neck to avoid dislocation. The incisions are closed with subcutaneous interrupted and intradermal running sutures with buried knots to prevent wound dehiscence secondary to biting.
Orthotopic transfer
Optimal revascularization of autologous trachea is achieved after fourteen days of heterotopic prelamination.[23-25] At this point, the trachea and its flap can be transferred to their orthotopic position in the neck [Figure 9]. Upon inserting the construct, it is important to minimize the amount of tension placed on the flap. This tension can potentially create respiratory distress secondary to kinking of the tube. Proximal and distal anastomoses are performed as described earlier.
Postoperative care
Rabbits are awakened from anesthesia with extra oxygen via mask ventilation and kept warm. Adequate analgesia is provided postoperatively and enrofloxacin is administered in the drinking water upon indication. Tracheoscopy is performed weekly or in case of respiratory distress (2.9 mm, 0°, rigid endoscope, Karl Storz).
Practical examples
Orthotopic prefabrication
To perform studies on vascularized autologous trachea, a native tracheal segment can be wrapped with lateral thoracic fascia prior to manipulation [Figure 10]. After two weeks of prefabrication, the autologous tracheal segment is vascularized and can be manipulated safely on the lateral thoracic pedicle.
Figure 10. Wrapping of an orthotopic tracheal segment within the lateral thoracic artery flap. The native trachea is not manipulated until complete ingrowth of the flap, i.e. after two weeks. After prefabrication, the tracheal segment can be safely manipulated on its pedicle, without the risk of devascularization
Heterotopic prelamination
Regular wound controls are planned during heterotopic vascularization. Every three days the skin is opened and the construct is exposed under general anesthesia. As such, intraluminal tissue-ingrowth and mucus-accumulation are avoided, thereby preventing fibrosis and infection.
For ethical reasons, if orthotopic inset is not planned, two lateral thoracic artery flaps can be used per rabbit to minimize the number of animals used [Figure 11].
Complications and limitations
Complications
Minor complications such as seroma formation can be treated by aspiration of the region of fluctuance. Wound dehiscence is prevented by using intradermal running sutures with buried knots, and by transferring the construct to the neck during heterotopic revascularization. To date, no flap failures have been observed. Three rabbits exhibited flap congestion, which could be corrected by widening the subcutaneous tunnel (1.5%, total n = 200).
Limitations
Although rabbit tracheal anatomy resembles human anatomy closely, the rabbit is not a large animal model. Rabbit trachea contains more submucosal vascular structures, as compared to the more glandular submucosa of human trachea [Figure 1]. Furthermore, the rabbit trachealis muscle encompasses only 10% of the tracheal circumference, in contrast to 30% in humans. Also, it is postulated that rabbits have better developed longitudinal anastomoses along the lateral tracheal wall, as is the case for cats and dogs.[12] Another difficulty in the use of rabbits for study is the application of immunohistochemistry markers in rabbit tissue. Rabbits are commonly used to produce monoclonal antibodies against rodent or human epitopes. As a consequence, appropriate rabbit-specific antibodies are more difficult to find, as they are often produced in the rabbit itself. As in humans, a disadvantage of the rabbit’s lateral thoracic artery is its routinely small caliber, which makes it more difficult for free flap transfer.
Conclusion
This review summarizes our experience with the rabbit as a versatile model for tracheal transplantation research. The advantages of working with rabbits, the anatomy of the rabbit trachea and the reliability of the lateral thoracic artery flap make this model the authors’ gold standard. Additionally, the pedicled lateral thoracic artery flap can be used for various reconstructive procedures and prelamination studies. The data presented in this review represent the fundaments of ongoing translational research in our center over the past twenty years. Because of the segmental blood supply of the trachea, it is unfeasible to transplant the organ together with a well-defined vascular pedicle. As such, the main challenge of successful tracheal transplantation is the creation of a new blood supply. In clinical practice, revascularization of human allotrachea in the radial forearm fascia was enhanced by making incisions in the intercartilaginous ligaments.[3] To further enhance vascularization of transplanted tracheae, the authors are currently investigating pro-angiogenic strategies in their standardized rabbit model.
Financial support and sponsorship
This work was supported by the predoctoral fellowship of the Research Foundation Flanders (FWO) of Dr. Margot Den Hondt.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
1. Delaere PR, Liu ZY, Hermans R, Sciot R, Feenstra L. Experimental tracheal allograft revascularization and transplantation. J Thorac Cardiovasc Surg 1995;110:728-37.
2. Delaere PR, Vranckx JJ, Verleden G, De Leyn P, Van Raemdonck D, Leuven Tracheal Transplant Group. Tracheal allotransplantation after withdrawal of immunosuppressive therapy. N Engl J Med 2010;362:138-45.
3. Delaere PR, Vranckx JJ, Meulemans J, Vander Poorten V, Segers K, Van Raemdonck D, De Leyn P, Decaluwé H, Dooms C, Verleden G. Learning curve in tracheal allotransplantation. Am J Transplant 2012;12:2538-45.
4. Delaere PR, Vranckx JJ, Den Hondt M; Leuven Tracheal Transplant Group. Tracheal allograft after withdrawal of immunosuppressive therapy. N Engl J Med 2014;370:1568-70.
5. Pribaz JJ, Fine NA. Prelamination: defining the prefabricated flap - a case report and review. Microsurgery 1994;15:618-23.
6. Yao ST. Microvascular transplantation of prefabricated free thigh flap. Plast Reconstr Surg 1982;69:568.
8. Graur D, Duret L, Gouy M. Phylogenetic position of the order Lagomorpha (rabbits, hares and allies). Nature 1996;379:333-5.
9. Bosze ZS, Houdebine LM. Application of rabbits in biomedical research: a review. World Rabbit Sci 2006;14:1-14.
10. Kamel KS, Lau G, Stringer MD. In vivo and in vitro morphometry of the human trachea. Clin Anat 2009;22:571-9.
11. Mankarious LA, Adams AB, Pires VL. Patterns of cartilage structural protein loss in human tracheal stenosis. Laryngoscope 2002;112:1025-30.
12. Salassa JR, Pearson BW, Payne WS. Gross and microscopical blood supply of the trachea. Ann Thorac Surg 1977;24:100-7.
13. Vranckx JJ, Den Hondt M, Delaere P. Prefabrication and prelamination strategies for the reconstruction of complex defects of trachea and larynx. J Reconstr Microsurg 2014;30:145-52.
14. Barone R. Comparative anatomy of domestic mammals. Volume 5, Angiology. 2nd ed. Paris: Vigot; 2012. (in French)
15. Delaere PR, Hardillo J. Tubes of vascularized cartilage used for replacement of rabbit cervical trachea. Ann Otol Rhinol Laryngol 2003;112:807-12.
16. Giessler GA, Friedrich PF, Shin RH, Bishop AT. The superficial inferior epigastric artery fascia flap in the rabbit. Microsurgery 2007;27:560-4.
17. Loukas M, du Plessis M, Owens DG, Kinsella CR Jr, Litchfield CR, Nacar A, Lu O, Tubbs RS. The lateral thoracic artery revisited. Surg Radiol Anat 2014;36:543-9.
18. Wei FC, Mardini S. Flaps and Reconstructive Surgery. 1st ed. Philadelphia: Saunders; 2009.
19. Flecknell PA, Roughan JV, Hedenqvist P. Induction of anaesthesia with sevoflurane and isoflurane in the rabbit. Lab Anim 1999;33:41-6.
20. Kushibe K, Tojo T, Sakaguchi H, Takahama M, Nishizaki K, Nezu K, Taniguchi S. Effects of warm ischemia and cryopreservation on cartilage viability of tracheal allografts. Ann Thorac Surg 2000;70:1876-9.
21. Kitamura Y, Shimizu N, Aoe M, Date H, Nagahiro I, Andou A. Allowable warm ischemic time to tracheal extraction for allotransplantation of cryopreserved trachea. Jpn J Thorac Cardiovasc Surg 2004;52:169-74.
22. Ryan S, McNicholas WT, O'Regan RG, Nolan P. Intralaryngeal neuroanatomy of the recurrent laryngeal nerve of the rabbit. J Anat 2003;202:421-30.
23. Delaere PR, Liu ZY, Pauwels P, Feenstra L. Experimental revascularization of airway segments. Laryngoscope 1994;104:736-40.
24. Hardillo JA, Vander Poorten V, Delaere PR. Transplantation of tracheal autografts: is a two-stage procedure necessary? Acta Otorhinolaryngol Belg 2000;54:13-21.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Den Hondt M, Vanaudenaerde BM, Delaere P, Vranckx JJ. Twenty years of experience with the rabbit model, a versatile model for tracheal transplantation research. Plast Aesthet Res 2016;3:223-30. http://dx.doi.org/10.20517/2347-9264.2015.117
AMA Style
Den Hondt M, Vanaudenaerde BM, Delaere P, Vranckx JJ. Twenty years of experience with the rabbit model, a versatile model for tracheal transplantation research. Plastic and Aesthetic Research. 2016; 3: 223-30. http://dx.doi.org/10.20517/2347-9264.2015.117
Chicago/Turabian Style
Den Hondt, Margot, Bart M. Vanaudenaerde, Pierre Delaere, Jan J. Vranckx. 2016. "Twenty years of experience with the rabbit model, a versatile model for tracheal transplantation research" Plastic and Aesthetic Research. 3: 223-30. http://dx.doi.org/10.20517/2347-9264.2015.117
ACS Style
Den Hondt, M.; Vanaudenaerde BM.; Delaere P.; Vranckx JJ. Twenty years of experience with the rabbit model, a versatile model for tracheal transplantation research. Plast. Aesthet. Res. 2016, 3, 223-30. http://dx.doi.org/10.20517/2347-9264.2015.117
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 15 clicks
Cite This Article 15 clicks












Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.